Mental Health Integration Project
advertisement
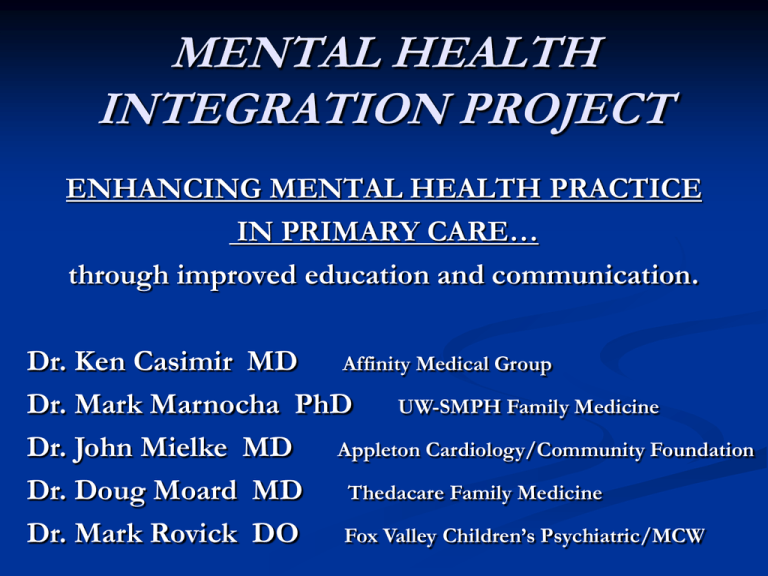
MENTAL HEALTH INTEGRATION PROJECT ENHANCING MENTAL HEALTH PRACTICE IN PRIMARY CARE… through improved education and communication. Dr. Ken Casimir MD Affinity Medical Group Dr. Mark Marnocha PhD UW-SMPH Family Medicine Dr. John Mielke MD Appleton Cardiology/Community Foundation Dr. Doug Moard MD Thedacare Family Medicine Dr. Mark Rovick DO Fox Valley Children’s Psychiatric/MCW Setting Fox Valley region: Third largest urban population area in Wisconsin Larger Cities: Oshkosh, Neenah, Menasha, Appleton. [Green Bay] Smaller Towns: Limited Scope: contiguous communities, and those with linkage via health systems x 2. Region/Community/Practice driven rather than state-level or discipline-specific. Chilton, New London, Shawano, Hortonvlle, Kimberly, Kaukauna, Little Chute, Freedom…. Weaknesses/Threats Serious shortage of Pediatric Psychiatry Inadequate Adult Psychiatry Access Nation-wide shortage of psychiatry Strong Family Medicine practices, though majority not full-scope. (no inpatient medicine or Ob) Family Medicine forced to assume wider scope of MH practice. Strengths/Opportunities Community interests in compassion, education, health-care, and youth services. Community Foundation w/physician voice. Connections with MCW and UW-SMPH Medical residency and consultation programs. Involved psychiatrists with community, primary care, and youth expertise. Community aim to improve MH access, align pediatric MH resources, and upgrade MH prevention. Relevant Literature Diverse studies of upgrading MH care skills among primary care physicians. No clear ‘gold standard’ as far as methods with well-documented and replicated results. Recent statewide initiatives to bolster primary care MH care skills, notably New York, Massachusetts, Nebraska. Pediatric MH concerns increasing, eg, ADHD overdiagnosis, proper use of atypicals, suicide prevention, emerging drug use, cyber issues. MHIP Task Force 630 am meetings begun in 2011 Coffee stat and prn Prior history of diverse connections among MHIP group members. Ongoing alignments with health systems, community initiatives, educational resources. Initial literature review. Questions about regional needs & physician interest? Development of mixed Quantitative/ Qualititative semi-structured interview format. Interview Format 11 Likert or other numeric items. 5 yes-no or other forced choice items. 4 open-ended questions. Comments solicited after all items. Interview responses transcribed by interviewers. Numeric and content summaries by 1st author. Physician Survey Information MHIP 21 semi-structured face-to-face interviews 12 female / 9 male regional physicians Snowball/Convenience Sample MD/DO mix Most Early-Middle career (3-20 years post residency) 17 Family Medicine, 3 Pediatrics, 1 Internal Medicine 8 Affinity; 7 Thedacare; 2 Kaukauna Clinic; 1 each FCCHC, PCA, UW, Independent From Appleton, Chilton, Greenville, Kaukauna, New London, Oshkosh, Shawano, Waupaca General Numerical Findings 57% do not feel proficient caring for MH problems. 67% do not feel counseling is sufficiently accessible. Only 29% identify an MD partner w/special interests in MH care. Only 20% find MH care reimbursement to be a problem. Physician Views about MH Changes BAD NEWS = “More Psychiatrists” is most needed change, but least practical. GOOD NEWS = “More PCP training” is 2nd most needed change, and the most practical. “More Counseling” is moderate in need and practicality. “Reimbursement Change” is least needed, and 2nd least practical. Need for MH Changes 5 change areas rated from 4 = ‘Great Need’ to 1 = ‘Minimal Need’ 4 3.95 3.45 3 3.28 3.17 2.65 2 1 More Psychiatry Physician Training More Counseling Community Reimbursement Education Changes Practicality of MH Changes 5 change areas rated from 4 = ‘Highly’ to 1 = ‘Minimally’ Practical 4 3 3 2.95 2.87 2 1.65 1.38 1 Physician Training Community Education More Reimbursement More Counseling Changes Psychiatry Physician Interest in MH Training 95% indicated they are either “Very amenable - Sign me up” or else “Interested-Have some questions.” Only 1 MD (later career) not interested! Only 24% (5 Physicians) said they need any compensation for such training. EXTENSIVE ideas from physicians for training content, AND for in-depth group training face-toface with primary care peers and psychiatry / MH resource people. Interview Content Summaries Mental Health Care Concerns: Lack of communication w/psychiatry; poor access to general MH resources; access to psychiatry; resources unfamiliarity. Suggested Training Areas: Refractory depression; Younger children; Bipolar; Schizophrenia; Suicide; ADHD; Managing meds; Algorithms for treatment, diagnosis; Listening/counseling. Initial MHIP Conclusions Additional psychiatric training is clearly identified by PCPs as both necessary and practical 95% of surveyed PCPs were either “interested” or “very interested” in structured psychiatry CME training Only 24% of surveyed PCPs identified a need for reimbursement for CME time Conclusions (continued) PCPs identify their relationships with psychiatrists as less than satisfactory Communication regarding available mental health resources is inadequate Improvement of MD-MD relationships, along with readily accessible network re: available resources is essential Current status of project Community Funding Initial curriculum per ASCP, with augmentation prn 9 monthly evening sessions Emphasis on complex cases, minimal basic review, and current evidence/practice updates 2.5 hours with dinner ~50 registrants; including NPs and students/residents. Future iterations may include office staff involved in MH case management Session eval forms; pretest and posttest assessment of comfort with aspects of complex OP MH care.