Falls Workshop_Frances Healy Presentation_Part 1
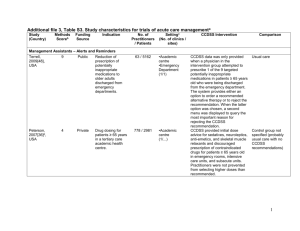
advertisement

Implementing the FallSafe bundle Dr Frances Healey, RGN, RMN, PhD Associate Director for Patient Safety, NHS England (past) Associate Director, Clinical Effectiveness and Evaluation Unit, RCP Plan • My brief: share the experience of piloting in England, how it was approached , what was successful, what the challenges were • Time for sharing thoughts, questions and answers FallSafe Quality Improvement Project Led by the Royal College of Physicians Funded by the Health Foundation Supported & promoted by: FallSafe: The Project “Can a ward-based nurse influence all disciplines to embed evidence-based falls prevention care bundles into regular ward practice using a quality improvement approach?” • Original project: 16 sites, variety of specialities • Extended evaluation (9 sites + 9 controls) awaiting publication • Formally assessed rapid spread at Portsmouth • Informal spread in a range of hospitals Headline results: original project • • • • • • Patients without a call bell in reach reduced by 78% Twice as many requests for medication review Patients without safe footwear reduced by 67% Twice as many patients had their L&S BP checked 56% more patients assessed for confusion Twice as many patients asked if they were worried they might fall • 41% decrease in patients given night sedation 60% certain last fall was reported 77% certain last fall was reported Reported falls rate per 1000 bed days + rolling 12 month average Reported injurious falls rate per 1000 bed days + rolling 12 month average Falls rate ratio 12 months before full bundle v.12 months after 0.75 (0.68-0.84), p<0.001 Injurious falls rate ratio 12 months before full bundle v.12 months after 0.86 (0.71-1.03), P=0.11 http://www.rcplondon.ac.uk/resources/falls-prevention-resources http://www.rcplondon.ac.uk/projects/fallsafe What was different about the FallSafe approach? 1. It was evidence-based Multi-factorial assessment and intervention reduces falls rates by 20%-30% Reference NICE 2013 Title Details Falls in older people clinical guideline update Appendix E Evidence tables http://www.nice.org.uk/guidance/in dex.jsp?action=download&o=62252 Myakie-Lye et al. 2013 Inpatient Fall Prevention Programs as a Patient Safety Strategy: A Systematic Review http://annals.org/article.aspx?articl eid=1656443 Cameron et al. 2012 Interventions for preventing falls in older people in care facilities and hospitals. doi: 10.1002/14651858.CD005465.pub3 DiBardio et al. 2012 Meta-analysis: multidisciplinary fall prevention strategies in the acute care inpatient population J Hosp Med. 2012;7:497-503 Spoelstra et al. 2012 Falls prevention in hospitals: an integrative review Clin Nursing research 21 (1) 92-112 Oliver et al. 2010 Preventing falls and fall-related injuries in hospitals (narrative update of Oliver et al. 2007) Clin Geriatr Med. 2010;26:645-9 Oliver et al. 2007 Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and metaanalyses. BMJ. 2007;334:82 Coussement et al. 2008 Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:29-36 m ul > ti-p fiv ro e fes co s i po mp on st o n a l -fa e l n t m oile l re ts ed ti vi i c ng ew at p st ion lan af re s f ur ed vie i n uc w e sc atio en ree n vi nin ro g nu n m er fo me ic o nt al t w ris ea k r sc e hi x ore p er pr ci ot se e w cto ris rs tb an pa b ala d tie es rm nt ide s in s fo ig rm n at io n perecentage of trials significant reductions in falls no significant reductions in falls 100 90 80 70 60 50 40 30 20 10 0 Oliver D, Healey F, Haines T (2010) Preventing falls and falls related injuries in hospital Clinics in Geriatric Medicine (26 4 645-692) “Having been doing this [nursing] for 30 years it’s the first time ‘evidence based’ meant anything to me. I was evidence based and proud of it!” Multifactorial assessment may include: • cognitive impairment • continence problems • falls history (causes, consequences, & fear of falling) • footwear that is unsuitable or missing • health problems that affect falls risk • medication • postural instability, mobility and/or balance problems • syncope syndrome • visual impairment “Ensure that any multifactorial intervention: Multifactorial intervention – promptly addresses the patient’s individual risk factors – takes into account whether the risk factors can be treated, improved or managed during the patient’s expected stay Do not offer falls prevention interventions that are not tailored to address the patient’s individual risk factors for falling.” 1 6 FallSafe: The care bundle 1) For all patients • Ask on admission about history of falls and fear of falling • Urinalysis on admission (just one element of underlying illness adding to falls risk) • Avoid new night sedation • Ensure call bell in reach • Ensure appropriate footwear available and in use • Bedrails: assessment of risks and benefits FallSafe: The care bundle 2) ‘high risk’ patients (all patients on FallSafe wards for older people) • Cognitive assessment (AMTS or MMSE) • Test for delirium if cognitively impaired (as per NICE guidelines on delirium) • Visual assessment: recognising objects from end of bed • Lying and standing blood pressure using manual sphygmomanometer (as part of syncope identification) • Nurse to request medication review by medical staff according to agreed guidelines • Toileting assessment and plan “Do not use fall risk prediction tools to predict inpatients’ risk of falling in Predicting patients’ hospital”risk of falling in hospital 2 0 “Regard all inpatients aged 65 years or older as being at risk of falling in hospital” + inpatients aged 50 to 64 years (if clinical judgement that underlying condition could cause falls) i.e. now recommend one bundle for all aged 65 years+ Falls risk assessment falls risk prediction scores modifiable risk factor checklists What was different about the FallSafe approach? 1. It was evidence-based 2. It prioritised the things we struggle with http://www.rcplondon.ac.uk/projects/national-auditfalls-and-bone-health-older-people National pilot audit All older patients: • 11% not asked about history of falls • 10% could use a call bell but did not have one in reach • 9% used a mobility aid but had their mobility aid out of reach • 6% had no safe footwear Even for super-high risk patients (fallers): • 23% did not have medication reviewed • 46% did not have L&S BP checked • 18% no cognitive screening High levels of dementia and delirium in inpatient fallers 88% had mobility problems 65% were cognitively impaired 65% had bone health problems 58% had continence problems/urgency 49% culprit medication 42% had orthostatic BP/cardiovascular 37% impaired vision 36% had delirium Royal College of Physicians 2012 Clinical Effectiveness and Evaluation Unit Report of the 2011 inpatient falls pilot audit www.rcplondon.ac.uk based on case note review of 447 patients in 46 hospitals who fell in September 2011 – data drawn from those where assessment was not omitted, so potentially skewed Risk factors for falling in hospital Hospital inpatients Odds Ratio (95% CI) History of falls 2.85 (1.14–7.15) Sedatives 1.89 (1.37–2.60) Antidepressants (yes vs. no) 1.98 (1.00–3.94) Cognitive impairment 1.52 (1.18–1.94) Age (for 5 years increase) 1.04 (1.01–1.06) Deandra S, Bravi F, Lucenteforte E et al. Risk factors for falls in older people in nursing homes and hospitals; a systematic review and meta-analysis Arch Gerontol Geriatr 56 (2013) 407–415 Risk factors for being injured in a fall in hospital Hospital inpatients Odds Ratio (95% CI) SRRIs (yes vs. no) 1.84 (1.04-2.67) 2+ antipsychotic 3.26 (1.20-8.90) Opiate 1.59 (1.14-2.20) Diuretic 1.53 (1.03-2.26) Mion et al. Is it possible to identify risks for injurious falls in hospitalized patients? Jt Comm J Qual Patient Saf; 2012 Sep;38(9):408-13 Baseline Project end Six months later 1 Call Bell in reach 91% 98% 99% 2 Cognitive screen 50% 78% 63% 3 Asked about fear of falling 29% 68% 71% 4 History of falls taken 81% 89% 96% 5 Lying Standing BP 25% 50% 43% 6 Medication review 42% 84% 72% 7 Night sedation not given 82% 87% 90% 8 Safe footwear on feet 91% 97% 99% 9 Urine dip-test 63% 78% 82% What was different about the FallSafe approach? 1. It was evidence-based 2. It prioritised the things we struggle with 3. It was multidisciplinary