Sideroblastic anemias
advertisement

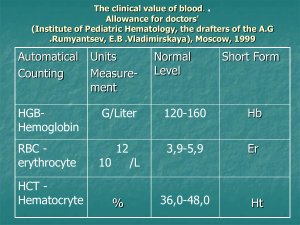
Faculty of Applied Medical Sciences Department Of Medical Lab. Technology 2nd Year – Level 4 – AY 1433-1434 Sideroblastic anemia, Anemia of chronic disease & Lead Poisoning Mr. Waggas Ela’as, M.Sc, MLT 1 Identify, classify and know the pathogenesis of Sideroblastic anemia. Identify ring sideroblasts, and their presence in the bone marrow. List the lab findings of Sideroblastic anemia Identify, classify and know the pathogenesis of anemia of chronic diseases. List the lab findings of anemia of chronic diseases. Express the lead poisoning and its route . Identify Basophilic stippling found in Sideroblastic anemia & lead poisoning. (iron incorporated in erythroblasts is not used to form Haem, so it is deposited in mitochondria that make a ring around the nucleus) (Disturbances of enzymes regulating heme synthesis) I. (more common) – MDS(Myelodysplastic syndrome) : (Nutritional deficiencies (copper, vitamin B6),Lead poisoning, Zinc overdose, Alcohol, Drugs (eg, antituberculous agents, antibiotics), Idiopathic) Iron overload Capacity of serum transferrin to bind iron is exceeded Non-transferrin-bound iron (NTBI) circulates in the plasma Excess iron promotes the generation of free hydroxyl radicals, propagators of Excess iron promotes tissue damage oxygen-related tissue damage Cardiac failure Liver damage or cancer Diabetes mellitus Growth failure * (interferes with the activity of the enzyme deltaaminolevulinic acid dehydratase) * Basophilic stippling of erythrocytes in lead poisoning 14 Anemia of chronic disease (ACD) * ACD is a common type of anemia that occurs in patients with infectious, inflammatory, or neoplastic diseases that persist for more than 1 or 2 months. * Probably it is the second most common form of anemia. (what is the 1st most common form?) * ACD is the most common cause of anemia in hospitalized patients. 15 Chronic infections : tuberculosis, lung abscess, sub acute endocarditis Non infectious inflammatory diseases : rheumatoid arthritis, systemic lupus erythematosus. Neoplastic Disorders : Hodgkin`s disease, lung and breast carcinoma. 16 1. Shortened red cell life span (from 120 to 60-90 days) 2. Relative bone marrow(erythropoiesis) failure: - Cytokines released from inflammatory cells (TNF-, IL-1, IFN-) affects erythropoiesis by inhibiting the growth of erythroid progenitors. 3. ABNORMAL IRON METABOLISM activation of the reticuloendothelial system with increased iron retention and storage within it. impaired release of iron from macrophages to circulating plasma transferrin. 17 The anemia is usually mild or moderate ( Hb 7-11g/dl) The anemia is most often normochromic and normocytic (MCHC and MCV are normal) (but in one third of the cases it presents as hypochromic microcytic) Iron metabolism 1. Serum Iron - decreased (it is necessary for the diagnosis of ACD) 2. TIBC - reduced 3. Transferrin saturation(TS) – normal/ decreased 4. Serum Ferritin-increased / normal 18 19 20 The bone marrow structure and cellularity on biopsy and aspiration, are generally normal, except for alterations occasioned by underlying disease. So the bone marrow examination is rarely done for diagnosis of ACD. 21 Unlike other hypochromic anaemias, BOTH serum iron & TIBC are low in ACD. 22 The causes of hypochromic microcytic anemia include iron deficiency, thalassemias and other genetic disorders of hemoglobin, the anemia of chronic disorders, sideroblastic anemia, and lead poisoning. These causes may be differentiated by special tests, including measurement of serum iron, total iron-binding capacity, and serum ferritin. Iron Deficiency Anemai Thalassemia Sideroblastic Anemia Anemia of Chronic Diseases Smear Microcytic Hypochromic Microcytic Hypochromic Microcytic Hypochromic Normoctic Normochromic˃ Microcytic Hypochromic Serum Iron (50150 μg/dl) Low Normal Normal Low TIBC (300-600 μg/dl) High Normal Normal Low Serum Ferritin 50-200 μg/l) Low High High Normal OR High Hb pattern Normal Abnormal Normal Normal % Saturation (30-50%) Low Normal OR High Normal OR High Low