Heart Failure Asma Khalil 27th June 12
Chronic Heart Failure
Asma Khalil ST1
27/6/12
Background
• Heart failure is a complex syndrome in which the ability of the heart to maintain the circulation of blood is impaired
• >50% assoc LVSD (reduced LVEF)
• Rest have preserved EF
?caused by diastolic dysfunction (due to decreased LV filling, with abnormal LV relaxation or distensibility during diastole)
• Normal-abnormal LVEF cut off ranges 40-50%
Background
• 2% of all hospitalized bed-days.
• 5% of all medical emergency admissions.
• GP sees 30 people with HF and suspect new diagnosis in 10 annually
Conditions that damage heart muscle or limit its ability to function normally:
– CAD
– HTN
– Cardiomyopathies.
– Drugs
– Toxins
– Endocrine conditions
– Infiltrative conditions
– Other conditions
(Chagas' disease, HIV infection, end-stage renal failure).
Conditions that reduce cardiac output:
• Increased vascular resistance with HTN.
• Abnormal heart rhythm
• Pericardial disease.
• OSA.
• Aortic stenosis (severe).
Conditions that result in a high cardiac output:
• Anaemia.
• Thyrotoxicosis.
• Septicaemia.
• Liver failure.
• AV shunts.
• Paget's disease.
• Thiamine deficiency.
When to suspect
Symptoms
– Breathlessness
(orthopnoea/PND)
– Fatigue (tiredness, exhaustion, decreased ET
– Fluid retention
Medical and social history
MI, CAD, or angina.
AF, DM, HTN, Excessive alcohol.
Cardiotoxic chemotherapy in the past.
FH of HF or sudden cardiac death from cardiomyopathy at a young age.
Signs
– Laterally displaced apex beat.
– Raised JVP.
– Enlarged liver
– Third or fourth heart sound
– Tachycardia.
– Lung crackles
– Dependent oedema
NYHA classification of heart failure symptoms [AHA 1994]
– Class I: asymptomatic LVD incl:
• No limitations. Ordinary physical activity does not cause fatigue, breathlessness, or palpitation.
– Class II: symptomatically 'mild' HF:
• Slight limitation of physical activity. Comfortable at rest. Ordinary
physical activity results in fatigue, palpitation, breathlessness, or angina pectoris.
– Class III: 'moderate' HF:
• Marked limitation of physical activity. Comfortable at rest but less
than ordinary physical activity will lead to symptoms.
– Class IV: 'severe' HF:
• Inability to carry on any physical activity without discomfort.
Symptoms of cardiac failure are present even at rest.
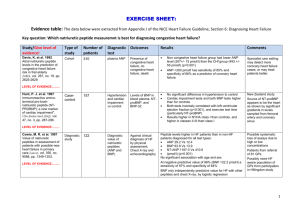
How to Investigate
• No Previous MI natriuretic peptide level — either B-type natriuretic peptide
(BNP) or N-terminal pro-BNP.
• MI in the past
Refer for specialist assessment and echo regardless of natriuretic peptide levels.
• In all 12-lead ECG. Exclude other causes:
– Chest X-ray.
– Blood tests: UEs, Cr, FBC, TFT, LFT, glucose, lipids.
– Urinalysis.
– Lung function tests (peak flow or spirometry).
• Assess for and manage any underlying causes (where appropriate).
Other diagnoses to consider
• Conditions causing SOB
– Chest disease
• COPD
• Asthma.
• Pneumonia.
• Cancer.
– Obesity.
– Volume overload
– Angina.
– Anxiety.
– Anaemia.
– Thyroid disease.
– Being unfit.
• Conditions causing peripheral oedema
– Dependent oedema that is not pathological, for example from prolonged inactivity.
– Nephrotic syndrome.
– Drugs
– Hypoalbuminaemia
– Venous insufficiency.
Be aware that high BNP levels can also be caused by:
LVH, ischaemia, tachycardia, RV overload, hypoxaemia (including PE), GFR < 60 ml/minute, sepsis, COPD, DM, age greater than 70 and liver cirrhosis.
When to refer
• Urgently (within 2 weeks) for specialist assessment and echo:
– previous MI
– Without MI + BNP > 400 pg/mL (116 pmol/L) or NT-proBNP >2000 pg/mL
(236 pmol/L).
– People with severe symptoms (if admission is not indicated).
– Women who are pregnant.
• Within 6 weeks:
– Without MI who have a BNP 100–400 pg/mL (29-116 pmol/L) or NT-proBNP 400–
2000 pg/mL (47–236 pmol/L).
• If natriuretic peptide levels are normal (BNP <100 pg/mL or NT-proBNP <400 pg/mL a diagnosis of HF is unlikely. However, referral may still be needed if:
– Clinical suspicion persists and the person is obese or taking drugs which lower natriuretic peptide levels (diuretics, ACE i, ARB, BB, or aldosterone antagonists).
– Another condition is suspected, which requires referral to a specialist.
• If it is not possible to measure natriuretic peptide levels,refer if:
– ECG is abnormal.
– ECG is normal, but there is still a strong suspicion of heart failure.
Management whilst awaiting specialist assessment
• Review medications (NSAIDs or CCBs).
• Symptoms sufficiently severe to warrant treatment (but not admission), start a loop diuretic:
– Furosemide 20 mg/day to 40 mg/day.
– Bumetanide 0.5 mg/day to 1.0 mg/day.
• If higher doses are required check adherence to treatment, review differential diagnosis, seek specialist advice.
• Seek specialist advise for pregnant women before initiating any drug treatments.
HF + LVSD
• To relieve symptoms of fluid overload = diuretic
• To reduce morbidity and mortality = ACE +/- BB
Use clinical judgement
• BB if angina.
• ACE inhibitor if DM/signs of fluid overload
– ARB if unable to tolerate ACE – cough
– Switch to BB licensed for HF (bisop, nebiv, carved) if already taking one for other co-morbidity
Introduce one drug at a time, and once stable on the first drug, add the second.
– If ACE, start low and titrate, check UE
– CI BB (asthma, heart block, symptomatic hypotension, or COPD disease with reversibility) or intolerance
– CAN give in PVD, erectile dysfunction, DM, interstitial pulm disease).
Check pulse+HR
• Still symptomatic despite optimal treatment with an ACE i (or AIIRA) and
BB?
– Refer for specialist review regarding further drug treatments eg aldosterone antagonists, an ARB + ACE inhibitor, hydralazine + nitrate (especially if the person is of Afro–Caribbean origin), or digoxin
• In all people, consider antiplatelet drug + statin.
– Antiplatelet if atherosclerotic arterial disease
– Statin if atherosclerotic arterial disease or 10-year risk of CV event >
20%
– Consider if anticoagulation therapy with warfarin is indicated eg HF and AF or HF + sinus rhythm and hx of thromboembolism, LV aneurysm, or intracardiac thrombus.
• Review other medications
NSAIDs (fluid retention and renal toxicity), CCB (fluid retention and have no mortality benefit), or antiarrhythmics.
• Consider comorbidities which may influence the treatment of heart failure
Angina/Asthma/COPD/ AF/ DM/ Gout/ Renal impairment
Follow up
Assess and monitor:
1. Psychosocial needs
2. Functional capacity
The NYHA tool.
3. Intercurrent infection
4. Fluid status — assess:
• Change in body weight.
• Jugular venous distention.
• Lung crackles
• Hepatomegaly
• Ascites.
• Oedema
• Hypovolaemia (postural decrease of more than
20 mmHg)
5. Cardiac rhythm —syncopal and presyncopal symptoms, pulse, HR
– If the person has syncope or presyncope (unless clearly due to postural hypotension), refer - this may be due to VT, particularly in people who have LVSD.
– If arrhythmia is suspected? 12lead ECG or arrange 24-hour monitoring.
– If symptoms have deteriorated and pulse is regular, consider doing ECG.
6. Biochemistry — monitoring medications
Referral
• To HF MDT or cardiology service for:
– initial diagnosis of heart failure.
– Severe HF (NYHA class IV)
– HF does not respond to treatment
– HF can no longer be managed effectively in the home setting.
• For specialist advice:
– Women who are planning / who are pregnant.
• For assessment for cardiac resynchronization therapy and an implantable
cardioverter-defibrillator:
– Left ventricular EF 35%
– NYHA class III or IV symptoms
– They are in SR: either with a QRS duration of 150 ms or longer
– or with a QRS duration of 120–149 ms and mechanical dyssynchrony that is confirmed by echo
– Receiving optimal pharmacological therpy
• Specialist advice may be appropriate when managing people with heart failure and a comorbidity
Self-care advice
• Recognize symptoms of HF, and what to do if symptoms deteriorate.
– Breathlessness, tiredness, ankle or abdominal swelling, and rapid weight gain.
– Promptly seek medical attention or adjust the doses of their diuretics
(as pre-agreed), or both.
• Monitor body weight
• Keeping active and physical exercise.
• Stop smoking
• Alcohol
• Restricting salt consumption – no specific guidelines, avoid excess
• Avoiding excessive fluid intake- if severe HF <1.5-2L/day
• Recognise symptoms of dehydration
• Vaccinations (annual influenza, one-off against pneumococcal disease)
Sexual activity
• May be related to CVD, medical treatments (BB), fatigue, or depression.
• Ok if can tolerate moderate exertion without cardiovascular symptoms
• People with NYHA class III or IV symptoms - slightly increased risk of worsening heart failure triggered by sexual activity.
• Phosphodiesterase inhibitors (sildenafil) NOT recommended in advanced HF;
CI nitrates, or nicorandil.
• If stable heart failure:
– Should not use GTN for at least 24 hours before or after taking sildenafil or vardenafil and for at least 48 hours before or after taking tadalafil.
– If they have an episode of angina during sexual intercourse, they must not use
GTN. They should stop sexual activity and, if their pain does not resolve, they should call for an ambulance.
• Some people may benefit from referral to a sexual dysfunction clinic.
Driving
• See DVLA website for the latest information regarding medical fitness to drive
• It is the person's responsibility to inform the DVLA of any condition that may affect their ability to drive.
• The DVLA's medical rules regarding heart failure are:
– For group 1 entitlement (cars, motorcycles)
• Continue, provided no symptoms that may distract the driver's attention.
• The DVLA need not be notified.
– For group 2 entitlement (lorries, buses)
• The person is disqualified from driving if symptomatic.
• Re-licensing may be permitted, provided that the left ventricular ejection fraction is at least 40% and there is no other disqualifying condition.
• Exercise or other functional testing may be required, depending on the likely cause of the heart failure.
• For people with ICDs, the DVLA has specific recommendations
• People should check with their insurer that they are still covered for driving.
Travel
Advise the person that:
– Most can safely travel by air, if condition is stable.
• Readiness to fly should be considered in the context of any comorbidities and the severity of HF
– People who have severe heart failure (NYHA class III or IV) should inform the airline of their condition, so that:
• Special consideration can be given to them (for example provision of a wheelchair and preferential access onto the aeroplane).
• Oxygen is available if the person should need it during the flight
(there may be a charge for in-flight oxygen).
– Advise the person of the importance of continuing to take their medication regularly when travelling.
Prognosis
• Difficult to estimate for an individual:
– HF does not evolve gradually, but has stable periods interrupted by episodes of acute destabilization.
– depends on the cause of the heart failure, the person's age, comorbidities + adherence tx
• Poor. About 50% of people with HF die within 4 years of diagnosis, approx 40% of people admitted to hospital with heart failure die or are readmitted within 1 year
Online resources
• Living with heart failure
– www.bhf.org.uk
— the British Heart Foundation.
– www.heartfailurematters.org
— the European Society of Cardiology.
• Salt in the diet
– www.bhf.org.uk
— the British Heart Foundation.
– www.bda.uk.com (pdf) — the British Dietetic Association.
• Coronary heart disease
– www.heartforum.org.uk
— the National Heart Forum.
• Planning ahead, and end-of-life issues
– www.endoflifecareforadults.nhs.uk
— the NHS National End of Life Care Programme supports the implementation of the UK Department of Health's End of Life Care Strategy by sharing good practice in collaboration with local and national stakeholders.
References
• NICE guidelines Chronic Heart Failure
• Clinical Knowledge Summaries
• European Society of Cardiology (2008) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008.
• National Clinical Guideline Centre for Acute and Chronic Conditions 2010