Part 1
advertisement

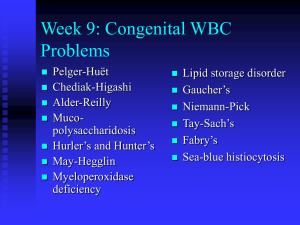
Year Two Review Part 1 Eric Niederhoffer SIU-SOM Outline • • • • • • • • • • • Newborn screening Glycolytic pathway Pentose phosphate pathway Fructose pathway Pyruvate metabolism and citric acid cycle β-Oxidation Urea cycle Branched-chain amino acids Aromatic amino acids Cholesterol pathway Steroid pathway Newborn Screening • • • • • • • • • • • • • • • • • • • • Amino acid disorders Arginemia/arginase deficiency Arginosuccinyl CoA lyase deficiency Citrullinemia/argininosuccinate synthetase deficiency Homocystinemia/cystathionine β-synthase deficiency Maple syrup urine disease Phenylketonuria Tyrosinemia Fatty acid oxidation disorders Carnitine transporter deficiency Carnitine/acylcarnitine translocase deficiency Carnitine palmitoyl transferase deficiency Type 1 Carnitine palmitoyl transferase deficiency Type 2 Glutaric acidemia Type 2 Long-chain 3-hydroxyacyl CoA dehydrogenase deficiency Medium-chain acyl CoA dehydrogenase deficiency Short-chain acyl CoA dehydrogenase deficiency Short-chain 3-hydroxyacyl CoA dehydrogenase deficiency Trifunctional protein deficiency Very long-chain acyl CoA dehydrogenase deficiency Newborn Screening • • • • • • • • • • • • • • • • • • • • • Organic acids disorders β-Ketothiolase deficiency Glutaric acidemia Type 1 Glutaric acidemia Type 2 Holocarboxylase synthetase deficiency 3-Hydroxy-3-methylglutaryl CoA lyase deficiency Isobutyryl CoA dehydrogenase deficiency Isovaleic aciduria Methylmalonic acidemia Methylmalonic acidemia with homocystinuria Propionic acidemia 3-Methylcrotonyl CoA carboxylase deficiency 2-Methylbutyryl CoA dehdrogenase deficiency Other disorders α-Thalassemia Congenital adrenal hyperplasia Cystic fibrosis Critical congenital heart disease Congenital hypothyroidism Galactosemia Sickle cell disease Glycolytic Pathway glucose Hexokinase (glucokinase) ATP glucose-6-phosphate Glucose phosphate isomerase fructose-6-phosphate Phosphofructokinase-1 ATP fructose-1,6-bisphosphate Aldolase Aldolase Triose phosphate isomerase dihydroxyacetone phosphate glyceraldehyde-3-phosphate Bisphosphoglycerate mutase 1,3-bisphosphoglycerate 2,3-bisphosphoglycerate NAD+ Glyceraldehyde-3-phosphate dehydrogenase NADH 3-Phophoglycerate kinase 2,3-Bisphosphoglycerate phosphatase ATP 3-phosphoglycerate Phosphoglycerate mutase 2-phosphoglycerate Enolase phosphoenolpyruvate Pyruvate kinase Lactate dehydrogenase lactate pyruvate NAD+ NADH ATP Glycolytic Pathway Disorders • Hexokinase – rare autosomal recessive, nonspherocytic hemolytic anemia. • Phosphoglucose isomerase – rare autosomal recessive, hemolytic anemia, less common neurological problems. • Phosphofructokinase – (Glycogen storage disease type VII; Tarui disease) rare autosomal recessive, three subtypes (classic, infantile onset, and late onset), myoglobinuria, hyperuricemia, hemolytic anemia when erythrocyte isoform is involved. Avoid high carbohydrate meals. • Adolase – rare autosomal recessive, three genes (ALDOA, mainly muscle; ALDOB, mainly liver, some kidney and intestine; ALDOC, mainly brain), ALDOA has myopathy and hemolytic anemia. ALDOB (hereditary fructose intolerance) vomiting, hypoglycemia, failure to thrive, cachexia, hepatomegaly, jaundice, coagulopathy, coma, renal Fanconi syndrome, severe metabolic acidosis, treat by restricting fructose. • Triosephosphate isomerase – rare autosomal recessive, congenital hemolytic anemia, progressive neuromuscular dysfunction, susceptibility to bacterial infection, and cardiomyopathy. • Glyceraldehyde-3-phosphate dehydrogenase – rare autosomal recessive, very little information available. Glycolytic Pathway Disorders • Bisphosphoglycerate mutase/phosphatase – rare, hemolytic anemia, polycythemia, increased hemoglobin affinity for O2. • Phosphoglycerate kinase – rare X-linked recessive, two forms, chronic hemolytic anemia, myopathic (myoglobinuria) with muscle symptoms especially upon exercise. • Phosphoglycerate mutase – rare autosomal recessive, mainly affects skeletal muscle. • Enolase – rare autosomal recessive, affects muscle, exercise intolerance. • Pyruvate kinase – autosomal recessive, most common inherited cause of nonspherocytic hemolytic anemia (normochromic, normocytic, and reticulocytosis), pallor, jaundice, fatigue, dyspnea, tachycardia and splenomegaly. Treatment is primarily supportive, avoid impact sports with splenomegaly, avoid large doses of salicylates, supplement with folic acid and B vitamins, use blood transfusions with decreased hemoglobin concentrations. • Lactate dehydrogenase – rare autosomal recessive, two forms, LDHA is mainly skeletal muscle, LDHB mainly heart muscle, LDH is tetramer of combination of LDHA and LDHB subunits. LDHA deficiency symptoms include fatigue, muscle pain, exercise intolerance, rhabdomyolysis, and myoglobinuria. LDHB deficiency is asymptomatic. Pentose Phosphate Pathway Glucose-6-phosphate dehydrogenase Lactonase 6-phosphogluconate glucose-6-phosphate 6-phosphoglucono-δ-lactone NADP+ NADPH 6-Phosphogluconate dehydrogenase NADP+ NADPH ribulose-5-phosphate Transketolase fructose-6-phosphate Ribulose phosphate 3 epimerase glyceraldehyde-3-phosphate Ribose-5-phosphate isomerase xylulose-5-phosphate ribose-5-phosphate Transketolase Transaldolase erythrose-4-phosphate sedoheptulose-7-phosphate fructose-6-phosphate glyceraldehyde-3-phosphate Pentose Phosphate Pathway Disorders • Glucose-6-phosphate dehydrogenase – X-linked recessive, most common diseaseproducing enzymopathy, hemolytic anemia most often triggered by bacterial or viral infections, oxidative drugs (sulfonamides and malarials), or eating fava beans (favism). Treatment is supportive, bed rest and oxygen, avoid triggers (drugs, diet, environmental). • Ribose-5-phosphate isomerase – very rare (single report), leukoencephalopathy and peripheral neuropathy. • Transketolase – very rare (single report), liver cirrhosis and hepatosplenomegaly. Fructose Pathway fructose Fructokinase ATP fructose-1-phosphate Aldolase B glyceraldehyde Triose phosphate isomerase dihydroxyacetone glyceraldehyde-3-phosphate phosphate Triose kinase ATP Fructose Pathway Disorders • Fructokinase – autosomal recessive, benign. • Aldolase B – autosomal recessive, (hereditary fructose intolerance) vomiting, hypoglycemia, failure to thrive, cachexia, hepatomegaly, jaundice, coagulopathy, coma, renal Fanconi syndrome, severe metabolic acidosis. Treatment by restricting fructose intake. Pyruvate Metabolism and Citric Acid Cycle lactate Lactate dehydrogenase NAD+ pyruvate Pyruvate dehydrogenase NADH acetyl-CoA Pyruvate carboxylase 2ATP NADH Citrate synthase oxaloacetate citrate Malate dehydrogenase Aconitase NAD+ malate isocitrate NAD+ Fumarase Isocitrate dehydrogenase NADH α-ketoglutarate NAD+ fumarate α-Ketoglutarate dehydrogenase Succinate dehydrogenase succinate FADH2 succinyl-CoA Succinyl-CoA synthetase FAD+ GTP GDP NADH Pyruvate and Citric Acid Cycle Disorders • Pyruvate dehydrogenase – rare, mostly sporadic, X-linked recessive (E1 α-subunit), autosomal recessive (X protein and E3 subunit), developmental delay, intermittent ataxia, poor muscle tone, abnormal eye movements, seizures (all dependent on amount of residual enzyme activity, <15% incompatible with life), increased serum and CSF lactate and pyruvate concentrations, increased serum and urine alanine; for E2 enzyme deficiency, hyperammonemia and increased nonspecific serum amino acid concentrations; for E2 enzyme deficiency, increased serum branched-chain amino acids concentrations, increased serum and urine α-ketoglutarate concentrations, enzyme assays on leukocytes, fibroblasts. Treatment by limiting carbohydrates and increasing fats, supplement with thiamine, carnitine, and lipoic acid. • Pyruvate carboxylase – rare, autosomal recessive, poor feeding, vomiting, and lethargy, Mental, psychomotor, growth retardation, poor or degenerative neurologic development, metabolic acidosis, increased serum lactate and pyruvate concentrations, increased serum lactate to pyruvate concentration ratio, decreased serum glucose during fasting, hyperalaninemia, hypercitrullinemia, hyperlysinemia, and decreased serum aspartic acid concentrations, hyperammonemia, increased CSF lactate, pyruvate, glutamic acid and proline concentrations, decreased CSF glutamine concentrations, enzyme assay of leukocytes or culturedfibroblasts, absence of pyruvate carboxylase mRNA. Treatment with thiamine, lipoic acid, dichloroacetate, citrate, and aspartic acid. Pyruvate and Citric Acid Cycle Disorders • Lactate dehydrogenase – rare autosomal recessive, two forms, LDHA is mainly skeletal muscle, LDHB mainly heart muscle, LDH is tetramer of combination of LDHA and LDHB subunits. LDHA deficiency symptoms include fatigue, muscle pain, exercise intolerance, rhabdomyolysis, and myoglobinuria. LDHB deficiency is asymptomatic. • α-Ketoglutarate dehydrogenase – autosomal recessive, psychomotor retardation, hypotonia, ataxia and convulsions (symptoms of Leigh syndrome), sudden death, myocardiopathy, hepatic disorders, hyperlactacidemia, increased serum glutamine concentrations, increased urine glutaric acid, enzyme assay of leukocytes, fibroblasts. • Succinate dehydrogenase – autosomal recessive, four subunit genes (SDHA, SDHB, SDHC, SDHD), SDHA leads to encephalomyopathy, other genes associated with tumour formation, enzyme assay of leukocytes, fibroblasts. • Fumarase – very rare, autosomal recessive, microcephaly, severe developmental delay, distinctive facial features, brain malformation, seizures, failure to thrive, hypotonia, increased urine fumarate, succinate, citrate, enzyme assays of cultured fibroblasts, lymphoblasts, or white blood cells, molecular genetic testing. Treatment is supportive. β-Oxidation palmitate Very long chain = C14 to 20 Long chain = C10 to 14 carnitine shuttle palmitoyl-CoA (C16) Medium chain = C6 to 10 FAD Acyl-CoA dehydrogenase FADH2 trans-𝚫2-enoyl-CoA enoyl-CoA dehydratase acetyl-CoA C4 C6 C8 C10 C12 L-3-hydroxyacyl-CoA NAD+ L-3-Hydroxyacyl-CoA dehydrogenase NADH 3-ketoacyl-CoA myristoyl-CoA (C14) thiolase acetyl-CoA CoASH β-Oxidation Disorders • Medium-chain acyl CoA dehydrogenase – autosomal recessive, preprandial irritability, lethargy, jitteriness, sweating, seizures, tachypneic, somnolent, mildly enlarged liver, decreased serum bicarbonate concentration, increased serum anion gap, hypoglycemia, hypoketonuria, hyperammonemia, increased urine monocarboxylic fatty acids and dicarboxylic organic acids (adipic, C6; suberic, C8; sebacic, C10; and dodecanedioic,C12), enzyme assay, molecular genetic testing. Treatment with increased calories from carbohydrates and protein, limited fats, avoid periods of fasting. • Very long-chain acyl CoA dehydrogenase – autosomal recessive, cardiomyopathy, hypotonia, hepatomegaly, hypoketotic hypoglycemia, increased serum C14:1, C14:2, C14, and C12:1 straight-chain acyl-carnitine esters, 3-hydroxy-acyl carnitine esters, and unsaturated acyl-carnitine esters, enzyme assays, molecular genetics testing. Treatment with increased calories from carbohydrates and protein, medium-chain triglycerides, avoid periods of fasting. • Long-chain 3-hydroxyacyl CoA dehydrogenase – autosomal recessive, cardiomyopathy, hypotonia, hepatomegaly, hypoketotic hypoglycemia, decreased serum carnitine, increased serum 3-hydroxydicarboxylic derivatives of the C16:0, C18:1, and C18:2 species, increased urine 3-hydroxylated dicarboxylic acids, enzyme assay, molecular genetics testing. Treatment with increased calories from carbohydrates and protein, medium-chain triglycerides, avoid periods of fasting. Urea Cycle aspartate acetyl CoA + glutamate citrulline argininosuccinate Argininosuccinate N-Acetylglutamate synthetase synthase Ornithine CoA HCO3 transcarbamoylase N-acetylglutamate ⊕ Argininosuccinate Carbamoyl phosphate lyase synthetase carbamoyl phosphate arginine H2O Arginase + NH4 ornithine urea Urea Cycle Disorders • N-Acetylglutamate synthase – very rare autosomal recessive, lethargy, poorlycontrolled breathing rate or body temperature, seizures, coma, hyperammonemia, increased serum alanine and glutamine urine orotic acid within reference range. Treatment is low protein intake. • Carbamoylphosphate synthetase – rare, autosomal recessive, early-onset lethargy, seizures, hyperammonemia, serum ammonia concentrations are usually 10-20 times higher than reference range. Treatment is reduced protein intake, increased carbohydrates and lipids, and glycerol phenylbutyrate to reduce ammonia concentrations when appropriate. • Ornithine transcarbamoylase – rare, X-linked recessive, early- or late-onset, lethargy, poorly-controlled breathing rate or body temperature, seizures, hyperammonemia, increased urine orotic acid, enzyme assays. Treatment is restricted protein intake, increased carbohydrates and lipids, and glycerol phenylbutyrate to reduce ammonia concentrations when appropriate. Urea Cycle Disorders • Argininosuccinate synthetase – rare, autosomal recessive, two forms (type I more common than II). Type I lethargy, poor feeding, vomiting, seizures, and loss of consciousness, type II confusion, restlessness, memory loss, abnormal behaviors (such as aggression, seizures, and coma, hyperammonemia, increased serum citrulline, increased urine orotic acid, enzyme assay of cultured fibroblasts. Treatment is restricted protein diet and glycerol phenylbutyrate to reduce ammonia concentrations when appropriate. • Argininosuccinate lyase – rare, autosomal recessive, lethargy, poorly-controlled breathing rate or body temperature, seizures, hyperammonemia, increased serum and urine argininosuccinic acid, increased serum citrulline, glutamine, alanine, and lysine, increased urine orotic acid, enzyme assay of cultured fibroblasts. Treatment is low-protein diet, arginine supplementation and glycerol phenylbutyrate to reduce ammonia concentrations when appropriate. • Arginase – very rare (least common urea cycle defect), autosomal recessive, delayed development, protein intolerance, spasticity, hyperammonemia (sometimes), assay for erythrocyte arginase activity. Treatment is low-protein diet and administration of oral sodium benzoate or sodium phenylbutyrate to reduce ammonia concentration when appropriate. Branched-Chain Amino Acids isoleucine Aminotransferase α-keto-β-methylvalerate valine leucine Aminotransferase α-ketoisovalerate Aminotransferase α-ketoisocaproate Branched-chain α-ketoacid dehydrogenase α-methylbutyl CoA isobutyl CoA isovaleryl CoA propionyl CoA 3-hydroxy-3-methylglutaryl CoA Propionyl CoA carboxylase D-methylmalonyl CoA HMG CoA lyase L-methylmalonyl CoA Methylmalonyl CoA mutase succinyl CoA acetoacetate Branched-Chain Amino Acid Disorders • Branched-chain α-ketoacid dehydrogenase – rare, autosomal recessive, newborn screening, poor feeding, vomiting, lethargy, and developmental delay, sweet odor of affected infants' urine, increased serum leucine and isoleucine concentrations, increased alloisoleucine concentrations by day 6, increased urine alpha-hydroxyisovalerate, lactate, pyruvate, and alpha-ketoglutarate concentrations, enzyme assay of lymphocytes or cultured fibroblasts (not necessary for diagnosis). Treatment is dietary restriction of branched-chain amino acids and supplementation of thiamine as appropriate. MSUD Express for juveniles and adults. • Propionyl CoA carboxylase – autosomal recessive, failure to thrive due to feeding intolerance and vomiting, ketoacidosis, dehydration, shock, increased serum anion gap and ketones, decreased urine pH, increased urine β-hydroxy propionic acid, lactic acid, and methylcitrate concentrations, enzyme assays of leukocytes. Treatment with restriction of branched-chain amino acids. Branched-Chain Amino Acid Disorders • Methylmalonyl CoA mutase – autosomal recessive, seizure, encephalopathy, stroke, hypotonia, lethargy, failure to thrive, hepatosplenomegaly, increased serum ammonia, glycine, propionic acid, and methylmalonic acid concentrations, increased urine methylmalonic acid, methylcitrate, propionic acid, and 3-hydroxypropionate concentrations. Treatment with protein restriction and carnitine supplementation. • 3-Hydroxy-3-methylglutaryl CoA lyase – rare, autosomal recessive, vomiting, diarrhea, dehydration, lethargy, hypotonia, non-ketotic hypoglycemia, metabolic acidosis, increased serum 3-hydroxy isovaleryl-carnitine and 3-methylglutaryl-carnitine concentrations, increased urine 3-hydroxy-isovaleric, 3-methylglutaric, glutaric, 3-methyl-glutaconic, 3hydroxy-3-methyl-glutaric acids and 3-methyl-crotonyl-glycine concentrations. Treatment with limiting fasting periods, low-leucine diet, and supplementation of carnitine. Aromatic Amino Acids phenylalanine Phenylalanine hydroxylase tyrosine Aromatic amino acid decarboxylase homogentisate dopamine norepinephrine epinephrine Tyrosinase Homogentisate oxidase 4-maleylacetoacetate DOPA quinone fumarylacetoacetate Fumarylacetoacetase acetoacetate fumarate Aromatic Amino Acid Disorders • Phenylalanine hydroxylase – autosomal recessive, newborn screening, fair skin and hair, intellectual disability, musty or mousy odor, epilepsy, extrapyramidal manifestations, eye abnormalities, increased serum phenylalanine concentrations. Treatment with phenylalanine restriction. • Aromatic amino acid decarboxylase – very rare, autosomal recessive, severe developmental delay, hypotonia, muscle stiffness, difficulty moving, athetosis, lethargy, feed poorly, startle easily, sleep disturbances, oculogyric crises, increased CSF L-dopa, 5hydroxytryptophan and 3-orthomethyldopa concentrations, decreased CSF homovanillic acid and 5-hydroxyindoleacetic acid concentrations, enzyme assay. Treatment with vitamin B6, dopamine agonists, and MAO inhibitors. • Tyrosinase – rare, autosomal recessive, oculocutaneous albinism, hair and skin depigmentation, decreased visual acuity, photophobia, iris transillumination, nystagmus, pigment deficiency in the peripheral retina, enzyme assay of hair bulb, molecular genetic testing. Treatment with nitisinone and address visual problems. • Homogentisate oxidase – rare, autosomal recessive, alkaptonuria, excreted urine becomes black in color, arthritic symptoms confined chiefly to the spine, hips, and knees, increased urine homogentisic acid concentrations, polymerase chain reaction test. Treatment with vitamin C and reduction of dietary phenylalanine and tyrosine. • Fumarylacetoacetase – rare, autosomal recessive, cabbagelike) odor, renal tubular dysfunction, failure to thrive, increased serum tyrosine and methionine concentrations, increased urine succinylacetone concentrations, aminoaciduria. Treatment with nitisinone and low-tyrosine, low-phenylalanine diet. 3-hydroxy-3-methylglutaryl CoA Cholesterol Pathway 7-dehydrocholesterol Δ7-reductase cholesterol HMG CoA reductase Δ24-reductase Δ24-reductase mevalonate Mevalonate kinase 7-dehydrodesmosterol Δ7-reductase desmosterol Δ5-dehydrogenase phosphomevalonate cholesta-7,24-dien-3β-ol Δ8,Δ7-isomerase isopentenyl pyrophosphate lathosterol farnesyl pyrophosphate Squalene synthase squalene lanosterol zymosterol Cholesterol Pathway Disorders • Mevalonate kinase – rare, autosomal recessive, less- and more-severe types, less-severe (Hyperimmunoglobulinemia D syndrome) has fever episodes with lymphadenopathy, abdominal pain, joint pain, diarrhea, skin rashes, and headache, more-severe (Mevalonic aciduria) has (fever or no fever) developmental delay, progressive ataxia, progressive problems with vision, and failure to gain weight and grow at the expected rate, unusually small, elongated head, increased serum immunoglobulins A and D concentrations (lesssevere type), increased urine excretion of mevalonic acid, enzyme assays. Treatment is supportive. • 7-Dehydrocholesterol reductase (3β-Hydroxysteroid-Δ7-reductase) – autosomal recessive (Smith-Lemli-Opitz syndrome), dysmorphic facial features, microcephaly, second-toe and third-toe syndactyly, intrauterine growth retardation, short stature, abnormally low weight for height, hypotonia, distinctive shrill cry, decreased serum cholesterol concentrations, increased serum dehydrocholesterol concentrations. Treatment is supportive. • Δ8,Δ7-isomerase – X-linked dominant (CHILD syndrome), dysmorphic facial features, microcephaly, second-toe and third-toe syndactyly, intrauterine growth retardation, short stature, abnormally low weight for height, hypotonia, distinctive shrill cry, decreased serum cholesterol concentrations, increased serum dehydrocholesterol concentrations. Treatment is supportive Steroid Pathway cholesterol Desmolase (CYP11A1) 17-Hydroxylase (CYP17A1) 17-Hydroxylase (CYP17A1) pregnenolone 17α-hydroxypregnenolone dehydroepiandrosterone 3β-Hydroxysteroid dehydrogenase 3β-Hydroxysteroid dehydrogenase 3β-Hydroxysteroid dehydrogenase progesterone 17α-hydroxyprogesterone androstenedione 17-Hydroxylase (CYP17A1) 17,20-Lyase (CYP17A1) Aromatase 21-Hydroxylase 21-Hydroxylase 17-Ketoreductase (CYP21A2) (CYP21A2) 11-deoxycorticosterone 11-deoxycortisol 11-Hydroxylase (CYP11B1) testosterone 11-Hydroxylase (CYP11B1) Aromatase estrone 17-Ketoreductase corticosterone estradiol Aldosterone synthase (CYP11B2) aldosterone 5α-Reductase cortisol dihydroxytestosterone Steroid Pathway Disorders • Desmolase – very rare (lipoid adrenal hyperplasia), autosomal recessive poor weight gain, vomiting, males are undervirilized, dehydration, hyperpigmentation, increased serum ACTH, hyponatremia, hyperkalemia, metabolic acidosis. Treatment with saline and fludrocortisone, female also with estrogen replacement. • 17-Hydroxylase – very rare (congenital adrenal hyperplasia), autosomal recessive, patients with XX or XY karyotypes are phenotypic females or ambiguous genitalia, hypertension, hypokalemia, metabolic alkalosis, increased serum progesterone, corticosterone, and deoxycorticosterone concentrations, decreased 17-hydroxyprogesterone, estrogens, and androgens concentrations. Treatment with glucocorticoid and estrogen replacement, salt restriction, diuretics as appropriate. • 3β-Hydroxysteroid dehydrogenase – very rare (congenital adrenal hyperplasia), autosomal recessive, ambiguous genitalia or female genitalia, hyperpigmentation, increased serum 11-deoxycortisol and deoxycorticosterone, increased ratio of 24-hour urine metabolite of 11-deoxycortisol to metabolite of cortisol. Treatment with glucocorticoid and mineralocorticoid therapy as appropriate. Steroid Pathway Disorders • 21-Hydroxylase – very rare (most common congenital adrenal hyperplasia), autosomal recessive, males have failure to thrive, recurrent vomiting, dehydration, hypotension, hyponatremia, hyperkalemia, shock, accelerated growth and skeletal maturation; in addition, females have ambiguous genitalia at birth, later in childhood with precocious pubic hair, clitoromegaly, increased serum 17-hydroxyprogesterone concentrations, increased urine pregnanetriol concentrations. Treatment with glucocorticoid and mineralocorticoid therapy as appropriate. • 11-Hydroxylase – very rare (congenital adrenal hyperplasia), autosomal recessive, androgen excess, masculinization of female newborns and precocious puberty in male children, hypertension, increased serum 11-deoxycortisol and deoxycorticosterone, urine 17ketosteroids, dehydroepiandrosterone, dehydroepiandrosterone sulfate, and androstenedione, and testosterone. Treatment with glucocorticoid replacement and antihypertensive therapy. • Aromatase – very rare, autosomal recessive, virilization manifests as pseudohermaphroditism in female infants, affected males do not present with obvious defects at birth, tall stature, delayed skeletal maturation, delayed epiphyseal closure, bone pain, eunuchoid body proportions and excess adiposity, increased serum testosterone concentrations. Treatment with estrogen replacement. Steroid Pathway Disorders • Aldosterone synthase – rare, autosomal dominant, autosomal recessive, severe saltwasting in infancy or stress-induced hyperkalaemia and postural hypotension in adulthood, increased serum renin activity, decreased serum aldosterone concentrations, increased serum 18-hydroxycorticosterone. Treatment with mineralocorticoid therapy (fludrocortisone) and sodium supplementation. • 5α-Reductase – rare, autosomal recessive, ambiguous genitalia, clitoral-like phallus, markedly bifid scrotum, pseudovaginal perineoscrotal hypospadias, rudimentary prostate, uterus and fallopian tubes are absent, testes are intact and usually found in the inguinal canal or scrotum, amniocentesis or chorionic villus sampling show XY karyotype, fluorescent in situ hybridization results positive for sex-determining region, increased serum testosterone-todihydrotestosterone ratio, molecular genetics studies. Treatment considerations of gender assignment. • 17-Ketoreductase – rare, autosomal recessive, characterized by clitoromegaly, posterior labioscrotal fusion and perineal blind vaginal pouch, testes are inguinal or in the labioscrotal folds, internal urogenital tract (epididymides, vasa deferentia, seminal vesicles, ejaculatory ducts) well developed; prostate and Müllerian structures are absent, baseline and post-human chorionic gonadotropin stimulation hormonal evaluation shows increased androstenedione and decreased testosterone concentrations, with an increased androstenedione-totestosterone ratio. Treatment considerations of gender assignment.