Ruxolitinib
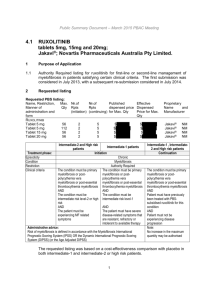
advertisement

JAK inhibitors and low blood cell count Srdan (Serge) Verstovsek M.D., Ph.D. Professor of Medicine Department of Leukemia University of Texas MD Anderson Cancer Center Houston, Texas, USA JAK inhibitor Diseases and studies CEP701 MF: phase II finished and I/II (new formulation) ongoing ET/PV: phase II completed AZD1480 MF: phase I finished, development stopped XL019 MF: phase I finished, development stopped NS-018 MF: phase I ongoing BMS-911543 MF: phase I/II ongoing LY2784544 ET/PV/MF: phase I finished; MF: phase II ongoing CYT387 MF: phase I/II QD completed; phase I/II BID completed; phase III planned SB1518 MF: phase I/IIx2 completed, phase III ongoing SAR302503/TG101348 MF: phase I/II completed; phase II completed, phase III completed; phase II second line ongoing ET/PV: phase II ongoing; PV: phase III planned MF: approved; phase II (low platelets) ongoing INCB018424/Ruxolitinib ET/PV: phase II completed; PV: phase III completed JAK2 Inhibitor Side Effects from Phase II Studies GI X X Anemia Platelets X X X X X Neuropathy X Ruxolitinib vs. Placebo: COMFORT-I Background • Placebo-controlled, randomized, double-blind, phase III study • Ruxolitinib starting doses: – Baseline platelet count 100-200×109/L: 15 mg BID – Baseline platelet count >200×109/L: 20 mg BID • Doses individually titrated based on safety and efficacy • Ruxolitinib treatment significantly reduced spleen size and improved myelofibrosis (MF_-related symptoms and QoL and was also associated with a survival advantage relative to placebo1 Objective • To describe long-term efficacy and safety of ruxolitinib with 1 year of additional follow-up beyond previously published data Data cutoff for current analysis: March 1, 2012. 1. Verstovsek S, et al. N Engl J Med. 2012;366(9):799-807. Verstovsek S, et al. Blood. 2012;120: Abstract 800. Patient Disposition at Current Analysis Ruxolitinib (n = 155) Placebo (n = 151) Placebo Ruxolitinib (n=111) Still on treatment 100 (64.5) 0 73 (65.8) Discontinued 55 (35.5) 40 (26.5) 38 (34.2) Patients, n (%) Crossed over 111 (73.5) Primary reasons for discontinuation Death 13 (8.4) 10 (6.6) 11 (9.9) Adverse event 11 (7.1) 9 (6.0) 7 (6.3) Consent withdrawn 9 (5.8) 6 (4.0) 9 (8.1) Disease progression 12 (7.7) 12 (7.9) 5 (4.5) Other 10 (6.5) 3 (2.0) 5 (4.5) ̶ ̶ 1 (0.9) Noncompliance with study medication • • All patients receiving placebo at the primary analysis crossed over or discontinued within 3 months of the primary analysis Median time to crossover: 41.1 weeks Verstovsek S, et al. Blood. 2012;120: Abstract 800. Incidence of New Onset Grade 3 or 4 Anemia and Thrombocytopenia Over Time Ruxolitinib Grade 4 Placebo Grade 3 Placebo Grade 4 50 Anemia 45 45 40 40 Percentage of Patients Percentage of Patients 50 Ruxolitinib Grade 3 35 30 29.0 25 20 15 10 5 11.5 9.9 2.9 4.1 3.4 Thrombocytopenia 35 30 25 20 15 10 8.7 5.3 4.8 5 1.9 0 0 0 3.4 0.7 0 0 1.6 1.6 1.9 0.9 0 0–<6 6–<12 12–<18 Months 18–<24 ≥24 0–<6 6–<12 12–<18 0 0 18–<24 0 0 ≥24 Months • All patients receiving placebo at the primary analysis crossed over or discontinued within 3 months of the primary analysis; therefore, data for patients receiving placebo is shown for 0–<6 months only Verstovsek S, et al. Blood. 2012;120: Abstract 800. Mean Daily Dose of Ruxolitinib Over Time • Approximately 70% of patients had dose adjustments during the first 12 weeks of therapy • Patients achieved a stable dose with longer-term use Mean Platelet Counts Over Time • Platelet counts remain stable with longer-term therapy Mean Percentage Change From Baseline 10 Ruxolitinib Placebo 0 -10 -20 -30 -40 -50 -60 BL 12 24 36 48 60 72 84 Weeks Median platelet count at baseline: Ruxolitinib, 262.0×109/L; Placebo, 238.0×109/L. 96 Mean Hemoglobin Levels Over Time • Mean hemoglobin nadirs after 8–12 weeks of therapy and recovers to a new steady state which remains stable with longer-term therapy Mean Percentage Change From Baseline 5 Ruxolitinib Placebo 0 -5 -10 -15 -20 BL 12 24 36 48 60 72 84 96 Weeks Median hemoglobin at baseline: Ruxolitinib, 105 g/L; Placebo, 105 g/L Verstovsek S, et al. Blood. 2012;120: Abstract 800. Hemoglobin Levels Over Time in Patients Without Transfusions or Dose Changes No RBC Transfusions and No Dose Changes Before Week 36 No RBC Transfusions Before Week 36 5 Mean Percentage Change From Baseline Mean Percentage Change From Baseline 5 0 -5 -10 -15 -20 BL 4 8 12 16 20 24 28 32 36 Weeks 0 -5 -10 -15 -20 BL 4 8 12 16 20 24 28 Weeks • Recovery in hemoglobin over time was seen regardless of transfusions and dose modifications Analyses were conducted in patients who completed Week 36. 32 36 RBC Transfusions Over Time 50 Percentage of Patients Proportion of patients with RBC transfusion in prior month 40 Ruxolitinib Placebo 72 96 30 20 10 Weighted mean rate of the placebo group = 24.37% 0 BL 12 24 36 48 60 84 108 Weeks From First Ruxolitinib Dose • By Week 36, the proportion of ruxolitinib-treated patients receiving RBC transfusions decreased to the level seen with placebo and remained stable thereafter Hemoglobin Levels Over Time By Ruxolitinib Titrated Dose • Patients titrated to 10 mg BID after nadir hemoglobin showed faster and more complete return of hemoglobin to pretreatment levels Titrated dose is defined as the average dose patients received between Weeks 8 and 56. Hemoglobin levels within 60 days of transfusion are not included. Efficacy by Titrated Dose Total Symptom Score Spleen Volume n=101 n=24 n=26 n=23 n=39 n=21 Week 24 n=103 n=22 n=26 n=23 n=38 n=20 n=35 n=28 Week 48 n=24 n=20 n=31 n=17 Titrated dose is defined as the average dose patients received in the last 4 weeks before assessment. Verstovsek S, et al. Blood. 2012;120: Abstract 800. Development of Anemia Does not Affect Response to Ruxolitinib Treatment Verstovsek S et al. NEJM 2012; 366:799-807. What happens if the therapy with JAK2 inhibitor is interrupted? Number of patients: 34 33 33 34 34 33 33 33 36 37 39 40 40 40 34 29 26 23 24 24 22 22 22 20 21 20 18 17 15 Days Around Dose Change • Return of the symptoms within 7 days Serious Adverse Events After Therapy Interruption Adverse Event Total with interruption, n Total SAEs, n (%) Ruxolitinib (n = 155) Placebo (n = 151) 49 54 3 (6.1) 3 (5.6) • no report of “withdrawal syndrome” • Percent of patients that discontinued ruxolitinib due to side effects was 11% • Percent of patient that discontinued placebo due to side effects was 11% Consideration in everyday practice: addition of an “Anemia Drug” to a JAK2 inhibitor • Danazol • Erythropoietin • Low dose thalidomide Abstract 176 Talpaz M, Paquette R, Afrin L, Hamburg S, Jamieson K, Terebelo H, Ortega G, Lyons RM, Tiu R, Winton E, Natrajan K, Odenike O, Peng W, O’Neill P, Erickson-Viitanen S, Leopold L, Sandor V, Levy R, Kantarjian H, Verstovsek S Distribution of Ruxolitinib Dose Over Time • In patients who completed 24 weeks of treatment, most have optimized their dose of ruxolitinib to 10 mg BID or higher 100% 10 BID 10 / 15 10 BID 15 BID 10 / 15 15 BID 10 / 15 80% 15 BID 5 / 10 10 BID 60% 5 BID 10 AM/15 PM 10 BID 5 / 10 10 BID 10 BID 5 AM/10 PM 40% 5 BID 5 / 10 5 / 10 20% 5 QD 5 BID 5 BID 5 BID 0 5 BID 5 BID 0% Week 4 Week 8 Week 12 Week 16 Week 20 Week 24 n = 41 n = 36 n = 31 n = 28 n = 25 n = 17 n values represent patients with available dose information at the time of data analysis. Data shown for each time point represent the dose that patients were on during the previous 4 weeks. Talpaz M, et al. Blood. 2012;120: Abstract 176. Reductions in Total Symptom Score and Spleen Length Percent Change From Baseline, Mean ±SEM Total Symptom Score 0 -10 -20 n = 41 n = 38 -30 n =35 n = 39 -40 n = 27 n = 31 n = 32 n = 28 n = 28 n = 18 -50 n = 18 n = 24 -60 Weeks TDD, mg Spleen Length Mean Median 4 8 12 16 20 24 10.0 13.2 15.1 16.8 18.3 19.1 10 15 15 20 20 20 Weeks TDD, mg Mean Median 4 8 12 16 20 24 10.0 13.2 15.1 16.8 18.3 19.1 10 15 15 20 20 20 Percent change from baseline is not calculated for patients with a “0” TSS or palpable spleen size of “0 cm” at baseline. Mean and median dose shown for patients with available dosing information. TDD, total daily dose. Talpaz M, et al. Blood. 2012;120: Abstract 176. Change From Qualifying Platelet Count to Nadir and to Week 24 of Individual Patients Qualifying to Week 24 160 160 140 140 Platelet Count (×109/L) Platelet Count. ×109/L Qualifying to Nadir 120 100 80 60 40 120 100 80 60 40 20 20 0 0 Individual Patients Individual Patients Talpaz M, et al. Blood. 2012;120: Abstract 176. THANK YOU sverstov@mdanderson.org