Fever in a returned traveller
Ouli Xie
Intern
Fever in a returned traveller
• 30 year old man presents with fever 38.5C
associated with abdominal pain
– Returned 2 months ago from a 3 week trip to India
– Multiple exposures and no travel prophylaxis
– Associated with 2 days of loose bowels but now
BNO for 2 days
– Some nausea but no vomiting
• PHx: Nil
• Meds: Nil
Examination
•
•
•
•
•
•
Haemodynamically stable, T 38.5C
Diaphoretic, unwell looking
Fluid depleted
Dual heart sounds, no murmur
Chest clear to auscultation
Tender RIF on palpation, but abdomen soft
DDx?
• Malaria
• Bacterial enteritis
• Inflammatory bowel disease
• Appendicitis!
An approach
•
•
•
•
•
•
•
History
Travel/exposure history
Examination
Common causes of fever
Causes not to miss
Investigations
Treatment
History
• Time course is essential
– Including progression of illness
• Incubation period can help
distinguish illnesses
– Dengue unlikely after 2 weeks
• Associated features
– Rash, headache, GI symptoms,
myalgia/arthralgia etc.
Exposure history
• T – travel – specific places and dates
rural/urban
• O – occupation
• A – activities – detailed list of activities
animals, fresh water, food etc.
• D – drugs – including IVDU
• S – sex
Causes
• Travel specific
– Malaria
– Dengue
– Bacterial enteritis
• More prevalent in area of travel
– Influenza
– Respiratory illnesses
• General causes of fever
– Appendicitis etc.
The big 3
• Malaria
• Typhoid
• Dengue
Malaria
• Caused by mosquito-borne protozoan
– Plasmodium falciparum
– Plasmodium ovale
– Plasmodium vivax
– Plasmodium malariae
– Plasmodium knowlesi
• Carried by dawn/dusk biting Anopheles
mosquito
• Multiple stages in life cycle
Malaria life cycle
http://www.cdc.gov/malaria/about/biology/
Characteristic features
• Falciparum malaria can be fulminant and
cause death
• Ovale and vivax have dormant liver stages and
may reactivate
• Malariae may have low levels of parasetaemia
and recrudesce weeks after infection
• Characteristically described as cyclical fevers
Falciparum malaria
• The most common cause of symptomatic
malaria
• Risk of complicated malaria
– Systemic symptoms or high level of parasetaemia
>5%
• Incubation 12-14 days
• Associated with high levels of chloroquine
resistance
Complicated malaria
• Systemic symptoms or high parasetaemia
–
–
–
–
–
–
–
–
–
Altered conscious state +/- seizures
ARDS
Circulatory collapse
Metabolic acidosis
Renal failure or haemaglobinuria
Haptic failure
Coagulopathy +/- DIC
Severe anaemia
Hypoglycaemia
http://courses.washington.edu/med620/mechanicalventilation/
case3answers.html
Clinical features
• Hx
– High cyclical fevers
– May have non-specific
associated features including:
• Headache, cough,
nausea/vomiting, diarrhoea,
abdo pain, myalgias/arthralgias
• Examination
– Splenomegaly
– Jaundice
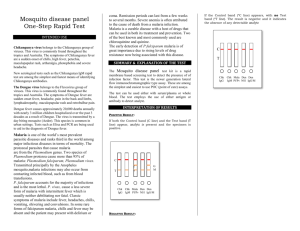
Diagnosis
• Thick and thin films
– Operator dependent
– Serial films required
• Rapid diagnostic tests
– ICT used at RMH
(immunochromatographic test)
– Used to detect malaria antigens
– Can distinguish between
Falciparum and non-falciparum
malaria
– Sensitivity and specificities ~95%
Treatment
• Artesunate is the preference for treatment of
falciparum malaria
– 3 day course of artemether-lumefantrine
– IV form available for severe falciparum malaria
• Always given in combination to prevent
resistance
• Non-faciparum malaria can be treated with
chloroquine if sensitive
– Note primaquine required for liver stage of vivax and
ovale
Dengue
•
•
•
•
4 serotypes
Carried by day-biting mosquito Aedes aegypti
Usually not lethal
Risk of dengue haemorrhagic fever
– Infection with 1 serotype results in super-antigen
response
– Circulatory collapse and
haemorrhage/coagulopathy
Dengue clinical features
• History
– Fever, arthalgias, myalgias and
severe headache (often retroorbital)
– “Breakbone fever”
– Maculopapular rash
• Examination
http://en.wikipedia.org/wiki/Dengue_fever
– Non-specific
– May find some lymphadenopathy,
rash, hepatomegaly
Diagnosis and treatment
• Basic bloods
– Classically shows a thrombocytopaenia and
leukopaenia
• Diagnosis
– Dengue serology
– Dengue PCR/ELISA
• Treatment
– Supportive
Enteric fever
• Typhoid/paratyphoid fever
• Caused Salmonella enterica serotype Typhi or
serotype paratyphi
• Faecal-oral spread
• Typhoid Mary
– Can be associated with chronic carriage
– Colonisation of biliary system
• Incubation 5-21 days
Clinical features
• Hx
– Classic progression described
• Rising fever in first week
• Abdo pain in second week with
appearance of rash
• Septic shock in third week
– May describe constipation or
diarrhoea
• Exam
http://www.zipheal.com/typhoid/typhoid-fever-symptoms/3761
– Characteristic rose spot rash
– Abdo pain, hepatosplenomegaly
Investigations
• Basic investigations
– May demonstrate a leukocytosis or leukopaenia
– Abnormal LFTs even in hepatitic pattern
• Diagnosis
– Blood culture (+ve in 40-80%)
– May also be cultured in stool or urine
– Serology minimal value
Treatment
• Supportive treatment
• Antibiotic therapy
– Azithromycin or ceftriaxone
– Ciprofloxacin useful if susceptible
– Beware resistance against fluoroquinolones in
South/South-East Asia
Summary
• Take a careful history
• Remember that fever in returned traveler
does not have to be a travel related illness!
• Remember the big 3 – malaria, dengue and
enteric fever
• Time course can often be the key
References
• Uptodate
• Yung, Allen P (2005). Infectious diseases : a
clinical approach (2nd ed). IP
Communications, East Hawthorn, Vic
• Kumar P and Clark M (Eds) (2009) Kumar and
Clark’s Clinical Medicine (7th edition).
Edinburgh: Saunders Elsevier.