DIC
advertisement

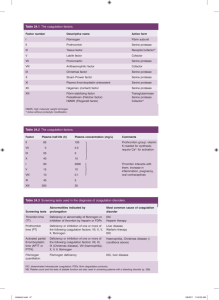
DIC Dr MB Dhlamini Department of Molecular Medicine and Haematology WITS University Objectives for the DIC lecture Definition of DIC Describe the pathogenesis of DIC Discuss mechanisms of acute DIC Definition of subacute/chronic DIC Discuss sequelae of activation of coagulation cascade. Describe examples of underlying disease and DIC. Discuss principles of laboratory diagnosis of DIC Describe management principles of DIC Disseminated Intravascular Coagulopathy Definition: -Clinicopathological syndrome in which wide spread intravascular coagulation is induced by procoagulants that are introduced /produced in the blood & overcome the natural anticoagulant mechanism. DIC characterised by: Systemic intravascular coagulation – widespread fibrin deposition in circulation Results : microvascular dysfunction & organ failure Massive ongoing activation may result in depletion of platelets & coagulation factors– bleeding. Secondary fibrinolysis Clinical Picture - DIC Underlying disorder S yste m ic a ctiva tio n of coa g u la tion W id esp rea d de p osition C o nsu m p tion o f P la te le ts M icro va su lar th rom b o tic o b stru ction D e cre a sed P late le ts & Co a gu la tio n facto r d e ficie n cy O R G A N F A IL U RE B L E E D ING Pathogenesis of DIC Acute DIC : Triggering mechanisms (TMS) 1. Entry of thromboplastins with high phospholipid concentration into circ. e.g. a) following extensive tissue trauma during surgery. b) Acute Vascular haemolytic episode (ffg incompatible blood transfusion) Acute DIC TMS cont’d 2. Direct activation of Factor X or Prothrombin(Factor II) by specific proteolytic enzymes in snake venom. 3. Severe Vascular Endothelial Injury e.g. gram negative septicaemia viral/protozoal diseases extensive burns – exacerbated by prolonged hypotension, hypoxia, acidosis Acute DIC TMS cont’d 4. Direct platelet activation in septicaemia and viraemic states or activation of platelets following: a) vessel wall endothelial damage b) thrombin generation by the coagulation cascade Subacute/Chronic DIC Slow activation of haemostatic system Spontanteous bruising rather than major bleeds Chronic compensated DIC can continue for many years – usu. Assoc. with vascular malformations Sequelae of Activation of the Coagulation Cascade Thrombin generation– fibrinogen converted to fibrin Trace amts of thrombin inactivated by formation of thrombin-antithrombin complexes ( protective mechanisms) If excess thrombin– cleavage of fibrinopeptide A & B from Aά & Bβ forming monomers Fibrin monomers polymerize to form fibrin clot Sequelae cont’d Fibrin strands/platelet aggregates cause blockage of arterial circ. Loose fibrin platelet plugs form a fine mesh sieve– red cells passing through distorted & fragmented ---- intravascular haemolysis Sequelae cont’d Secondary activation of the fibrinolytic pathway. ffg fibrin deposition – tPA released from vascular endothelium converting plasminogen to plasmin within fibrin clot Free plasmin – cleavage of fibrinogen and lysis of cross linked fibrin Breakdown of fibrinogen– formation of fragments D/E ( via X-Y) Sequelae cont’d Specific lysis of fibrin—formation of specific FXIII cross linked complexes incl. D-Dimers Fibrinogen/fibrin breakdown—FDPs or DDimers) Free plasmin may also cleave other peptides e.g.FV, FVIII & 1st component of complement. Sequelae cont’d Liver cell synthesis fails to compensate for their consumption thus decreased Factors V, VIII, XIII, fibrinogen BM megakaryocyte production unable to maintain normal plt count Sequelae cont’d Combination of : - coagulation factor deficiency - thrombocytopenia - impaired platelet function - inhibitory action of raised FDPs = generalised/continued widespread bleeding Underlying Dx Bacterial infections - most common cause gram negative lipopolysaccharide gram positive exotoxin cytokines Meningococcemia- Purpura on the calves Meningococcemia-2 Underlying Dx cont’d Other infections 1) Viral e.g. viral haemorrhagic fever probably via endothelial damage 2) Protozoa e.g. Malaria Underling Dx cont’d Trauma - frequently associated with 1) release of phospholipid 2) endothelial damage 3) Cytokines also play a role Underlying Dx cont’d Malignancy - low grade or subacute DIC - Trigger Tissue Factor: usu. assd with metastatic disease e.g. Ca Pancreas, Ca lung, Ca stomach - APL : hyperfibrinolysis, TF on leukaemic cells Underlying Dx cont’d Obstetrics - implicated in the following 1) Septic abortion 2) Abruptio Placenta 3) Ecalmpsia 4) Placent Praevia 5) Amniotic fluid embolism Underlying Dx obstetrics cont’d Mechanisms - entrance of cellular elements of the decidua/placenta with thromboplastin-like activity into maternal circ. - meconium and fetal squamous cells from amniotic fluid into maternal circulation– activation of coagulation - IUD – slow progressive DIC– bleeding late manifestation Underlying Dx cont’d Vascular disorders 1) large aortic aneurysms 2) Kasabach-Merrit syndrome ---- result in local activation of coagulation ---- overflow into systemic circ. Diagnosis of DIC -Investigate underlying dx -Evidence of consumption eg. Thrombocytopenia,prolonged INR/PTT,decreased factors -Evidence of activation of fibrinolytic pathway : elevated D-Dimer levels and presence of FDP’s -Decrease in coagulation inhibitors: Antithrombin,Protein C&S Management of DIC NB: Rx of the underlying disease Supportive management eg. Platelets, FFP’s, cryoprecipitate Coagulation inhibitors : Heparin, Antithrombin and Activated Protein C Stroke Case Studies 38yr male,RVD positive, neutropenic Confused, not on warfarin or heparin INR 1.08, PTT 34.90s, D-Dimers 1.66mg/l, fibrinogen 3.81g/l ,antithrombin 110% and platelets 182x10^9/l Case 2 66yr old female post- NSTEMI, treated with antibiotics for infection INR 2.73, correct. 1.01,PTT 32.6s, DDimers 0.87mg/l, fibrinogen 4.1g/l ,Factor VII 17%, Antithrombin 84% and Plt 204x10^9/l. Case3 52yr female with perforation of the bowel and sepsis INR1.82, correct. 1.33, PTT 65.5s,correct 34.1s, D-Dimers 4.71mg/l, fibrinogen 1.96g/l, antithrombin 57% and platelets 35x10^9/l. Thrombin ratio 0.78 (within normal range)