Malaria
advertisement
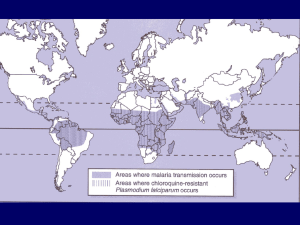
One day Workshop YUMS |Tissue and Blood Protozoan diseases Malaria & Leishmaniasis Mohammad Amin Ghatee Ph.D in medical Parasitology MALARIA THE KILLER DISEASE • 500 million people suffer from malaria •Over one million of people die each year. • •The majority of victims are children and pregnant women. (one African child every 30 seconds) • Sub-Saharan Africa bears 90 per cent of the burden. Plasmodium species which infect humans Plasmodium falciparum (tertian) Plasmodium vivax (tertian) Plasmodium malariae (quartian) Plasmodium ovale (tertian) Geographical distribution and incidence of malaria Figure 23.10 Plasmodium species • Plasmodium falciparum: Tropics. Accounts for 50% of all malaria cases. Most pathogenic. • Plasmodium vivax: Tropics, subtropics, and some temperate regions.. About 43% of all malaria cases. Some Africans are refractory to infection because the lack the red cell receptor that the parasite use to enter. • Plasmodium malariae: Tropics. About 7% of all malaria cases. • Plasmodium ovale: West Africa. Rare. HOSTS DEFINITIVE HOST: Anopheline female Mosquito (sexual reproduction) INTERMEDIATE HOST: Humans (asexual and sexual phases) Malaria Life Cycle Types of Infections • Recrudescence – exacerbation of persistent undetectable parasitemia, due to survival of erythrocytic forms, no exo-erythrocytic cycle (P.f., P.m.) – Blood origin – Can be occurred along the life time • Relapse – reactivation of hypnozoites forms of parasite in liver, separate from previous infection with same species (P.v. and P.o.) – Tissue (liver) origin – Up to 3-5 years after primary infection Erythrocytic phase stages of parasite in RBC • • • • Young trophozoites or ring form Tropohozoite forms merozoites Schizogeny to forms merozoites releasing merozoites into blood stream. • Merozoites invade other RBCs and schizongeny is repeated • Parasite density increases until host’s immune response slows it down • Merozoites may develop into gametocytes (gametogony), the sexual forms of the parasite Development in the mosquito • Upon ingestion with a blood meal, both the micro and macrogametocyte rapidly mature • Macrogamete is released from ruptured rbc • Microgametocyte rapidly undergoes multiple nuclear divisions to form 8 gametes • Exflagellation Development in the mosquito: the ookinete A mature ookinete. A number of organelles are shown. The nucleus can be seen at the lower end of the organism. There are abundant ribosomes in the area above the nucleus and endoplasmic reditulum can also be seen. The zygote is surrounded by a three-layered pellicle. The apical complex at the upper end includes numerous rhoptries and micronemes (dark spots). Image from Sinden RE. "Malaria", Topics in Inernational Health,(1998) The WellcomeTrust, CABI Publishing, CAB International Development in the mosquito • Encysted ookinete transforms into oocycst • 10-14 days of development • reductional nuclear division, haploid again • multiplication to form 1000’s of sporozoites THE OOCYST SEM which shows two oocysts on the outer wall of the midgut of a mosquito. These contain developing P. gallinacium sporozoites. Image from Guggehheim R."Malaria", Topics in Inernational Health,(1998) The WellcomeTrust, CABI Publishing, CAB International) Anopheles gambiae, the deadliest malaria vector (top), and blue-colored Plasmodium oocysts, appearing from the mosquito’s gut. (MOSQUITO ENGINEERING:Building a Disease-Fighting Mosquito. Martin Enserink/Science 2000 290: 440-441. (in News Focus) Schizogenic periodicity and fever patterns • Schizogenic periodicity is length of asexual erythrocytic phase – 48 hours in P.f., P.v., and P.o. (tertian) – 72 hours in P.m. (quartian) • Initially may not see characteristic fever pattern if schizogony not synchronous. • With synchrony, periods of fever or febrile paroxsyms assume a more definite 3 (tertian)- or 4 (quartian)- day pattern. Clinical presentation • Early symptoms – – – – – – – – – Headache Malaise Fatigue Nausea Muscular pains Slight diarrhea Slight fever Photophobia Anorexia • Could mistake for influenza or gastrointestinal infection Paroxysm of malaria Malaria Paroxysm • Malaria tertiana: 48h between fevers (P. vivax and ovale) • Malaria quartana: 72h between fevers (P. malariae) • Malaria tropica: irregular high fever (P. falciparum) Disease Severity Pv Po Pm Pf moderate Paroxysm mild to mild severe Severity moderate to severe Average 50,00020,000 9,000 6,000 500,000 (per mm3) Maximum 50,000 30,000 20,000 2,500,000 (per mm3) Anemia ++ + ++ ++++ Duration Disease 3-8 w 2-3 w 3-24 w 2-3 w Infection 5-8 y* 12-20 m* >20 y 6-17 m Complications renal cerebral** *true relapses ( recrudescence) due to dormant hypnozoite stage in liver **plus many other organs Malaria the disease 3 Severe manifestations Cerebral malaria Irritability, loss of reflexes, neurological symptoms similar to menigitis, coma 20% fatality Severe anemia Progressive severe drop of hematocrit, poor oxygen Supply for organs and tissues Renal failure Dwindling urine, high urea Level in serum Knobs and cytoadherence • Cytoadhrence and rosetting correlates with the presence of “knobs” (left column) on the surface of the infected RBC • The right column shows a RBC infected with a knob-less strain which does not cause cerebral malaria • Knobs are made up of parasite derived proteins knobs knob-less Cerebral Malaria Possible Pathophysiology cytoadherence cerebral ischemia hypoxia, metabolic effects, cytokines (eg, TNF-) coma death Severe anaemia - pathogenesis • Erythrocyte destruction during schizogony (destruction of both parasitized and nonparasitized erythrocytes) Spleen • Erythrophagocytosis in spleen • Immune mediated response • Black water fever • Bone marrow suppression Other severe complications • Pulmonary oedema • Renal insufficiency (nephrotic syndrome) – P. malariae • Haemolysis • Thrombocytopaenia, DIC • Superinfections (secondry infection) – Septicaemia Immunity and Resistance in malaria • Protective immunity to malaria is primarily a premunition. • In highly endemic areas, infants are protected by maternal antibodies, and young children are at greatest risk after weaning. Genetically resistance factors • Sickle cell anemia, favism, and thalassemia can cause resistance to infection by P. f -Duffy blood groups and P. v Modes of transmission • 1. Natural or biological transmission • 2. Accidental transmission: blood transfusion sharing of needles by IV drug users 3. Maternal transmission Malaria Diagnosis Clinical Diagnosis: • Symptoms: fever, chills, headache, malaise, etc. • History of being in endemic area • Splenomegaly and anemia as disease progresses Malaria Diagnosis Laboratory diagnosis: • Microscopic demonstration of parasite in blood smear (distinguish species) • thick film: more sensitive • thin film: species identification easier • Fluorescent microscopy • antigen detection ‘dipstick’ • Serology • Polymerase Chain Reaction 1. 4. Touch 3 drops of blood to a clean slide. Carry the drop of blood to the first slide and hold at 45 degree angle. 2. 5. Spread the drops to make a 1 cm circle. Pull the drop of blood across the first slide in one motion. 3. Touch a fresh drop of blood to the edge of another slide. 6. Wait for both to dry before fixing and staining. Malaria Blood Smear • Remains the gold standard for diagnosis • Giemsa stain • distinguishes between species and life cycle stages • parasitemia is quantifiable • Requirements: equipment, training, reagents, supervision • Simple, inexpensive yet labor-intensive • Accuracy depends on laboratorian skill Interpreting Thick and Thin Films • THICK FILM – – – – – – – – lysed RBCs larger volume 0.25 μl blood/100 fields blood elements more concentrated good screening test positive or negative parasite density more difficult to diagnose species • THIN FILM – – – – fixed RBCs, single layer smaller volume 0.005 μl blood/100 fields good species differentiation – requires more time to read – low density infections can be missed Malaria Parasite Erythrocytic Stages Ring form Schizont Trophozoite Gametocytes Plasmodium falciparum Infected erythrocytes: normal size, maurers cleft, discrimination of P. falciparum from other species is a important, because P. falciparum in blood of non-immune case is a medical emergency. M I Gametocytes: mature (M)and immature (I) forms Rings: double chromatin dots, multiple infections in same red cell Schizonts: 16-24 merozoites (rarely seen in peripheral blood) Trophozoites: compact Plasmodium vivax Infected erythrocytes: enlarged up to 2X; deformed; (Schüffner’s dots)) Rings Schizonts: 12-24 merozoites Trophozoites: ameboid; deforms the erythrocyte Gametocytes: round-oval Plasmodium ovale Infected erythrocytes: moderately enlarged (11/4 X); fimbriated; oval; (Schüffner’s dots) “malariae - like parasite in vivax - like erythrocyte” Trophozoites: compact Rings Schizonts: 6-12 merozoites;(usually 8) dark pigment Gametocytes: round-oval Plasmodium malariae Infected erythrocytes: size normal to decreased (3/4X), Zeimanns dots Trophozoite: compact Trophozoite: typical band form Schizont: 6-12 merozoites (usually 8); coarse, dark pigment ; (“rosettes”) Gametocyte: round; coarse, dark pigment Malaria Serology – antibody detection Antibodies to asexual parasites appear some days after invasion of RBCs and may persist for months • Positive test indicates past infection • Not useful for treatment decisions – Investigating congenital malaria, esp. if mom’s smear is negative Malaria Antigen Detection • Immunologic assays to detect specific antigens • Commercial kits now available as immunochromatographic rapid diagnostic tests (RDTs), used with blood • P. falciparum histidine-rich protein 2 (PfHRP-2) • parasite LDH (pLDH) • Monoclonal and polyclonal antibodies used in antigen (Ag) capture test • Species- and pan-specific Ab • Cross reactivity with rheumatoid factor reportedly corrected Detection of Plasmodium antigens Polymerase Chain Reaction (PCR)) • Molecular technique to identify parasite genetic material • Uses whole blood collected in anticoagulated tube (200 µl) or directly onto filter paper (5 µl) • Definitive species-specific diagnosis now possible Treatment • • • • Chloroquine Primaquine Quinine Artemisinins Selected Anti-Malarials • Blood schizonticides: 1-Rapid acting: Chloroquine, Amodiaquine, Quinine, Quinidine, Mefloquine, Atovaquone, Artemisinin 2- Slow acting: Antifolates(Fansidar, proguanil) , Clindamycin, Tetracyclines, Proguanil Tissue schizonticides: Primaquine , Proguanil Gametocidal: Primaquine Anti – relapsing: Primaquine Chinchona the source of quinine • Peruvian Indians appear to have been the first to know about the medicinal effects of quinine. • They chewed Chinchona bark while working in the mines as forced laborers for the Spanish Malaria Drug Therapy in Iran Plasmodium falciparum & Plasmodium malariae infections First day: Chloroquine 600 mg (4 tab), 6 h later: 300 mg Second day: Chloroquine 300 mg Third day: Chloroquine 300 mg & Primaquine 45 mg (3 tab) Vaccine • Radiated sporozoite • Sporozoite recombinant proteins • Spf66: synthethic polypeptides of merozoites • RTS,S: recombinant HBV surface protein and parasite proteins