Nutrition and Dietetics in the Normal Patient
advertisement

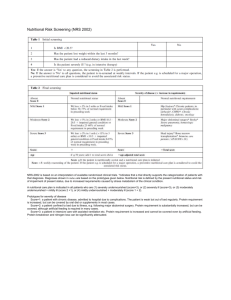
Nutrition and Dietetics in the Normal Patient Study Aims Definition Malnutrition Actual body weight Ideal body weight Predicted body weight Nutritional assessement Calculation of nutritional needs Complications of overfeeding Introduction Malnutrition common Predisposition to Defined as 10% of USUAL body weight Delayed healing Post-operative Infection Added Morbidity and Mortality Recognition thus important Preventable disease Treatable disease Introduction (cont . . .) Usual / actual body weight Ideal body weight As measured by scale Male Female H2 * 20 H2 * 25 Predicted body weight Male Female 50 + 0.91 (Height in cm – 152.4) 45.5 + 0.91 (Height in cm – 152.4) Nutritional Assessment 1. History and examination 2. Anthropological markers 3. Biochemical markers 4. Calculations of energy and protein requirements Nutritional Assessment History Pre- morbid conditions Estimates the risk of malnutrition Hepatic and renal failure IBD Cancer and HIV/AIDS Burns and head injuries Conditions that limit intake or increase output History of recent weight loss Dietary Hx Intake concerning calory (energy), protein, vitamin and trace elements Nutritional Assessment Physical Examination Caloric intake Protein status Subcutaneous fat of buttocks and extremities Extremity muscle bulk and strength Temporal wasting Vitamin intake Changes in skin, mucosa and skin appendages Skin texture change Cheilosis and glossitis Peripheral neuropathy ect Nutritional Assesement Physical Examination (cont . . . ) Trace elements Sx similar to vitamin def + menal changes Nutritional Assessment History and physical examination The above determines the risk for malnutrition Guidelines for identifying patients at risk Weight Overweight (BMI 30) and underweight (BMI < 18) Weight loss more than 10% actual weight Alcoholics NPO more than 5 days Medication with anabolic effect / antinutrient porp Nutritional Assessment Anthropological Markers Body Mass Index (BMI) Weight (kg) / height 2 Gross overweight is a risk for malnutrition Skinfold thickness (SFT) < 18 underweight < 10 Severely malnouraged Measures subcutaneous fat and thus energy reserve (10 - 13 mm) Midarm circumference (MAC) Muscle bulk and therefore somatic protein status (22 – 23 cm) Nutritional Assessment Anthropological Markers (cont . . . ) Bio-electrical Impedance Analysis Single frequency models unreliable Dual frequency modes in current clinical assessment Expensive initial outlay Accurate measurement of body composition Nutritional Assessment Biochemical anlysis Serum proteins Estimates visceral protein reserve Overall markers include Overall poor reliability due to complex factors Total serum protein, albumin, tansferrin and total lymphocyte count Due to long half live reflects chronic malnutrition More sensitive markers due to shorter half live Pre-albumin, retinol binding protein, ceruloplasmin Reflects acute changes in nutritional status Nutritional Assessment Biochemical anlysis Nitrogen balance Measures protein synthesis and breakdown Calculations Protein intake is the sum of all nitrogen intake (Enteral and parenteral) Protein breakdown is measured by nitrogen excretion in urine, faeces, fistula ect N intake = g protein / 6.25 N output = (urine urea * urine volume/day(l) * 0.028) + losses (3 – 6g) Balance Positive = anabolism Negative = catabolism Mild 5 – 10g Moderate 10 – 15g Severe 15g Calculation of nutritional needs Energy requirements TE = NPE + PE TE = Total energy requirements, NPE = Non-protein energy,PE = protein energy NPE = Carbohydrate + Lipids PE = 1.2 – 2 g/kg IBW NPE = 25 – 30 Kcal/kg IBW Carbohydrates = 5 g/kg Lipids = 1 – 1.5 g/kg or 20kcal/kg Complications of overfeeding Carbohydrates Glucose oxidation rate No more than 5 mg/kg/min Delivers 4 cal / g or Complications Hyperglycemia and hyper-osmolar states Hapaic steatosis due to lipogenesis Increased CO2 and lactate production Complications of overfeeding Lipids Lipid infusions Maximum rate 1 – 1.5 g/kg Given as short, medium and long chain Delivers 9cal / g Complications of overfeeding Hiperlipedaemia and pancreatitis Fat overload syndrome Immiunological supression HSR Complications of overfeeding Proteins Amino-acid and protein infusion 1.2 – 2 g / kg Delivers 4 cal / g Given as variaty of amino-acids Complication Azothemia