Identifying and Referring
Patients with Suspected Cancer
Dr Nick Pendleton
NICE Clinical Knowledge
Summaries (CKS)
• Cancer – suspected (NICE referral advice)
http://cks.nice.org.uk/#specialityTabnt
Referral timelines
• Immediate: an acute admission or referral
occurring within a few hours, or even more
quickly if necessary
• Urgent: the patient is seen within the
national target for urgent referrals
(currently 2 weeks)
• Non-urgent: all other referrals
About this presentation:
• The scenarios in this slide presention are
based wholly or partly on real patients who
have presented to GP surgeries. They have
been anonymised for use as a teaching tool
for GPs in Training. For realism the patients
have been given fictional names, ages and
professions.
Lesley Summers - 31
• Whilst I’m here can you check this
mole on my arm?
A B C D E Rule
ASYMMETRY
IRREGULAR BORDER
COLOUR – gaining, losing , multiple colours
Diameter greater than 6mm (1/4 inch)
Evolving
(?)
Mr Simpson 53, Company Director
• « I try and stay away from Doctors if I can
but my wife has made this appointment! »
• « What is your wife worried about!? »
• « I have this lump on my leg… Its getting a
bit bigger and its quite sore »
Can I ask you some questions about it?
• « How long has it been there? »
• « About 3 months or so »
• « Is there any history of an injury? »
• « Yes, come to think about it, I knocked my
leg with an axe whilst chopping logs about 4
months ago »
What are the worrying features of
a palpable lump?
• Refer urgently as suspected soft tissue
sarcoma if:
•
•
•
•
•
•
Greater than about 5 cm in diameter
Deep to fascia, fixed or immobile
Painful
Increasing in size
A recurrence after previous excision
If there is any doubt about the need for referral,
discussion with a local specialist should be
undertaken
Mr Simpson was referred (2WW)
• CT showed an homogenous mass with capsule
formation. US scan appearances resembled a
multi-locular cyst. The mass was excised.
• Histology – necrotic debris, fibrin and blood
clots.
• Fortunately it was not a Sarcoma.
• “A case of chronic expanding hematoma in the
tensor fascia lata”
• http://escholarship.org/uc/item/6wg5260x
Ricky, 15
« Coach said I should come and see
you about my left leg –It’s
interfering with my training. I play a
lot of sport including football 3
times a week »
Tell me more about it..
• I don’t remember injuring it, but I’ve not
been able to run on it for a few weeks now
• It is sore and tender to press on
• It hurts even when I’m not walking about
• It’s more sore this week than a few weeks
ago
• On examination: he’s limping, there is a
bony and tender swelling below the knee
What is the Differential Diagnosis?
• Osgood-Schlatter’s Disease?
• A Primary Bone Tumour?
• Osteosarcoma most commonly presents
between 10 and 24 years old
• This is an age when a lot of people take
part in sports
What should you do next?
• Patients with increasing, unexplained or
persistent bone pain or tenderness,
particularly pain at rest (and especially if
not in the joint), or an unexplained limp
should be investigated urgently ?Bone
Tumour
• CKS Guidance recommends an immediate
Xray and then if bone tumour is a
possibility – refer urgently (2WW)
OSTEOSARCOMA (MALIGNANT BONE TUMOUR)
Mr Jones, 46, Salesman
• Blood results done as part of health screen:
LFTs
• ALP slightly raised 25% above normal
• ALT raised 50% above normal
• Other bloods and LFTs normal
• Not on any medications, PMH nil, non-smoker
Review appointment
• Alcohol intake 60 -70 units a week
• ‘Don’t worry I will curb my drinking
doctor – its just become a habit to
open a bottle of wine after work with
my wife’
• Plan: recheck LFTs in 4-6 weeks (NB. the
guidance says 6 months)
Review appointment 2
• Alcohol intake 20 units a week
• ‘We have also started healthy eating
and exercising doctor!
• LFT results: ALT still raised 50% above
normal, ALP slightly better but still close to
25% above normal
Ultrasound Report
• There is a hyperechoic mass with
in one lobe of the liver. It is
not possible to say whether this
is a benign cyst or a sinister
lesion. Referral for urgent MRI is
indicated.
Telephone Encounter
• Hello Mr Jones – I am ringing about your
Ultrasound report, is now a good time to talk?
• No, sorry Doctor – we have just had a telephone
call to say my mother has passed away in the
nursing home. I don’t want to discuss anything at
the moment. I’ll come and see you at the surgery
soon. Goodbye.
• What do you do next?
Mrs Gladys Parker, 72
• Dysphagia and weight loss. Gastroscopy 1
month ago normal.
• Came with daughter. My mum is still losing
weight and can’t swallow properly. The
Doctor we saw last week gave her some
ensure drinks but something’s not right!
Re-referral for gastroscopy
Report: There is a
circumferential stricture
seen with the appearances
of an advanced oesophageal
carcinoma…
The patient died 4 weeks later
Letter to Endoscopy Unit
Dear Sister X
I would like to enquire whether it
is possible for a tumour of this
advanced stage to appear with in
this short time scale and do you
have any video footage of the
previous exam?
Response from GI Consultant
Thank you for your letter. No I do
not think this lesion could have
arisen in this short time scale. I
think it was missed during the
first examination. We will be
exploring this with the
endoscopist. We do not currently
video the examinations.
Mr Schonberg, 66
A Cutaneous Horn – 25% will have
SCC at the base
Mr Chandra, 46, IT Developer
• I have been passing blood from my back
passage every time I go to the toilet for the
last 3 days
• No change in bowel habit
• Its bright red
• Its after a motion
• It’s not painful
Examination
• Abdomen examination normal,
no mass
• PR examination normal
• What would you do next?
WHAT DOES THE CKS GUIDANCE SAY?
• In patients 40 years of age and older, reporting
rectal bleeding with a change of bowel habit
towards looser stools and/or increased stool
frequency persisting for 6 weeks or more, an
urgent referral should be made.
• In patients 60 years of age and older, with rectal
bleeding persisting for 6 weeks or more without a
change in bowel habit and without anal
symptoms, an urgent referral should be made .
Mr Chandra, 46, IT Developer
• I have been passing blood from my back
passage every time I go to the toilet for the
last 3 days
• No change in bowel habit
• Its bright red.
• Its after a motion
• It’s not painful
WHAT DOES THE CKS GUIDANCE SAY?
• In patients with equivocal symptoms who
are not unduly anxious, it is reasonable to
use a period of 'treat, watch and wait' as a
method of management
• In men of any age with unexplained iron
deficiency anaemia and a haemoglobin of
11 g/100 mL or below, an urgent referral
should be made
Timothy, 6 years old
• He’s got a lump on his neck! Its getting
bigger
•
•
•
•
3 cm lymph node in posterior triangle
Hard and irregular in shape
Recent URTI/sore throat
Pallor
Causes of Neck Swelling in Children
LYMPHADENOPATHY (enlarged lymph nodes)
• LOCAL
• SYSTEMIC
LYMPHADENITIS (inflamed lymph nodes) or
ABSCESS
NON-LYMPHADENOMATOUS NECK
SWELLINGS
BMJ 2012;344:e3171
LYMPHADENOPATHY (enlarged lymph nodes)
• LOCAL
•
•
•
•
Viral or bacterial upper respiratory tract
Ear infection, Oropharyngeal infection
Headlice infestation, Dental abscess
Cat scratch disease (gram –ve bacteria Bartonella Henselae or
Quintana)
• SYSTEMIC
•
•
•
•
•
•
Malignancy (lymphoma or leukaemia)
Viral infections (Epstein-Barr virus, cytomegalovirus, rubella)
Kawasaki disease
Mycobacterial infection (tuberculous or non-tuberculous),
Sarcoidosis
Systemic lupus erythematosus
Juvenile idiopathic arthritis
BMJ 2012;344:e3171
Lymphadenitis (inflamed lymph
nodes) or abscess
• Bacterial lymphadenitis
• Mycobacterial lymphadenitis
• Abscess
BMJ 2012;344:e3171
Non-lymphadenomatous
neck swellings
•
•
•
•
•
•
•
Cystic hygroma
Sternocleidomastoid swelling
Thyroid gland enlargement
Thyroglossal cyst
Dermoid cyst
Branchial cyst
Mumps
BMJ 2012;344:e3171
Features of High Risk Neck Lumps
in Children
• Non-tender, firm or hard lymph nodes
• Progressively enlarging
• Lymph nodes in the supraclavicular area or
axillary area
• Lymph nodes > 3 cm in size
• Lymph nodes in children with a history of
malignancy
• Hepatosplenomegaly, Fever, Weight Loss
• Night Sweats
Clinical Otolaryngology, 31, 433 – 434
and GP Notebook (lymphadenopathy)
Timothy, 6 years old
•
•
•
•
He’s got a lump on his neck!
3 cm lymph node in posterior triangle
Hard and irregular in shape
Recent URTI/sore throat, Pallor
• Clearly fits urgent referral criteria for a
suspicious neck lump
Mrs Sullivan, 50, unemployed
• I’ve got this ringing in my left ear!
• I can’t hear as well either
• I sometimes have a spinning sensation in my
head
“IN MY RIGHT EAR”
“IN FRONT”
Rinne both ears
AC>BC
Weber without
lateralization
Weber lateralizes left
Weber lateralizes
right
Normal/bilateral
sensorineural loss
Sensorineural loss in Sensorineural loss in
right
left
Combined loss :
conductive and
sensorineural loss in
left
Rinne left BC>AC
Conductive loss in
left
Rinne right BC>AC
Combined loss :
conductive and
Conductive loss in
sensorineural loss in right
right
Rinne both ears
BC>AC
Conductive loss in
both ears
Combined loss in
Combined loss in left
right and conductive and conductive loss
loss on left
on right
AC = Air Conduction BC = Bone Conduction
Mr Sullivan, 50, unemployed
• I’ve got this ringing in my left ear!
• I can’t hear as well either
• I sometimes have a spinning sensation in my
head
• Examination: sensorineural hearing loss
• Diagnosis – small acoustic neuroma (tumour of
vestibulocochlear nerve)
A Large Acoustic Neuroma
Can cause these additional symptoms:
• headaches with blurred vision
• numbness or pain on one side of the face
• problems with limb coordination on one side of
the body
• less often, muscle weakness on one side of the
face
• in rare cases, changes to the voice or difficulty
swallowing
Mrs Simpson, 52
« I am fed up with this, just look at
my belly its massive, I feel bloated,
but I’ve got no appetite and when I
do eat I’ve either got diarrhoea or
can’t go at all. Also I keep having to
urinate, I feel tired and my back
hurts! »
OVARIAN CANCER
VERSUS
IRRITABLE BOWEL SYNDROME
IRRITABLE BOWEL SYNDROME
OVARIAN CANCER
Bloating
Bloating
Abdominal Pain
Pelvic or Abdominal Pain
Nausea/ Poor Appetite/Feeling Full/
Flatus/Belching
Trouble Eating or Feeling Too Full
Quickly
Constipation and/or Diarrhoea
Constipation
Urinary Symptoms eg. frequency
Urinary Symptoms eg. frequency
Fatigue
Fatigue
Upset Stomach/Heartburn
Upset Stomach
Back Pain
Back Pain
Abdominal Swelling (with Weight Loss?)
Abdominal Swelling with Weight Loss
Muscle pains
Pain During Sex
Menstrual Changes
It is uncommon for IBS to first develop in women over the age of 50
Investigating Ovarian Cancer
Symptoms in Primary Care
• Measure serum CA125 in primary care in women
with symptoms that suggest ovarian cancer
• If serum CA125 is 35 IU/ml or greater, arrange an
ultrasound scan of the abdomen and pelvis
• For any woman who has normal serum CA125 (less than 35
IU/ml), or CA125 of 35 IU/ml or greater but a normal
ultrasound: assess her carefully for other clinical causes of
her symptoms and investigate if appropriate
NICE CG 122 - OVARIAN CANCER
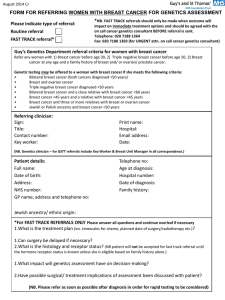
Sally Smith, 39, Secretary
« My Sister is 45 and having
treatment for breast cancer and
I want to know if I am at risk »
« My Aunt died from Ovarian
cancer 2 years ago »
What is a Significant Family History?
• One first-degree female relative diagnosed with breast cancer at
younger than age 40 years
• One first-degree male relative diagnosed with breast cancer at
any age
• One first-degree relative with bilateral breast cancer where the
first primary was diagnosed at younger than age 50 years
• Two first-degree relatives, or one first-degree and one seconddegree relative, diagnosed with breast cancer at any age
• One first-degree or second-degree relative diagnosed with
breast cancer at any age and one first-degree or second-degree
relative diagnosed with ovarian cancer at any age (one of these
should be a first-degree relative)
• Three first-degree or second-degree relatives diagnosed with
breast cancer at any age
http://www.patient.co.uk/doctor/familial-breast-cancer
Alternative Scenario
• Mother had breast cancer aged 50. No other
family history.
• Offer information and reassurance, secondary care
referral not indicated unless the family history
contains:
•
•
•
•
•
•
Bilateral breast cancer, Male breast cancer
Ovarian cancer, Jewish ancestry
Sarcoma in a relative younger than age 45 years
Glioma or childhood adrenal cortical carcinomas
Complicated patterns of multiple cancers at a young age
Paternal history of breast cancer (two or more relatives on the father's side
of the family)
http://www.patient.co.uk/doctor/familial-breast-cancer
Mr Jenkinson 71
• Telephone call: « I cannot tolerate this
shoulder pain any longer. Surely I need
an X-ray or something. The Drs have
said there would be no point as it would
just confirm arthritis, but it is getting
worse and my arm is loosing muscle and
strength! »
• XRAY request: 6 months of right
shoulder pain now needing morphine
PANCOAST TUMOUR AT RIGHT APEX
Summary of the Session
•
•
•
•
•
•
•
•
•
•
•
•
A Mole – Possible Malignant Melanoma
Lump on the Leg – Possible Sarcoma
Leg Pain – Osteosarcoma or Osgood-Schlatter’s
Abnormal LFTs – ?Hepatocellular Carcinoma
Dysphagia with normal gastroscopy – Oesophageal Tumour
Cutaneous Horn – SCC
Rectal Bleeding - Referral Guidance
Neck Lumps in Children
Tinnitus and Hearing Loss – Acoustic Neuroma
IBS versus Ovarian Cancer
Breast cancer - Family History
Shoulder Pain - Lung Cancer (Pancoast Tumour)
Identifying and Referring
Patients with Suspected Cancer
CLINICAL RECORD REVIEW
Tony Frazer 36, National Account
Manager (Sales)
• July 2013
• Dr A on-call
• Telephone triage encounter:
• Haematemesis fresh and dried (coffee
bean) blood
• Abnormal weight loss, 3 stone in 7/12
Same day appointment with Dr B
• Heamatemesis after drinking
excessive alcohol and vomiting
• 2 stone weight loss in 7 months
• Exam normal, weight 65kg (75kg Sept 12)
• Needs 2WW referral, upper GI poss
mallory weiss tear but in
combination with weight loss need
to r/o malignancy.
14 August – Dr C
•
•
•
•
•
Gastroscopy normal, h.pylori -ve
Very tired
Intermittent diarrhoea
No appetite, weight 63kg
Mood OK – but a lot of stress in last year
• Blood tests requested to exclude coeliac
• Start omeprazole 20mg bd
Dr C – 22 August
• Omeprazole caused dizziness
• TTG IgA test – normal
• c/o No appetite, mood ‘ok’, loss of
concentration, memory disturbance,
stressful life events
• Not open to possible depression
• Wanted to go private – GI consultant
2nd October
• Continues to lose weight - wt 59Kg
• Consuming 2000 calories in food from
McDonalds and 2500 calories in supplements
• Upper GI consultant suggested the cause of
his weight loss is depression and suggested
starting him on mirtazapine (and arranges CT)
• Patient thinks this is wrong as he has a great
life and everything to feel good about.
Weight Chart
25 September – Dr D
• CT scan was normal
• Now feels too weak and tired to work
• Weight stable
• Feels frustrated and down in mood
• TATT, sleeping lots, buying own high
calorie supplements
• Awaiting further GI consultant review.
See in 3 weeks
25 November – Dr C
• Gaining weight
• Taking mirtazapine
• Has seen consultant again who suggests
Chronic Fatigue Syndrome (CFS) is the
possible diagnosis
• Referred CFS Specialist for opinion
• In the meantime wants to try hydrotherapy
to get some fitness back
Weight Chart
7 February 2014
• Diagnosis of CFS confirmed by
specialist
• 16 September 2014 – making
progress with CFS therapy and a
return to work is possible in early
2015
About this presentation:
• The scenarios in this slide presention are
based wholly or partly on real patients who
have presented to GP surgeries. They have
been anonymised for use as a teaching tool
for GPs in Training. For realism the patients
have been given fictional names, ages and
professions.