Geriatric Medicine Update for General Practitioners
advertisement

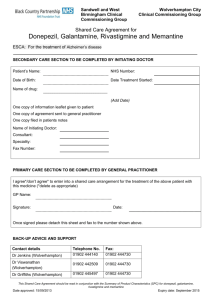
Geriatric Medicine Update Dr Elena Mucci ConsultantPhysician/Geriatrician Leadership Tutor October 2013 Is the approach to HTN in the elderly different? HYVET trial • HYVET: 3845 subjects, 80+ and functional – SBP > 160; goal 150/80 – Indapamide and ACEi vs. Placebo 30% reduction in all cause mortality • ABP Substudy (112 subjects at baseline) – Mean CBP 172/90 mm Hg – No orthostasis – Mean daytime ABP: 136/78 – Mean 24 hr ABP: 133/77 Beckett NS, NEJM, 2008; 358: 1887‐1898 Bulpitt CJ, Hypertension, 2013; 61: 89‐94 Anticoagulation and Fall Risk Should we be prescribing anticoagulants in patients with fall risk? • Prospective study ▫ 515 pts, median age 71, treated w/ vitamin K antagonists ▫ Fall risk associated with risk for major bleeding? ▫ High fall risk if: fall in past yr, gait/balance/mobility issue ▫ 60% were high risk • Outcomes ▫ No difference in time to first major bleeding event including fatal or intracranial within 12 months f/u. ▫ Risk for major bleed independently associated with polypharmacy. • 12% increased risk for each additional drug taken. Am J Med 2012. PMID: 22840664 Anticoagulation and Fall Risk • Take Home Point: ▫ Patient > 65 yrs with CHADS2 score of 2-3 would have to fall 295 times yearly for risk of fall-related SDH to outweigh benefits of stroke prevention. ▫ Polypharmacy greater risk. ▫ Use this opportunity to stop unnecessary medications. Aspirin to prevent recurrent DVT • Recurrence of unprovoked VTE after stopping anticoagulants ▫ 5-15% at one year, 30-50% at 5-10 yrs ▫ Highest risk: male, mod-severe post-thrombotic syndrome, proximal DVT, elevated D-dimer 3-4 weeks after stopping therapy. • Extending anticoagulants associated with increased risk of bleeding. • Is the use of low dose aspirin an alternative? Low Dose Aspirin for prevention of recurrent DVT • Double blind placebo controlled RCTs • WARFASA (402 pts) and ASPIRE (822 pts) Trials ▫ Pts with first unprovoked VTE who stopped anticoagulation after 6-18 months of therapy. ▫ Randomized to ASA 100 mg daily vs. Placebo • VTE recurrence ▫ Pooled data from both trials ▫ 32% reduction in rate of recurrent VTE ▫ 34% reduction in rate of major vascular events ▫ Low risk of bleeding NEJM 2012. PMID: 22621626, 23121403, 231 21404 Update on drugs commonly used in the Elderly • Omeprazole impairs absorption of calcium, iron, and levothyroxine • Omeprazole is a cause of acute interstitial nephritis • Omeprazole can cause B12 deficiency • Omeprazole contributes to C Dif and delays recovery • Fenofibrate and losartan significantly lower serum uric acid levels • Longterm use of metformin may result in significant B12 deficiency • Trimethoprim causes reversible elevation of serum creatinine and potassium AF and new anticoagulatnts • Dabigatran, direct Thrombin inhibitor, 110mg BD; 150 mg BD, 75mg BD if eGFR 15-30, renal excretion. Non inferior to warfarin. • Rivaroxaban, 10a inhibitor, 20mg OD, 15mg OD in renal disease, also licensed for PE/DVT, renal/liver excretion. Non inferior to warfarin. • Apixaban, 10a inhibitor, 5mg BD and 2.5 mg BD, mainly liver excretion-safer in renal disease. The only one which showed reduction in all cause mortality, including reduction in major bleeding, GI bleeding-no difference. AF, rate control • RACE II • Goal heart rate <80bpm vs. <110bpm • Permanent atrial fibrillation • <80 years of age • Resting atrial fibrillation rate >80bpm • Primary outcome composite: – Death from cardiovascular causes – Hospitalization for heart failure – Stroke or systemic embolism – Major bleeding – Arrhythmic events including syncope or VT – Implantation of pacemaker or ICD • Van Gelder et al. NEJM 2010;362:1363-1373 2011 ACC/AHA Updates • Treatment to a goal resting heart rate <80bpm is not beneficial compared to <110bpm in patients with atrial fibrillation who have LVEF >40% and no or minimal symptoms (Class III) Treatment Options • Beta-blockers-sympathetic pathway – Carvedilol less effective than others • Verapamil-Diltiazem • Digoxin-As adjunct only-parasympathetic pathway – Use if heart failure also • Amiodarone-Rarely for rate control • AV node ablation and pacing Diastolic Dysfunction HFpEF • Prevalence: increasing with the aging population and increasing recognition • Systolic HF: CAD, HTN, DM • Diastolic HF: Age, Female, HTN, Obesity • Precipitating factors: labile HTN, Med noncompliance,Diet non-compliance, • Iatrogenenic (NSAIDS, fluids), Infections HFpEF • • • • • • • • • • • Treatment: Class I: Control of BP (<130/80) Agents not specified Control of tachycardia in Afib Reduction of central blood volume-with diuretics Class IIa: coronary revascularization if ischemic Class IIb: Restoration of NSR Digitalis use not well established ACE/ARB/BB/CCB Medications Used to Treat Hallucinations, Delusions and Agitation • Antipsychotics (Black Box Warning!) – Haloperidol – Risperidone – Olanzapine – Quetiapine • Anticonvulsants – Carbamazepine • Antidepressants – Sertraline • Β-adrenergic receptor antagonists – Propanolol • Antianxiety agents – Clonazepam, lorazepam Statin induced Myopathy • Myalgia Normal CK, reduce the dose, try different drug, stop the drug, restart at lower dose or different one. • Myositis Elevated CK, stop the drug till CK/symptoms normalised, restart with a statin with high half life, like Rosuvastatin+/- Co-Enzyme Q10. • Rhabdomyalisis CK 10 times the normal level, myoglobinuria, AKI, death. Stop statin and never use again. Continuation of donepezil in patients with moderate-to‐severe Alzheimer’s disease may improve cognition at 52 weeks. • RCT • 295 community-dwelling patients, mean age 77.1; 65% females; 95% white, mean MMSE 9; taking Donepezil for at least 3 months. • 4 groups: Continue donepezil with placebo memantine Continue donepezil and starting memantine Discontinue donepezil with placebo memantine Discontinue Donepezil an starting Memantine Follow up period 52 weeks Outcome measures: Cognition (SMMSE) and functional status (BADLS) Howard R, McShane R, Lindesay J, Ritchie C et al. Donepezil and Memantine for Moderate-Severe Alzheimer’s Disease. N Engl J Med. 2012 Mar 8;366(10):893-903. Continuation of donepezil in patients with moderateto‐severe Alzheimer’s disease may improve cognition at 52 weeks. • Clinically important difference SMMSE of 1.4 points or more BADL score of 8 points or more • Donepezil v no Donepezil: 1.9 points difference on SMMSE and 3.0 points difference on BADLS. • Memantine v no Memantine: 1.2 points and 1.5 points difference respectively • No difference Donepezil+Memantine Clinical Bottom Lines • NICE 2011: treatment should be continued only when it is considered to be having a worthwhile effect on cognitive, global, functional or behavioural symptoms. • This study suggests that cognitive outcomes can be improved with continuing Donepezil treatment. • What do I do: If patient is on Donepezil I continue If not on any treatment I start on Memantine If on Donepezil and developed severe behavioural problems I stop Donepezil and start Memantine I stop everything in the EoLC Medications to treat mood disorders in dementia • Selection of antidepressant usually based on previous response to the drug: – trazodone (50mg at bedtime) – sedating and useful with agitated depression and insomnia – also consider nortriptyline 10mg at bedtime – Sertraline 25-50mg per day (proven effective in clinical trials, may especially be useful with agitated depression) • May see improvement in sleep and agitation soon after instituting therapy but full relief of depression delayed by 4-6 weeks Medications to treat sleep disturbances • Trazodone 50-100mg po bedtime • Quetiapine begin with 12.5mg bedtime but can work up the dose. Use only if sleep disturbance is severe and associated with agitation. • Avoid usual sleep medications such as zopiclone Medications to treat apathy • May try a low dose of methylphenidate (5– 10mg early morning but never after 2pm) • If depressed, may try a more stimulating antidepressant such as fluoxetine (10mg to begin with) Tight control of DM in NH eligible older adults may be associated with poor outcomes • Cohort study • 367 NH patients with DM, mean age 80 (+/-9) • 67% female. Almost one-third on oral and 50% on insulin, 79% cognitive impairment , mean ADLs 8, follow up 2 years • Outcome measures: functional decline and death at 2 years • 4 groups: less than 7%, 7-8%, 8-9% and over 9% Yau, C. Glycosylated Hb and Functional Decline in Community-Dwelling NHEligible Elderly Adults with DM. J Am Geriatr Soc. 2012 Jul;60(7):1215-21 Clinical bottom lines • HbA1c level of 8-9% appears to be associated with less functional decline or death at 2 years • Current AGS recommends AbA1c target of 8.0% or less for frail elderly adults with limited life expectancy may be lower than necessary to maintain function and delay death for this vulnerable population. • ADA Position Statement suggests a patient-centred approach in the management of type 2 DM and recommends less stringent HbA1c goals. • Although this study was conducted in NH patients, it suggests that clinicians should consider less aggressive glycaemic targets when managing vulnerable older adults.