Lessons for Anaesthesia
advertisement

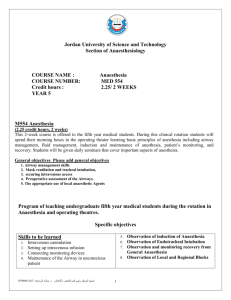
Lessons for anaesthesia Steve Yentis: London 9th Dec 2014 Paul Clyburn: Edinburgh 12th Dec 2014 Mike Kinsella: Belfast 22nd Jan 2015 Anaesthetic direct deaths pre-2009 n.b. previous 20 years: 20-50 direct deaths per year 9 8 7 6 n % 5 4 3 2 1 0 1985-87 1988-90 1991-93 1994-96 1997-99 2000-02 2003-05 2006-08 Direct deaths Triennium attrib. to anaesthesia % Direct deaths Rate per 100 000 maternities 95% CI 1985-87 6 4.3 0.26 0.12 0.58 1988-90 4 2.8 0.17 0.07 0.44 1991-93 8 6.3 0.35 0.18 0.68 1994-96 1 0.7 0.05 0.01 0.26 1997-99 3 2.8 0.14 0.05 0.42 2000-02 6 5.7 0.30 0.14 0.66 2003-05 6 4.5 0.28 0.13 0.62 2006-08 7 6.5 0.31 0.15 0.64 2009-11 3 3.6 0.12 0.03 0.37 2010-12 4 5.1 0.17 0.05 0.43 Comparing changes in anaesthetic deaths • • • • Small numbers Deaths are often complex Difficult to attribute to one cause Previously some deaths ?arbitrarily attributed to anaesthesia • Easy to overlook important anaesthetic lessons in ‘non-anaesthetic deaths’ → Hence ‘Lessons for Anaesthesia’ Lessons for anaesthesia • Anaesthetic reviewers looked at all 203 deaths – very many examples of good practice – areas where improved anaesthetic care may have affected outcome • No. of direct anaesthetic deaths remain low (4) • Clear that anaesthetists should be involved in critical periods of care in high-risk women • Need to be proactive not reactive Anaesthetic lessons from direct deaths Complications after PDPH • Two women with post-dural puncture headache – one managed with blood patch – one managed conservatively • Not followed up or referred to GP • Persistent headache for weeks • Emergency presentation – cavernous venous sinus thrombosis – subdural haematoma Complications after PDPH • Lessons: – women with PDPH should be followed up – GP should be notified – PDPH is not the only cause of headache – serious neurological symptoms / signs require urgent appropriate referral / imaging – inter-hospital transfer of woman with reduced consciousness requires medical supervision – appropriate prescription of anti-VTE prophylaxis is a team responsibility Hypoventilation • Two women had prolonged hypoventilation during or following GA for PPH – both overweight – one possible severe bronchospasm after induction – one following extubation + long delay before re-intubation • Airway problems + fixation error • Inadequate post-operative monitoring Hypoventilation • Lessons: – awareness of fixation errors; use of simulation – value of practice drills of common emergencies • severe bronchospasm / mechanical obstruction • difficult or oesophageal intubation – uniform standards of postoperative monitoring – recognition of hypoventilation – adequate volume replacement in (ongoing) haemorrhage [Anaphylaxis] • Peri- / post-mortem tryptase is often elevated → Hence elevated peri-mortem tryptase does not necessarily indicate anaphylaxis Collapse after anaesthesia • Two cases of collapse shortly after receiving bupivacaine – one following epidural top-up – one following wound infiltration with 100 mg • Prompt management incl. use of lipid rescue • Not attributed to anaesthesia but highlights ever-present risk Collapse after anaesthesia • Lessons: – be prepared to deal with adverse effects of LA – availability of Intralipid and protocols – sudden collapse can occur at any time and the cause not always apparent – prompt action & good teamwork / communication important in managing unexpected catastrophe Hyperkalaemia • • • • • Pre-eclampsia with mild renal impairment C-section under spinal anaesthesia Given postoperative diclofenac Found to be hyperkalaemic Not treated immediately → cardiac arrest Hyperkalaemia • Lessons: – hyperkalaemia is a medical emergency & requires immediate treatment – NSAIDS contraindicated in impaired renal function Anaesthetic lessons from other cases Teamworking & crisis management • Human factors remain an important issue – communication between and within teams – leadership – fixation errors • Lessons: – need for ongoing (multidisciplinary) training – place of simulation Uterine displacement • Often not mentioned, or mentioned but initiated late • ‘Out of hospital’ use inconsistent • Lesson: – ambulance staff should be trained to apply and record uterine displacement during transfer Early warning scores • Sometimes poorly recorded or not acted upon • Lessons: – if EWS are in use, they should be applied and acted upon – compliance with EWS requires auditing Abdominal pain • Severe abdominal pain (not due to labour) requiring opioids often associated with severe underlying condition • Lesson: – pregnant women with severe abdominal pain need senior medical review including anaesthetic Recognition of critical illness • Failure to recognise critical illness • Doses of iv induction agents (especially thiopentone) sometimes felt to be excessive for critically ill women • Lessons: – continued training in recognising critical illness – improved training in use of thiopentone – ?continued place of thiopentone in obstetrics Management of major cases • Inadequate preparation for / management of long procedures & major haemorrhage – temperature measurement & warming – invasive monitoring – appropriate volume replacement • Lesson: – basic principles of anaesthesia for major surgery should be applied Serious Untoward Incident investigations • SUIs sometimes inadequate • Frequently no anaesthetist on panel • Lesson: – All SUI investigations of pregnant and postpartum women should include an obstetric anaesthetist Conclusions • No. of directly attributed deaths remains low • Focus on drawing out lessons from all cases • Much good practice with detailed reflection by anaesthetic teams • Anaesthetists are integral members of multidisciplinary obstetric care & must be involved proactively • Important to appreciate human factors • Anaesthetists must be involved in SUI investigations Acknowledgements • All anaesthetic assessors • All ICM assessors • OAA & RCoA