FFF Workshop 27.03.14 Nottingham PL
advertisement

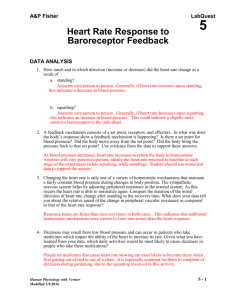
Guide to Action to Prevent Falls (GTA) Community version – in use Care Home version – under evaluation Dementia version – in development Robertson K, Logan P, Conroy S, Dods V, Gordon A, Challands L, et al. Thinking Falls- Taking Action: development of a Guide to Action for Falls Prevention British Journal of Community Nursing 2010;15(8):406 - 410. Robertson K, Logan P, Ward M, Pollard J, Gordon A, Williams W, Watson J. Thinking falls-taking action: a falls prevention tool for care homes.Br J Community Nurs. 2012 May;17(5):206-9 Logan, PA; Coupland, CAC; Gladman, JRF, et al Community falls prevention for people who call an emergency ambulance after a fall: randomised controlled trial. . British Medical Journal 2010; 340 c2102 Professor Pip Logan Division of Rehabilitation & Ageing University of Nottingham Developing the GTA Group of clinicians, social services, fire service, local authorities, older people, commissioners, researchers 2008- to date Incorporates clinical guidelines, research findings, clinical expertise Checklist outlining 37 risk factors and recommended interventions Training by falls specialists: Two hours, groups 4-8, interactive session Intervention manual, GTA forms, falls incident record sheet √ √ √ √ FALLS HISTORY MEDICAL HISTORY MOVEMENT & ENVIRONMENT PERSONAL History of Falls History of falls prior to admission to the care home Falls reason for admission to care home Medical history Stroke, Parkinson’s Disease, dementia, epilepsy, blackouts, diabetes, short of breath, heart disease, arthritis, high / low blood pressure Medication On 4 or more medications, on sedatives, antidepressants, diuretics Transfers Needs help on/off chair, bed, toilet Unsteady when transferring, tends to rush Nutrition Needs encouragement to eat Poor appetite, Recent weight loss Balance Holds furniture when moving, unsteady when walking, loses balance on turning, cannot walk unsupported due to unsteadiness Stumbles or trips Noted to stumble / trip even if no obstacle, near misses noted Continence Incontinent of urine / faeces, toilet difficult to access, frequency, urgency, gets up at night to use toilet/commode, concerned about continence / getting to toilet in time, difficulty managing clothes, catheter, constipation Fluid Drinks less than 5 cups of fluid a day, needs encouragement to drink, often leaves drinks History of Falls History of falls since admission Recent Falls 2 or more falls in the past 6 months (A fall is defined as inadvertently coming to rest on the ground or at a lower level, including slipping from side of bed) Dizziness Complains of dizziness, dizzy on first standing up Fractures Has broken bones as result of fall: Wrist, hip, humerus, pelvis, spine, ribs, collar bone, shoulder, ankle Cognition Does not recognise own limitations, poor understanding of space and distance, unaware of hazards , poor short term memory Gait Shuffles, leans to side, leans backwards, walks fast Walking Needs supervision when walking, needs assistance of 1 or 2 to walk Hospital admission Attended A&E due to fall, Ambulance called - not taken to hospital ,admitted to hospital due to fall Behaviour Agitated, unsettled, anxious, periods of aggression, risk to others Walking aids Uses incorrectly, refuses to use, forgets to use, poor condition Sleep Unsettled at night, sleeps a lot during the day, feels tired Other injury due to falls Head injury, cuts, bruises, skin tears Comprehension Has difficulty understanding verbal instructions / questions Heating / body temperature Feels cold, sits for long periods at a time, doesn’t recognise when cold Vision Has diagnosed sight loss, wears varifocal / bifocal glasses refuses to wear glasses Coping strategies Inability to get up or summon help Mood Low mood, depression. anxiety, fearful Alarm Unable to reach alarm, forgets to use, does not call for assistance Fear of Falling Is anxious / worried about falling, lacks confidence, remains seated for much of day due to fear of falling Communication Unable to express needs verbally, unable to make self understood, difficulty making self understood clearly Flooring Rugs, clutter, flexes, Floor coverings, spillages Lighting Poor lighting day and/or night, location of light switches Footwear Unsupportive footwear, footwear too loose / tight, painful feet Pain Has specific / general pain, pain not helped by pain killers, on meds for pain that cause side effects e.g. constipation, dizziness, unable to communicate in pain FALLS HISTORY √ MEDICAL HISTORY √ MOVEMENT & ENVIRONMENT √ √ PERSONAL History of Falls Review all incidents using Incident Analysis Form, look for any patterns to falls e.g. time of day, activity at time of fall, inform GP of falls history / recent falls Postural blood pressure to be checked in lying, sitting and standing - alert GP if drop of more than 20mmHg, Request medical review to identify any medical causes of falls e.g. infection, stroke, low blood pressure, heart problems Identify any possible causes of falls and take steps to reduce those risks Medical history Check for signs of acute illness / infection, consider medical review from GP if condition not been reviewed in last 6 months, if low blood pressure prompt to stand still on 1st standing up Transfers Consider use of alternative furniture, refer to OT for advice if required Nutrition Encourage to eat small amounts regularly, ensure teeth well fitted, review reasons for poor appetite and weight loss - refer to GP, dietician Medication Medication should be reviewed by GP every 6 mths, consider side effects of meds i.e. dizziness, sedation, confusion. and refer to GP if concerned Balance Encourage to stand still on first standing Advise to keep head and feet in line when turning, increase supervision, consider referral to physiotherapist Dizziness Postural blood pressure to be checked in lying, sitting and standing - alert GP if drop of more than 20mmHg, Advise to move legs and feet before standing and to stand still and count to 10 on first standing up Stumbles or trips Document incidents, review incidents for time, location, activity at time. Review possible causes e.g. footwear, eyesight Continence Ensure continence assessment completed, refer to comm. nurse or continence service, test urine, assess for constipation, consider signage to toilet, refer to OT if required, consider commode for night use, check regularly if requires toilet Fractures At risk of osteoporosis, Ask GP to review if person is falling and has had previous fracture(s) Cognition Refer to GP if not reviewed in last 6 mths, use signage for toilet, bedroom, lounge, use physical gestures and prompts, Repeat information when person unable to remember, inc super Gait Prompt to lift feet, stand upright, refer physio Hospital admission Review causes of fall, initiate any treatment recommended, inform GP Behaviour Refer to GP if medical review required, Mental Health services, Ensure no acute illness or infection, be aware of risk of introducing / increasing psychotropic medication Walking aids Check correct height, check ferrules, prompt to use correctly Sleep Encourage activity during the day, consider time goes to bed, be aware of risk of medication to aid sleep increasing risk of falls, increase night supervision, consider use of sensor mats Other injury due to falls Review causes of fall, initiate any treatment recommended, inform GP Comprehension Speak clearly, in short sentences, with simple instructions, use physical gestures and prompts Heating / body temperature Ensure draft free environment, consider temperature if person sitting for long periods, mobilise regularly Vision Ensure access to regular sight checks (every 2 yrs), ensure adequate lighting day and night, advise against bifocal glasses Coping strategies Ensure call buzzer easily accessible and working Consider use of sensor equipment Increase level of supervision and document Mood Reassure, encourage socialisation, Be aware of risk of introducing / increasing psychotropic medation Alarm Ensure able to access alarm call system in rooms, consider use of sensor equipment, increase supervision Footwear Advise on suitable footwear, check footcare, - nails, corns, callouses, refer to podiatry Fear of Falling Consider reasons for fear of falling, increase supervision, ensure mobility maintained, encourage and reassure Communication Consider alternative communication methods, physical gestures, observe behaviour and routines for insight into how the person may be feeling Flooring Ensure floor free from clutter, rugs and flexes, avoid patterned flooring, avoid thresholds, keep floors dry at all times Pain Refer to GP if pain poorly controlled, review medication if side effects to prescribed tablets, observe behaviour and facial expression for signs of pain if unable to communicate Walking Refer to Physiotherapist, assist in completing exercise programme prescribed Lighting Ensure good lighting with no glare, consider use of night light, ensure switches accessible Fluid Encourage to drink 6-8 cups of fluid a day, stay with person whilst having a drink, document poor fluid intake if does not finish drinks, review reasons for poor fluid intake eg worried about getting to toilet Feasibility testing of the GtACH • 20 minutes versus 2 hours for non-training completers. • 26 residents were assessed • 179 risk fall factors were identified • 163 recommended interventions were recorded • 86 (53%) of these interventions were completed and recorded in the care plan. • 9/11 participants with abnormal blood pressure received treatment to rectify. • 7/8 participants who were having difficulties alerting staff when needing help, received a better placed buzzer and sensory alarm mats placed next to the bed. • 5/10 incontinent participants were given a management plan or referred to the continence service or district nurse To estimate important parameters that are needed to design the main study. To test the feasibility of completing an RCT to evaluate a falls prevention intervention (GtACH) in care homes. To determine whether to proceed with a large trial To decide the best approach to adopt for the design of the definitive trial Future directions Evaluate GTA ? Implement GTA ? Lots of interest Already used locally Thank you Pip.logan@nottingham.ac.uk