Dr. Vincent Cheung - Managing Complications of Therapy in CKD
advertisement

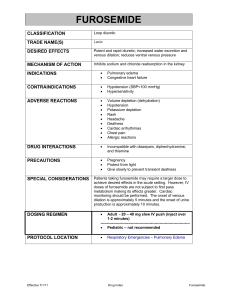
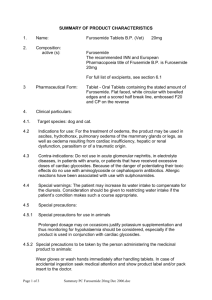
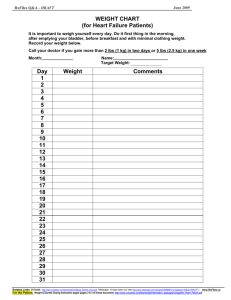
Managing complications of therapy in CKD Dr. Vincent Cheung The Diabetes and Nephrology Symposium November 19th, 2014 Disclosure • Faculty: Dr. Vincent Cheung • Relationships with commercial interests: – Advisory Board Honoraria: • Takeda • Astra Zeneca – Speakers Honoraria: • Servier Canada • Canadian Heart Research Centre Disclosure of Commercial Support • This program may receive financial support from Servier Canada in the form of an honorarium. • Servier Canada products are not specifically discussed in this program. 3 Diabetes and renal care Outline • Too wet too dry • K+ Too high too low • Hyperuricemia/Gout Too wet too dry “Bruce”, a diabetorenocardiopath Bruce • • • • 73 years old Type diabetes for 10 years MI, PCI 3 years ago Meds: Ramipril 10 mg od Amlodipine 10 mg od Metformin 500 mg tid Saxagliptin 2.5 mg od ASA 81 mg od Bruce • Good diabetic control • Recent cardiac testing – echo moderate systolic dysfunction, no ischemia • Presents with SOB, orthopnea, leg swelling, weight gain of 15 lbs Bruce • • • • Furosemide 40 mg po od 2 days later no better Furosemide increased to 80 mg od Excellent urine output, feeling better after 4 days • 3 weeks later, after weekend trip, Furosemide “didn’t work”, weight up 12 lbs in 2 days • Furosemide increased to 120 mg bid Bruce • Excellent urine output, weight back down after 4 days • Furosemide reduced to 120 mg od • 1 week later, diarrhea, weak, almost fainted • Seen in ER. Felt to be “dry”, Cr 244 • Furosemide, ramipril and metformin stopped, IV fluid given, Cr down to 190 • Sent home within 24 hours Bruce • Feeling stronger, improved appetite • Restarted on Furosemide 40 mg bid • 3 days later back to ER with 14 lb weight gain, SOB Why is Bruce so unstable? 40 mg 120 mg bid 80 mg 190 185 180 120 mg Weight in lbs 175 170 165 40 mg bid 160 155 Stopped 150 145 140 0 10 20 30 Days 40 Diabeto-renal concepts Glycemic instability Pushes glucose down • Reduced intake • Insulin/sulfonylurea • Exercise • BB, quinolones • EtOH Too high Serum Glucose Pushes glucose up • Increased intake • Insufficient insulin • Inactivity • Steroid, Thiazide Too low Why is volume so unstable and what can we do about it? • • • • • • • • Diet? Na+ restriction/dietary routine Ischemia? Cardiac optimization A Fib? Rate control NSAIDs/COX-2 inhibitors Avoid Other Na+ retaining meds – steroids, glitazones Dehydration? Sick Day Med Advice Cardiac Output variation with volume status Diuretic resistance 40 mg 120 mg bid 80 mg 190 185 180 120 mg Weight in lbs 175 170 165 40 mg bid 160 155 Stopped 150 145 140 0 10 20 30 Days 40 Sick Day Medication Advice • Pre-emptive temporary withdrawal of certain medications during period of dehydrating illness • Diarrhea, vomiting, poor intake • Excessive heat exposure, bowel prep, high output ostomy • Instruct patients to stop ACE, ARBs, diuretics, NSAIDs and NSAID creams to avert renal failure, hypotension, hyperK+ • Can resume usual meds when better 40 mg 120 mg bid 80 mg 190 185 180 120 mg Weight in lbs 175 170 165 40 mg bid 160 155 Stopped 150 145 140 0 10 20 30 Days 40 Cardiac Output Frank-Starling curve LV Filling Volume Cardiac Output Frank-Starling curve LV Filling Volume Frank-Starling curve Cardiac Output Normal Heart failure LV Filling Volume Cardiac function and Volume • Changes in volume status can result in marked changes in cardiac output • Reduction in cardiac output leads to heart failure and renal dysfunction • In decompensated heart failure patient renal function may improve with diuresis Advances in Heart Failure Therapy • • • • • • • • • ACE/ARB Aldactone blocker Cardio-selective beta-blockers Antiarrhythmics Implantable defribrillator Cardiac resynchronization therapy Valve repair Revascularization LV restoration Furosemide • Loop diuretic • Introduced 1966 • Excretion 2/3 renal 1/3 hepatic • Half life 100 minutes Diuretic resistance Dose response characteristic • All or none response • Dose threshold Distal Adaptation Breaking Phenomenon NSAIDs Urine production in 6 hrs Furosemide dose-response curve 40 80 120 160 Dose 200 240 280 Urine production in 6 hrs Furosemide dose-response curve Worsening heart and/or renal function 40 80 120 160 Dose 200 240 280 Urine production in 6 hrs Furosemide dose-response curve 40 80 120 160 Dose 200 240 280 Urine production in 6 hrs A B C 40 80 120 160 200 240 280 Dose Furosemide Furosemide changed 120from mg in 80AM, mg 40 po mg to 40 in mg PM po bid What What is is the the intention? intention? What will happen? Adaptation • Longstanding furosemide use can result in hypertrophy of distal tubular cells • Compensatory Na+ reabsorption occurs to counter diuretic effect of loop • Thiazide diuretics effective either as permanent fixture of rescue therapy Thiazides Distal tubule CA Inhibitors Proximal tubule 5% Antikaliuretics 70% 4.5% Thick Ascending Limb Collecting duct 20% 100% GFR 140 L/day Plasma Na 140 mEq/L Filtered Load 26,100 mEq/day 0.5% Loop Diuretics Loop of Henle Volume 1.5 L/day Urine Na 100 mEq/L Na Excretion 155 mEq/day From Knauf & Mutschler Klin. Wochenschr. 1991 69:239-250 Adaptations: Rebound sodium retention “Breaking phenomenon” Urine sodium , mEq/6 hr 300 F – Furosemide 40 mEq/d 250 200 150 100 50 0 F F F F Wilcox, et al, Kidney International 31:135, 1987 Why is volume so unstable? Volume Cardiac Output Renal Function Diuretic resistance 40 mg 190 120 mg bid 80 mg 185 180 120 mg Weight in lbs 175 170 165 40 mg bid 160 155 Stopped 150 145 140 0 10 20 30 Days 40 Diabeto-renal concepts • Sliding scale – Strategy of prescribed proportional dosage adjustments to provide acute correctional action • Target Weight – Use of a set weight as a surrogate for optimal body volume status Diuretic sliding scale • Escalating or declining loop diuretic dose dictated by daily weight • Can incorporate thiazide diuretic as maintenance or rescue to counter adaptation • Can incorporate potassium supplement to compensate for increased potassium losses • Patient feedback and self management Diuretic Sliding Scale FUROSEMIDE No Furosemide, take in more salt No Furosemide 80 mg in AM 80 mg in AM and PM 120 mg in AM and PM 160 mg in AM and PM 200 mg in AM and PM, call MD 167 168 170 173 176 179 180 ZAROXOLYN POTASSIUM 2.5 mg 5 mg 10 mg A B Urine production in 6 hrs WEIGHT less than 167 to 169 to 171 to 174 to 177 to greater than C 40 80 120 160 Dose 200 240 280 1 tab 2 tabs 2 tabs 2 tabs bid 2 tabs bid 40 mg 190 120 mg bid 80 mg 185 180 120 mg Weight in lbs 175 170 165 40 mg bid 160 155 Stopped 150 145 140 0 10 20 30 Days 40 Diuretic Sliding Scale • Patient should weigh self daily, record weight and follow scale instructions • Once established need regular follow-up • Volume check to adjust target weight – Lean weight changes, constipation, amputation, hardware • Reassessment of diuretic response/threshold “When you take your water pill(s), do you pee soon after?” Assessing Edema Intravascular Expansion – Sustained, not intermittent – Wt gain, SOB, orthopnea – History of cardiac disease, high Na+ intake, – Renal insufficiency – JVD, creps, wheeze, effusions Vasodilatory – Worse after prolonged upright posture – Better after prolonged supine – Worse with hot weather – Venous insufficiency – Absence of other risks or signs of volume excess K+ too high too low 40 mg 190 80 mg 120 mg bid K+ Too high Too low 185 180 120 mg 170 6.0 6 165 Serum Potassium Weight in lbs 175 5 40 mg bid 160 155 4 150 3 Stopped 3.2 2.8 145 2 140 0 10 20 30 Days 40 Potassium • Disorders of potassium common in CKD and DM • Like glucose and volume, various factors can drive potassium up or down • Vigilance for these factors, frequent checking and early corrective action can improve K+ management Diabeto-renal concepts Potassium Balance Pushes K+ down • Reduced intake • Loop/thiazide diuretics/steroids • Kayexalate • Diarrhea/vomiting • Alkalosis Too high Serum Potassium Pushes K+ up • Increased intake • ACE, ARB, Spironolactone, NSAID • Sulfa • Renal failure • Acidosis • Tissue breakdown, internal bleeding Too low K+ Management Tips • Combining K+ sparing with K+ wasting agents can aid in K+ balance • Check K+ 2-3 weeks after change in medication that can affect K+ handling ACE/ARB, diuretic, NSAID, Sulfa • Check K+ with worsening overload or dehydrating illness • Instruct patients on dietary K+ K+ Management Tips • Replacement requires 80 – 100 mEq to correct serum potassium by 1 mmol/L in average sized person • Kayexalate: – 30 gm po will reduce serum K+ by about 0.3 mmol/L – Excessive dose can cause hypoMg++, hypoCa++, constipation – Use may be limited by sodium load Hyperuricemia Urate 680 No history of gout or stones Hyperuricemia • Common in – – – – – Metabolic syndrome Heart failure Renal insufficiency Alcohol use Diuretic use • Causes gout, uric acid kidney stones, urate nephropathy • Associations with hypertension, LVH, renal decline in CKD, CV events, but treatment of assymptomatic hyperuricemia not indicated Uric Acid/Gout • Anti-inflammatory treatment of acute gout – NSAID – Volume retention, renal dysfunction, peptic ulceration, hypertension, increased CV risk – Colchicine – Diarrhea, sensimotor neuromyopathy, myelosuppression – Corticosteroids – Volume retention, hyperglycemia, thrush, peptic ulceration – Weight gain, sleep disturbance – AVN Hip, osteoporosis, cataracts Uric Acid/Gout • Anti-inflammatory treatment of acute gout – NSAID – Consider holding ACE/ARB during course – Monitor volume and renal function closely – Consider PPI – Colchicine – Give trial supply and plan B – Corticosteroids – Watch volume and glycemia – Quick taper to low dose – Consider PPI Reducing Hyperuricemia • Reduce diuretics, especially thiazides • Consider once daily or alternate day loop diuretic dose • Low purine diet • Weight loss/exercise • Consider switching ACE/ARB to Losartan Urate Lowering Therapy • Allopurinol – Dose 50 - 300 mg daily in CKD – Can cause rash, pruritis, elevated LFTs, hypersensitivity reaction • Febuxostat – For use if intolerant to Allopurinol • Probenecid – Uricosuric, use only with eGFR > 50 Urate Lowering Therapy • Start 1-2 weeks after acute attack settled with anti-inflammatory therapy • Aim for uric acid level 360 • Continued anti-inflammatory prophylaxis for 6 – 9 months recommended to avert flare • Continue ULT indefinitely Am J Kidney Dis 47:51-59. Summary Multiple factors in diabetorenocardiopath patients conspire to cause instability in volume and potassium status. Strategies to monitor, anticipate and rapidly correct perturbations can help maintain stability Patient self management contributes to optimization in these complex patients Thank You