Steroid Sick Day Rules Endocrinology

Clinical Guideline
“SICK DAY RULES” FOR ADULT ENDOCRINE PATIENTS WITH
PROVEN GLUCOCORTICOID DEFICIENCY/DEPENDENCY
SETTING
FOR STAFF
Trust wide
All Medical Staff
PATIENTS Patients with proven glucocorticoid (cortisol) insufficiency secondary to either adrenal or pituitary pathology and who are taking daily replacement glucocorticoid medication
-------------------------------------------------------------------------------------------------------------------------------------------
All patients should be advised to wear a Medic Alert
talisman at all times. Medic Alert ® can also be contacted during office hours, Mon-Fri, 9am-5pm on Free phone: 0800 581420.
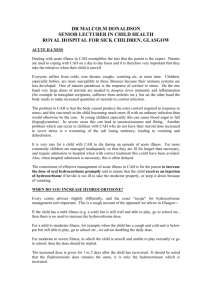
Sick Day Rules
Should the patient face an extreme physical stress such as trauma, surgery or acute illness they will require extra steroid cover so that the body can meet that stress. Without increasing the steroid dose they may experience severe weakness, headache, dizziness, nausea and vomiting and possibly a more serious deterioration in health. Typically the dose of steroids will only need to be increased for a couple of days if they have an illness that is transient and managed in the community. If they are unable to take/absorb an increased dose of steroids orally because of vomiting or diarrhoea, they will urgently require steroid injections and should attend an Accident & Emergency Department or be seen by a Medical Practitioner at home quickly.
The general advice for any serious illness is as follows:
1. Double the normal daily steroid dose (no increase in Fludrocortisone is required) when the patient has a temperature of more than 37.5
0 C (99.5
0 F).
2. The patient should be advised to contact their GP if their illness worsens or it lasts for more than
3 days and they should be advised to always seek medical help if their temperature reaches 40 0 C
(104 0 F). In severe illness urgent medical assistance should be promptly sought (999 ambulance if appropriate).
3. As soon as the patient’s temperature returns to normal, their steroid dose should be gradually tapered back to their normal daily dose within two days.
4. If the patient experiences vomiting/diarrhoea then they should be advised to take an additional
20mg Hydrocortisone (or 5mg Prednisolone or 0.75mg Dexamethasone or 25mg Cortisone
Acetate as relevant) immediately afterwards and they should sip rehydration/electrolyte fluids. If they experience repeated vomiting or diarrhoea then they should seek urgent medical help.
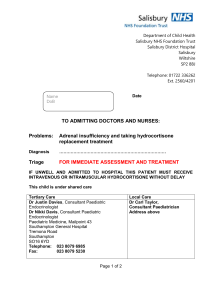
Steroid Emergency Pack
All patients should have 100mg Hydrocortisone for injection with needle and syringe [Efcortesol
(liquid) or Solu-Cortef (powder plus vial of water)] available at home for use in an emergency. This should be administered promptly by a health care professional who is called out to visit the patient at home rather than being delayed until they reach hospital. The GP practice nurse may also be willing to teach the patient how to self-administer this injection should they wish to learn. It is crucial to emphasise that should a patient be unwell enough to require an injection of hydrocortisone in the community then they should also promptly attend their local hospital as an emergency for assessment.
Version 2 Aug 2013 - Review Aug 2016 Authors Dr Karin Bradley & Dr Natasha Thorogood, Endocrinology Consultants Page 1 of 2
Surgery
Any surgery will require intramuscular or intravenous steroid injection. We encourage our patients to discuss their endocrine condition and the need for extra steroid cover before-hand with their Surgeon or
Anaesthetist. They often find it helpful to show this letter to Health Care Professionals in order to clarify their need for steroid cover . Further guidance can be obtained from the patient’s named consultant in the department of Endocrinology at the BRI. Typically for major surgery 100-150mg hydrocortisone is appropriate over the first 24hours but this can be quickly reduced with recovery. This can be given in three or four divided iv or im boluses or as an iv infusion at a rate of 4mg/hr.
For example:
100 mg of intravenous or intramuscular Hydrocortisone with induction of general anaesthetic followed by
24 hours of Hydrocortisone 50mg three times daily via the intravenous/intramuscular route, decreasing to Hydrocortisone 20mg orally three times daily for 24 hours on second postoperative day and then reduce to double normal standard replacement (20mg on waking, 10mg at 12pm and 10mg at 5pm).
Advise as prompt as possible a return to standard replacement Hydrocortisone (typically 10mg on waking, 5mg at 12pm and 5mg at 5pm).
Pregnancy and Labour
Evidence shows that in normal pregnancy the circadian rhythm is preserved but that free/bioavailable cortisol increases in late pregnancy and so glucocorticoid replacement may need to increase in the late second or third trimesters. There is no routine approach and this should be individualised based on symptoms and baseline dosage – an increase of ~25-30% is not unreasonable if required. No biochemical monitoring of steroid replacement is required.
During normal labour/normal vaginal delivery it is appropriate to recommend that normal oral glucocorticoid dosages are doubled. No increase in mineralocorticoid (fludrocortisone) is required. These can be rapidly tapered back to normal following delivery.
Any significant instrumental delivery, surgery or general anaesthetic should result in intramuscular or intravenous steroid injections instead of their normal oral replacement. Please see above under the surgical guidance notes.
Post-partum, remember to advise that the patient may need to modify their normal glucocorticoid regimen based on their sleep pattern to ensure adequate energy levels. Typically the approach would be to alter the frequency of doses rather than to alter the total dosage for any prolonged period.
-------------------------------------------------------------------------------------------------------------------------------------------
For patients with a diagnosis of primary adrenal failure ( Addison’s disease) then additional information is available from the Addison’s Disease Self Help Group ( www.addisons.org.uk
) and for patients with pituitary disease advice is available from The Pituitary Foundation
( http://www.pituitary.org.uk
)
-------------------------------------------------------------------------------------------------------------------------------------------
USER GROUPS CONSULTED: Endocrinology, Surgery and Anaesthetics via the Neuroendocrine MDT.
Obstetrics via Joint Endocrine Antenatal Clinic.
QUERIES: Endocrine Specialist Registrar (referrals) bleep 6216 (9am-5pm weekdays)
Endocrine consultants via switchboard
Version 2 Aug 2013 - Review Aug 2016 Authors Dr Karin Bradley & Dr Natasha Thorogood, Endocrinology Consultants Page 2 of 2