Adult starvation and disease-related malnutrition: A proposal for
advertisement

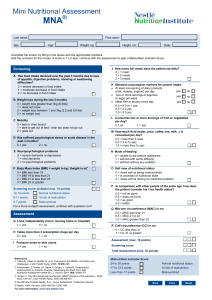
Malnutrition 實習生:曾郁涵 指導老師:林京美營養師 報告日期:2012/12/21 2 Clinical Nutrition 29 (2010) 151–153 journal homepage: http://www.elsevier.com/locate/clnu 3 Recent evidence suggests that varying degrees of acute or chronic inflammation are key contributing factors. Malnutrition has measurable and important adverse effects on clinical outcomes. It is important to recognize the presence or absence of a systemic inflammatory response. Methods An International Guideline Committee was constituted to develop a consensus approach to defining malnutrition syndromes for adults in the clinical setting. Consensus was achieved through a series of meetings held at the ASPEN and ESPEN Congresses. 4 5 chronic starvation without inflammation S tarvation - Related M alnutrition inflammation is chronic and of mild to Chronic D isease- R elated M alnutrition moderate degree inflammation is acute A cute D isease- R elated M alnutrition and of severe degree 6 7 8 1. Translation of this diagnostic approach to routine clinical practice will require validation. 2.These transitions may be blunted by nutritional intervention, early recognition of the process is imperative. 3. Patient with SRM or CDRM is prone to deteriorate quickly with any additional acute inflammatory event. 4. Sarcopenic obesity may represent a chronic low level inflammatory state. 9 Clinical Nutrition 30 (2011) 194-201 Introduction In German hospitals, every fourth adult patient at admission is already malnourished or has a risk. To improve patient outcome and to decrease costs for the health care systems. Aim to develop and evaluate a routinely manageable concept for an improved nutritional care of malnourished in-hospital patients. 10 11 Intervention trial between January 2007 and November 2007 (follow up until June 2008) Under nutrition risk (NRS ≧ 3) CG standard hospital care I individualized nutritional support G (5 to maximum 28 days) Exclusion criteria : •no informed consent •terminal condition Detailed nutritional assessment Prescribed by physician •expected stay <5 days Individual food supply in this study independently. •previous participation •patient on starvation Fortification of meals •PN (maltodextrin, rapeseed oil, •being on dialysis cream, protein powder) In-between snacks and oral nutritional supplements 12 13 • • • • • • • • • • average daily energy and protein intake changes in bodyweight during hospitalization number of complications number of antibiotic therapies due to infectious complications length of hospital stay(LOS) quality of life Short Form 36 Questions (SF-36) Score hospital readmission (after six months) mortality (hospital and six months after discharge) oral nutrition standard supplement consumption plasma concentrations of 25-OH-D3, ascorbic acid and glutathione 14 15 ≧75%TEE I G: 83% CG: 30% 16 17 66.1 → 68.1 → p=0.002 18 Both are low compliance with Oral nutrutional supplement(ONS). IG Ascorbic acid Glutathione 25-OH-D3 - In-hospital complications was lower in IG than in CG. Antibiotics treatment were more often prescribed to patients of CG than IG. Patients of CG were more often re-hospitalized. 19 20 21 Body weight attribute a major effect to energy intake. ◦ <75% TEE, was associated with weight loss. Acute or chronic disease has to consider an higher metabolic rate. Lack of energy and protein is accompanied with micronutrient deficiencies . Food quality shall still be considered apart from food quantity. 22 Nutritional care has to follow a tight algorithm in order to guarantee that the daily individual needs. Malnourished patients profit from nutrition support regarding nutrition status and quality of life. They have fewer complications, need fewer antibiotics and are less often re-hospitalised 23 Clinical Nutrition 31 (2012) 637-646 Introduction If nutritional therapy is not adequately provided, these patients have a higher risk of diminished physiological function, complications, longer length of hospital stay, decreased quality of life, and mortality. This study aimed at exploring food sensory quality as experienced and perceived by patients at nutritional risk during various meals. 24 25 • NRS-2002 ≧ 3 •Food intake < 75% Meal observations food records open-ended question (experiences and preferences) 26 27 28 Food sensory perception and eating ability Food sensory needs Appearance Aroma ACCEPT: garnished /plain and simple DISLIKE: haphazardly ACCEPT: cold with limited smell (strawberry, forest berry and orange) DISLIKE: warm dishes / citrus flavoured supplement ACCEPT: natural, neutral flavour (Sour) →varity Taste DISLIKE: bitter tastes Specific foods (e.g., coffee, tea, dark chocolate, wine, red meat) due to heightened bitter flavours or metallic tastes 29 ACCEPT: soft and fluid (moisture)foods Texture Temperature Variety DISLIKE: dairy products(sickly film) difficult to cut, troublesome packaging PREFER: hot meals drinks→ice cold •Mose patients prefer variety of food. •Difficulty eating patient tended to eat similar foods and a more fixed diet. Motivation to eat ◦ Pleasure ◦ Comfort ◦ Survival Hospital admission versus post-discharge 30 31 32 33 The study generated a model for optimizing food sensory quality and even developing innovative foods to promote intake in patients at nutritional risk. 34 Summary • The commentary present a simple etiologybased construct for the diagnosis of adult malnutrition in the clinical setting. • To develop and evaluate a routinely manageable concept for an improved nutritional care of malnourished in-hospital patients. • A model for optimizing food sensory quality and developing innovative foods to promote intake in patients at nutritional risk.