Disseminated Intravascular Coagulation
advertisement
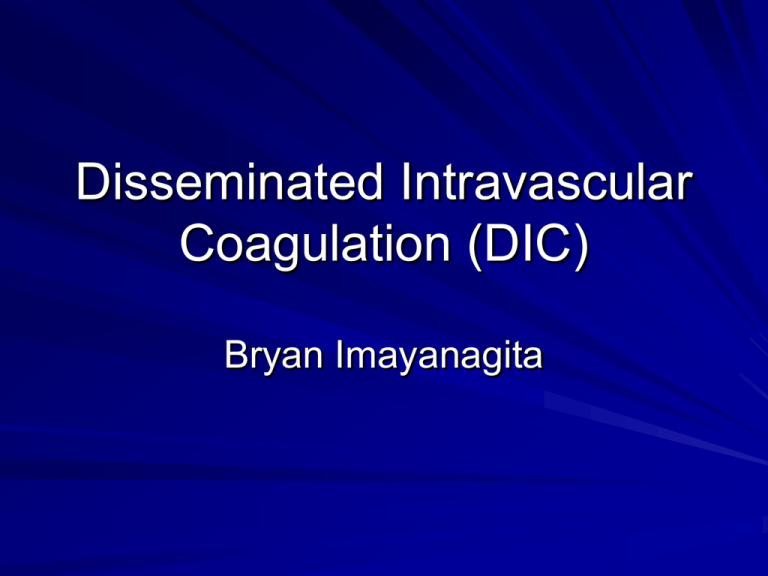
Disseminated Intravascular Coagulation (DIC) Bryan Imayanagita Background Pathological activation Formation of clots throughout the body in the blood vessels Leads to abnormal bleeding; can cause clots that disrupt blood flow to organs Multiple organ failure and death Causes Sepsis (most common) endothelial cell damage (heat stroke, shock) obstetrical complications neoplasias trauma Pathophysiology fire/fire extinguisher analogy in normal coagulation Thrombin (fire) generation at the site of injury The endothelium (fire extinguisher) expresses antithrombin molecules which will bind to thrombomodulin No endothelium at damaged tissue site; allows coaguation. Stopped once thrombin reaches healthy tissue. In DIC, coagulation and anti-coagulation out of balance Diagnosis Bleeding from 3 unrelated sites History of blood loss, hypovolemia DVT, microvascular thrombosis Main Features of DIC Features Bleeding Affected Patients, % 64% Renal dysfunction 25% Hepatic dysfunction 19% Respiratory dysfunction 16% Shock 14% Central nervous system dysfunction 2% Treatment Determined if patient is bleeding or needs an invasive procedure – If either is positive: fresh frozen plasma or cryoprecipitate can be given Folic acid Heparin treatment not established – May not be effective; needs anti-thrombin for anticoagulant activity, reduced by DIC Prognosis 10%-50% mortality rate DIC with sepsis significantly higher than DIC with trauma Sources http://www.medstudents.com.br/terin/terin2 .htm http://emedicine.medscape.com/article/77 9097-overview