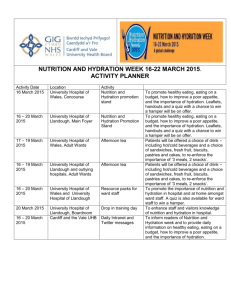
Nutrition and Hydration workshop
advertisement
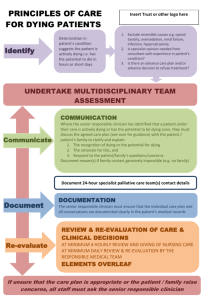
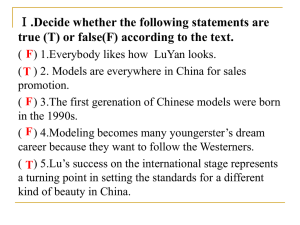
Post Liverpool Care Pathway End of Life Conference 14th May 2014 Nutrition and Hydration Presented by Catriona Brooks and Carolyn Stapely Macmillan Dietitians at WSHFT Aim of this session To empower you to feel confident with managing food and drink concerns at the end of life…… Diagnosing dying is not easy – it is not a precise science Accurate prediction in non-cancer patients is especially difficult as there is no accurate way of telling when it’s the last few days of life This makes knowing what’s the right thing to do even harder for health care professionals Are they allowed to eat and drink? If so, what can we give them? How much should we give them? Their oral intake is poor, should we start them on artificial nutrition or hydration? Nutrition at the end of life Should we be maintaining a nutrition care plan? Weight / MUST / food charts etc? What do we tell the family when they ask what we are doing about their relatives poor food and fluid intake? Should we refer them to the Dietitian due to their poor dietary intake? Is there any evidence available to support what we are doing? Will they die in discomfort from hunger or thirst? Are we affecting the dying process by giving / withholding food or fluids? The length of the dying process depends on which cells are deprived of oxygen – reducing organ function Changes in respiration, loss of sphincter control, reduction in blood perfusion and renal function Loss of ability to swallow due to neurological dysfunction increasing risk of choking Weakness and fatigue - sleep more to conserve energy What happens physiologically when we die? Gastric emptying, digestion and absorption and peristalsis decline. This reduces the body’s ability to be able to tolerate food Lose the desire to eat and drink – loss of appetite can happen weeks before last hours of life. There are many causes for this, most of which become irreversible close to death. Will they die in discomfort from hunger or dehydration? Loss of appetite is normal and hunger is not felt. Food is often not appealing or may be nauseating. People who are dying will eat and drink if they want to. Ketosis due to reduced food intake may help to enhance a euphoric effect which can calm the person and help with pain. Most experts believe that dehydration in the last hours of life does not cause distress and may stimulate endorphin release which adds to the persons sense of well being Studies have shown that terminally ill patients do not experience hunger or thirst and for those that do this is satisfied with small amounts of food and sips of fluid Recent study (Bruera, Hui et al.) comparing 100ml subcutaneous fluid with 1L saline found no difference in fatigue, sedation, hallucination, muscle spasm or overall survival between the groups Dry mouth is usually due to mouth breathing and medications and can be effectively managed with good mouth care What do we tell the family when they ask what we are doing about their relatives poor food and fluid intake? Check that the family know that their relative is dying and help them understand what happens physiologically when we die, so that they can start to understand why their relative is not eating or drinking much. Let the relatives and family know what you are doing to keep their loved one comfortable and how they can help with this too. Suggest other activities that encourage touch and being present. Are they allowed to eat and drink? What can we give them? How much should we give them? ☺Always offer food and drink – rarely do people need to be strictly NBM ☺Take into consideration the personal and cultural preferences of the individual and their family ☺ Focus on personal choice, taste and tolerance rather than the nutrient content ☺ Encourage independence (OT,SLT, Dietitian) ☺ Small quantities are better tolerated – may only be a few mouthfuls or sips ☺ Provide help with eating and drinking ☺ Softer food consistencies may be better tolerated ☺ Sucking on ice lollies or ice chips may relieve a dry mouth ☺ Optimise the presentation of food and drink so that it looks good. Think about the size of plates, cups, crockery etc. to make eating/drinking easier ☺ Nutritional supplements are often unnecessary unless desired Are we affecting the dying process by giving/withholding food or fluids? The offer of food and drink by mouth is part of basic care as is the offer of washing and pain relief. It must always be offered to patients who are able to swallow without serious risk of choking or aspiration. There is a genuine concern that dehydration accelerates death particularly in the elderly and frail where maybe their symptoms resemble dying We know that if you withhold fluids death usually occurs within 3-14 days Withholding food alone with adequate hydration death occurs within 57-90 days There is very little good quality research to answer this question Much of the research that is available particularly focuses on the use of clinically assisted nutrition and hydration (rather than food or drink by mouth) – but even with this research it is often not of good quality. The majority of people who are imminently dying do so comfortably without the assistance of CAN/CAH. In the last days the lack of food or fluid will not contribute to the death. Good communication with the medical teams, patient, family and carers is essential to ensure patients get the right care. Clinically Assisted Nutrition and Hydration (CAN/CAH) The law does not distinguish CAN from any other forms of medical treatment. A medical treatment is started for a specific purpose and discontinued when failing to achieve or maintain this purpose. In patients where death is believed to be inevitable and where nutrition intervention is not considered to be of benefit, it can be withdrawn or withheld. Cochrane reviews have examined evidence on the effects of CAN/CAH upon the quality and survival length of palliative care patients. To date there remains insufficient good quality trials to make any recommendations for routine practice. It therefore remains unknown whether this treatment helps people to live longer or feel better. Clinicians therefore need to make decisions based on the perceived benefits and harms of CAN/CAH in individual patient circumstances. REFERENCES British Medical Association (2007) Withholding and withdrawing life-prolonging medical treatment: Guidance for decision making. London. Blackwell publishing Good P, J Cavenagh et al. (2008a) “Medically assisted nutrition for palliative care in adult patients” Cochrane Database Systematic Review 4 Good P, J Cavenagh et al. (2008b) “Medically assisted hydration for palliative care in adult patients” Cochrane Database Systematic Review 2 Treatment and Care Towards the End of Life: Good practice in decision making. (2010) GMC. Royal College of physicians and British Society of Gastroenterology (2010) Oral feeding difficulties and dilemmas: A guide to practical care particularly towards the end of life. London: Royal College of Physicians. Bruera, ED. Hui, et al. (2013) “Parenteral hydration in patients with advanced cancer: A multicentre, double-blind, placebo controlled randomised trial” Journal of Clinical Oncology 31(1): 111-118 Parry et al. (2013) Evidence Briefing Pathways for the Dying Phase in End of Life Care Independent review of the Liverpool Care Pathway. More Care Less Pathway (2013) https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverp ool_Care_Pathway.pdf Leadership Alliance for the Care of Dying people. Engagement with patients, families, carers and professionals. (2013) Gateway reference no:00616 To conclude… “Palliative care affirms life but recognises dying as a natural process; neither intentionally hastening nor postponing death”