SMILES – Brighton and Hove CCG
advertisement
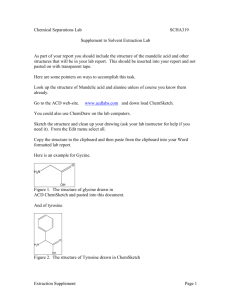
Epidemiology of Mental Health in Brighton and Hove • Population approx 250,000 • High levels of self harm • Consistently in top three suicide rates and drug related deaths in the country • 2480 patients with a diagnosis of psychotic SMILES background to development Reconfiguration of MH services in 2008, with Community Mental Health teams bring divided in to Access and Recovery services This was to incorporate the Recovery and well being agenda and was also in response to the introduction of IAPT Patients who didn’t meet the threshold for Recovery services but still had severe and enduring mental health problem, were increasingly being discharged to primary care Looked at what was happening across the city for QuOF Huge variation in physical health templates – almost all did BMI, BP, Smoking , Alcohol, Lipids. Less good results for side effects, diet, exercise or sexual health Absence of risk screening and recovery planning on annual care plan - only 30% asked about suicide risks No care plans recorded as being given to patient • ..and more detail, • ..and more detail, • ..and more detail until we covered everything. • No nasty surprises! Eligibility for the LES Practice must score 85% for MH9 [annual review including health promotion] Patients 18 + in stable accommodation and registered with a GP participating in the scheme Diagnosis of SMI including schizophrenia, bi polar affective disorder and personality disorder Low risk, or omnipresent and well managed risk. Patient, GP and consultant all in agreement for transfer of care Eligibility for the LES Practice must score 85% for MH9 [annual review including health promotion] Patients 18 + in stable accommodation and registered with a GP participating in the scheme Diagnosis of SMI including schizophrenia, bi polar affective disorder and personality disorder Low risk, or omnipresent and well managed risk. Patient, GP and consultant all in agreement for transfer of care Two tier approach Level two All patients are discharged from secondary care to maintain through put in services Annual care plan and bi annual review with Nurse and GP using standard template Reviewed by Liaison Nurse at least every twelve weeks Referral from primary care to CRHTT if needed Fast track back to recovery if mental health becomes unstable Barriers to usual discharge processes identified in primary care GPs (and sometimes service users) did not understand why patients were being discharged Sometimes not clear plan of care for patient Sometimes no relapse signatures /risk management plan GPs unfamiliar with mental health medication, and apprehensive about responsibility for this patient group Limited resources to support with medication issues and risk management issues Fractured relationships between primary and secondary care The client • • • • • • • 20 year history of psychotic disorder Stable on treatment Insight, motivation, confidence Lives alone in one bed flat, sub let scheme Supportive family Discharged to SMILES Worked with SMILES for 2 years The work we do • Recovery planning • Wellness and Recovery Action Plan • Work and learning, part time work, relationship, needing to move home • Regular meetings with SMILES nurse • 6 monthly supported GP reviews • Physical health monitoring at GP surgery SMILES drop in group, The Recovery Star A closed group for SMILES users once a month Recovery Star Model 10 Ladders of change Each session focuses on a area for change Open and supportive discussion Personal experience of services Rehearsing the plan for difficult times What would we do differently? It was a very detailed spec – to the point that we got a bit lost in it at times! More service user participation and consultation earlier in the process -although this hasn’t been problematic Lots of time spent scoping and initial patient lists soon became defunct in terms of suitability Ways forwards Physical health template now universally available for all GP IT systems and recommended by CCG for standard QuOF template for all practices Planning to pilot and introduce Clozapine monitoring as part of shared care agreement under LES. Opened Clinical Network Mettings to all practices and invited staff form Recovery Looking to include more practices Ways forward May consider skill mix/peer support if we grow the project Broadening the eligibility by diagnosis/referral route Considerations about how to support clients in practices that don’t want to get involved, ?Shared care arrangement for patients on depots who are still under secondary care