Thyroid Storm Case Study
advertisement

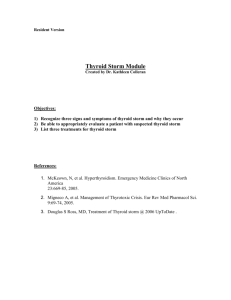
Thyroid Storm Case Study -Develop knowledge of the etiologies, manifestations, and treatment of endocrine and metabolic disorders. -Demonstrate understanding of the common endocrine abnormalities, especially regarding presentation, initial evaluation and management, and disposition. Presentation • The patient is a young, otherwise healthy woman accompanied by her husband with a history of Graves Disease, diagnosed three months prior. The husband has brought her into the Emergency Department from home due to what he thinks is a “severe panic attack.” The patient is visibly jittery, crying, upset. She reports a lack of sleep. She does appear extremely anxious. • The patient has become pregnant and has not as yet had her first prenatal visit. She has been non-complaint with her medication methimazole, due to her concerns over the medication’s effect on her pregnancy. Physical Assessment: • • • • Tachycardia Atrial Fibrillation (irregular rapid pulses) Hypertension Rales • What else do you want? 180/110 170 94% RR up to 30 CBC, chem panel normal TSH <0.002 B Blocker treatment • • • • • • • • • • • • • Complications: intrauterine growth retardation, prolonged labor, neonatal bradycardia, hypotension, hypoglycemia, prolonged hyperbilirubinemia, evaluate the risk-to-benefit analysis [4] Consider: Esmolol (cardioselective) Metoprolol Atenolol Propranolol Assessment • History patient gives: been nervous, etc. for the past week, with symptoms worsening • Patients initial exam: febrile, agitated, diarrhea , • Patients physiology: sinus tachychardic, soft and smooth skin Assessment • Discussion with patient reveals that she has not been overly concerned about her Grave’s disease, she only came to the hospital because she is trying to get pregnant and doesn’t want to be sick, doesn’t take her medicine because she thinks it will decrease her chances of getting pregnant • CT chest reveals thickened left ventricle • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Burch and Wartofsky Predictive Clinical Scale for Thyroid Storm Parameter taken into consideration Scoring Points Thermoregulatory dysfunction Temperature (Oral, ºF) 99-99.9 5 100-100.9 10 101-101.9 15 102-102.9 20 103-103.9 25 >104 30 CNS Effects Absent 0 Mild (agitation) 10 Moderate (delirium, psychosis, extreme lethargy) 20 Severe (seizures, coma) 30 GI-hepatic dysfunction Absent 0 Moderate (diarrhea, nausea, vomiting, abdominal pain) 10 Severe (unexplained jaundice) 20 Tachycardia (beats/min) 99-109 5 110-119 10 120-129 15 130-139 20 >140 25 Congestive Cardiac Failure Absent 0 Mild (pedal edema) 5 Moderate (bibasal rales) 10 Severe (pulmonary edema) 15 Atrial Fibrillation Absent 0 Present 10 Precipitating Events Absent 0 Present 10 ≥45: highly suggestive of thyroid storm 25-44: suggestive of impending storm <25: unlikely to represent thyroid storm Pathophysiology • Hyperthyroidism includes diseases that are a subset of thyrotoxicosis that are caused by excess synthesis and secretion of thyroid hormone by the thyroid. These diseases are not associated with exogenous thyroid hormone intake or subacute thyroiditis. (See Etiology.) • Thyrotoxicosis is the hypermetabolic condition associated with elevated levels of free thyroxine (FT4) and/or free triiodothyronine (FT3). Treatments • Many of the neurologic and cardiovascular symptoms of thyrotoxicosis are relieved by betablocker therapy. Prior to therapy, examine the patient for signs and symptoms of dehydration that often occur with hyperthyroidism. After oral rehydration, beta-blocker therapy can be started. Do not administer beta-blocker therapy to a patient with a significant history of asthma. Calcium channel blockers can be used for the same purposes when beta blockers are contraindicated or poorly tolerated. • Antithyroid Drugs • Antithyroid drugs (eg, methimazole, propylthiouracil) have been used for hyperthyroidism since their introduction in the 1940s. They are employed for the long-term control of hyperthyroidism in children, adolescents, and pregnant women (propylthiouracil only for pregnancy). In women who are not pregnant, the medications are used to control hyperthyroidism prior to definitive therapy with radioactive iodine. In surveys of thyroid specialists in the United States, the preferred treatment of hyperthyroidism is radioactive iodine therapy. • Antithyroid medications inhibit the formation and coupling of iodotyrosines in thyroglobulin, which are necessary for thyroid hormone synthesis, leading to a gradual reduction in thyroid hormone levels over 2-8 weeks or longer. A second therapeutic action of propylthiouracil, but not methimazole, is the inhibition of conversion of T4 to T3. T3 is a more biologically active form of thyroid hormone. A quick reduction in T3 is associated with a clinically significant improvement in thyrotoxic symptoms. • Titrate the antithyroid drug dose every 4 weeks until thyroid functions normalize. Some patients with Graves disease go into a remission after treatment for 12-18 months, and the drug can be discontinued. Notably, half of the patients who go into remission have a recurrence of hyperthyroidism within the following year. Nodular forms of hyperthyroidism (toxic multinodular goiter and toxic adenoma) are permanent conditions and will not go into remission. • The drug of choice for hyperthyroidism in the nonpregnant woman is methimazole. The recent US Food and Drug Administration (FDA) boxed warning for increased liver failure with propylthiouracil has limited its use to just the first trimester of pregnancy. Methimazole has rarely been associated with cloacal and scalp (cutis aplasia) abnormalities when given during early gestation. Generally, if a women desires pregnancy, the patient is switched to propylthiouracil. After the 12 weeks of gestation, the patient is switched back to methimazole. Methimazole is a more potent and longer-acting drug. Often, patient compliance is better with methimazole taken once or twice daily than with propylthiouracil given 3-4 times daily. • Propylthiouracil is still the drug of choice in uncommon situations of life-threatening severe thyrotoxicosis because of the additional benefit of inhibition of T4 -to-T3 conversion. Administer propylthiouracil every 6-8 hours. The reduction in T3, which is 20100 times more potent than T4, theoretically helps to reduce the thyrotoxic symptoms more quickly than does methimazole. Once thyroid levels are decreasing toward normal, the patient can be switched to methimazole therapy. Should we give the B blocker? • Consider the risks/benefits… We have given a B Blocker and restarted her methimazole. Vital signs have improved • Give an SBAR to the floor…