Chronic DIC
advertisement

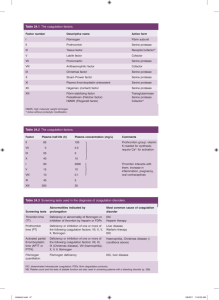
Disseminated Intravascular Coagulation Coagulation cascade Extrinsic system (tissue damage) Intrinsic system (surface contact) XII XIIa Tissue factor XIa XI IX VIIa IXa VIII VIIIa X Vitamin K dependant factors VII Xa V Va II Fibrinogen IIa IIa (Thrombin) Fibrin DIC may be initiated by Exposure of blood to tissue factor (eg after trauma). Endothelial cell damage (eg by endotoxin or cytokines). Release of proteolytic enzymes into the blood . ( eg pancreas , snake venom ) Infusion or release of activated clotting factor. (eg Factor IX concentrate ) Massive thrombosis. Severe hypoxia and acidosis. Disseminated Intravascular Coagulation (DIC) Mechanism Systemic activation of coagulation Intravascular deposition of fibrin Thrombosis of small and midsize vessels with organ failure Depletion of platelets and coagulation factors Bleeding Acute DIC Acute DIC develops when blood is exposed to large amounts of tissue factor over a brief period of time . - Bleeding - Acute renal failure - Hepatic dysfunction - Pulmonary disease - Central nervous system dysfunction - Malignancy Chronic DIC: chronic DIC develops when blood is continuously or intermittently exposed to small amounts of tissue factor and compensatory mechanisms in the liver and BM are largely able to replenish the depleted coagulation proteins and platelets . Chronic DIC: *Malignancy, the most particularly solid tumors, ( is common cause of chronic DIC). *Venous thromboses commonly present as deep venous thrombosis in the extremities or superficial migratory thrombophlebitis (Trousseau's syndrome), *Arterial thromboses can produce digital ischemia, renal infarction, or stroke. DIAGNOSIS of DIC Acute DIC: Fibrin degradation product or D-dimer levels. Prothrombin time. Activated partial thromboplastin time. deficiencies of factors XII, XI, IX and VIII. Plasma fibrinogen concentration . Chronic DIC: platelet count moderately reduced. plasma fibrinogen is often normal or slightly elevated. PT and PTT may be within normal limits. DIC versus fibrinolysis: Primary fibrinogenolysis occurs when plasmin is generated in the absence of thrombosis. It is may occur in certain conditions, such as : direct infusion of thrombolytic agents and in patients with prostate cancer . It can be distinguished from DIC by the absence of elevated level of D-dimers. However, when fibrinolysis is prominent, elevated levels of D-dimer and other fibrin degradation products will be present. DIC versus TTP-HUS: The pathogenesis of DIC, a thrombotic microangiopathy resulting from activation of the coagulation system, is different from the pathogenesis of another thrombotic microangiopathy, Thrombotic thrombocytopenic purpura-hemolytic uremic syndrome ( TTP-HUS ) , which results from primary platelet activation due in many cases to a congenital or acquired defect in von Willebrand factor cleaving protease or primary endothelial injury. TREATMENT 0f DIC Platelet transfusion Fresh frozen plasma Heparin ? Protein C concentrate Treatment of the underlying disease Definition of DIC • DIC is a clinicopathologic syndrome in which widespread intravascular coagulation is induced by procoagulant that are introduce or produce in circulation and overcome the natural anticoagulant mechanisms. • DIC may cause tissue ischemia from occlusive microthrombi as well as bleeding from both consumption of platlet and coagulation factor and anticoagulation effect of product of secondary fibrinolysis. Common clinical conditions associated with Disseminated Intravascular Coagulation Activation of both coagulation and fibrinolysis Triggered by • Sepsis • Trauma – Head injury – Fat embolism • Malignancy • Obstetrical complications – Amniotic fluid embolism – Abruptio placentae • Vascular disorders • Reaction to toxin (e.g. snake venom) • Immunologic disorders – Severe allergic reaction – Transplant rejection Pathogenesis of DIC Release of thromboplastic material into circulation Coagulation Fibrinogen Thrombin Fibrin Monomers Fibrin Clot (intravascular) Consumption of coagulation factors; a PTT PT TT Fibrinolysis Fibrinogen Presence of Plasmin plasmin FDP Intravascular clot Fibrin(ogen) Platelets Degradation Schistocytes Products Plasmin Disseminated Intravascular Coagulation Treatment approaches • Treatment of underlying disorder • Platelet transfusion • Fresh frozen plasma • Anticoagulation with heparin • Coagulation inhibitor concentrate (ATIII) Management of underlying disordes although the pt may benefit from other treatment survival depend on vigorous treatment of underlying disorder : • • • • • Intensive antibiotic treatment in G- bacteremia Hysterectomy in abruptio placenta Resection of aortic aneurism Debridment of crush tissue Volume replacement , correction of hypotention & oxygenation, restore the function of coagulation inhibitory system. Replacement therapy • For thrombocytopenia : 6-10 U plat (ideally rise to more than 50000-100000) • For hypofibrinogenemia (<100 ) : 8-10 U Cryopercipitate • For coagulation factor depletion : 1-2 U FFP • ( depend on severity of depletion & body weight) Classification of thrombocytopenia • Associated with thrombosis – Thrombotic thrombocytopenic purpura – Heparin-associated thrombocytopenia – Trousseau’s syndrome – DIC – AML (m3) • Associated with bleeding – Immune-mediated thrombocytopenia (ITP) – Most others Classification of platelet disorders • Quantitative disorders – Abnormal distribution – Dilution effect – Decreased production – Increased destruction • Qualitative disorders – Inherited disorders (rare) – Acquired disorders • Medications • Chronic renal failure • Cardiopulmonary bypass