What is memantine
advertisement
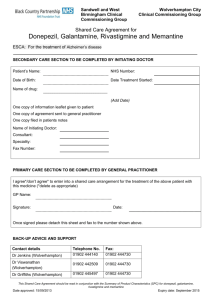
Pharmacy 735 Module 4 Sample Case Presentation 1 Patient Description OH, a 85-year-old female Previously was independent with basic activities of daily living Gradual functional and cognitive decline due to Alzheimer’s Disease, ↑ behavioral disturbances Referred by family physician for inpatient admission to Auckland City Hospital (ACH) geriatrics program for further assessment. 2 Psychiatric and Medical History Axis I: Cognitive impairment due to Alzheimer’s Disease (AD) Diagnosed with AD in 2005 start donepezil March 2007 – switched to rivastigmine May 2007 – moved from home to Silver Birch Lodge July 2007 – switched to galantamine Last MMSE prior to this admission = 9/30 Hypertension Current presentation - Behavioral and psychological symptoms of dementia (BPSDs): wandering, agitation, anxiety, insomnia, paranoia, disinhibition, depression Axis II: Deferred Axis III: Osteoarthritis (knees + shoulder), Osteoporosis, Urinary incontinence, Hypertension, Glaucoma Axis IV: Loss of independence due to cognitive decline Axis V: GAF = 35-40 3 Medications Dementia Galantamine ER 24 mg po in the morning BPSDs Quetiapine 25 mg po daily + 50 mg at bedtime Depression Citalopram 10 mg po daily CVS prevention Enteric Coated Aspirin 81 mg po daily Hypertension Hydrochlorothiazide 12.5 mg + Losartan 50 mg po daily Osteoporosis Calcium elemental 500 mg po BID Vitamin D 1000 IU po daily Alendronate 70 mg po q1wk Glaucoma Timolol XE 0.25% eye drops 1 gtt OS daily 4 Vaccinations Flu yearly, Pneumococcal Alzheimer’s Disease Most common type of dementia Chronic, progressive, irreversible Dementia - Latin “de mens” = “without mind”…? DSM-IV: memory impairment + ≥1 of: Aphasia Apraxia Agnosia Disturbance in executive function Impairs independent daily function Decline from previous level of function NOT due to course of delirium 5 Treatment – Nonpharmacological Family/caregiver education, counseling, support Structured environment Therapeutic alliance between medical team and caregiver(s) Cueing and scheduling Orientation Environmental modification Exercise, physiotherapy, group therapy, music therapy, occupational therapy 6 Treatment Options Pharmacological Medications to slow cognitive decline: Cholinesterase inhibitors (CI) Donepezil (Aricept®) Rivastigmine (Exelon®) Galantamine (Reminyl® ER) NMDA receptor antagonist Symptomatic therapies for BPSDs CIs Memantine Antidepressants Short-term: antipsychotics, benzodiazepines Memantine (Ebixa®) 7 Back to the case… Drug-Related Problems OH is experiencing: worsening cognition and requires optimization of drug therapy for dementia worsening BPSDs and requires optimization of drug therapy OH is at risk of worsening urge incontinence due to an increased dose of galantamine 8 Therapeutic Alternatives Continue galantamine alone Discontinue galantamine and initiate memantine alone (switch) Continue galantamine and initiate memantine (combine) Nonpharmacological measures 9 Clinical Question: “In an elderly patient with AD who is already on galantamine, is the addition of memantine superior to addition of placebo for slowing the rate of cognitive and functional decline?” 10 What is memantine (Ebixa®)? Approved by the US FDA in 2003 for treatment moderate-severe AD Available in New Zealand since Feb 2005 NOT funded by Pharmac NOT on the hospital formulary Cost = approx $180/month 11 Mechanism of Action Glutamate Binds to postsynaptic NMDA receptor Controlled amount of Ca2+ influx Chronically elevated MEMANTINE ↑↑ Ca2+ influx Excitatory signal Excitotoxicity 12 Literature Review Memantine in Moderate-Severe AD Dementia subtype All-cause RCT Winblad 1999 Alzheimer’s Reisberg 2003 Tariot 2004 Van Dyck 2007 Intervention MMSE Mean range MMSE Monotherapy <10 6 Monotherapy 3-14 8 Combination with donepezil Monotherapy 5-14 10 5-14 10 13 Summary of Evidence Moderate-severe AD: small beneficial effect in combination with CI on cognition, function, behavior, and global scales at 6months Some conflicting results in monotherapy RCTs May help agitation Well-tolerated 14 What do the guidelines say? “Memantine is an option for patients with moderate to severe stages of AD” (Gr B, Level 1) “Its use in mild stages of AD is not recommended” (Grade D, Level 1) “Combination therapy… is rational…appears to be safe, and might lead to additional benefits for patients with moderate-severe AD” (Grade B, Level 1) “Patients can be switched from a CI to memantine…based on the judgment of the prescribing physician and the patient (or their proxy)” (Grade B, Level 3) Hogan et al. Alzheimer's and Dementia 2007;3:355-84. 15 Recommendation: Continue galantamine ER at 24 mg po daily Add memantine 5 mg po qAM x 1 week, then 5 mg po BID x 1 week, then 10 mg qAM + 5 mg po qPM x 1 week, then 10 mg po BID 16 Rationale Efficacy? Evidence of efficacy in moderate-severe AD, although effect sizes are small Recent evidence (Van Dyck 2007) show discrepancies in efficacy for monotherapy Benefit in combination with donepezil Patient has trialed other CIs May be helpful for agitation Toxicity? Well tolerated No drug-drug, drug-disease interactions Compliance? – will get med-assist Cost? – family willing and able to pay, eager to try 17 Monitoring Plan - Efficacy Cognition Function/ADLs – weekly no change BPSDs – weekly MMSE = 9/30 @ ~4wk MMSE = 11/30 (7’s), 13/30 (WORLD) @ ~2mo Improvement in sleep, combativeness, agitation Less withdrawn Responded well to environmental/nondrug measures Gradual ↓ of quetiapine Caregiver satisfaction/stress Caregivers report improvement, caregiver satisfaction 18 Monitoring Plan - Toxicity Memantine Ongoing monitoring of: nausea/vomiting, constipation, headache, confusion, worsening of urge incontinence Galantamine Bradycardia – repeat ECG after dose increase Ongoing monitoring of: nausea/vomiting, insomnia, vivid dreams, muscle cramps, fatigue 19 References McShane R, Sastre A, Minakaran N. Memantine for dementia (review). The Cochrane Collaboration 2006;2. Van Dyck CH, Tariot PN, Meyers B, et al. A 24-week randomized, controlled trial of memantine in patients with moderate-severe Alzheimer Disease. Alzheimer Dis Assoc Disord 2007;21(2):136-143. Tariot PN, Farlow MR, Grossberg GT, et al. Memantine treatment in patients with moderate to severe Alzheimer Disease already receiving donepezil: a randomized controlled trial. JAMA 2004;291(3):317-24. Van Dyck CH, Schmitt FA, Olin JT. A responder analysis of memantine treatment in patients with Alzheimer Disease maintained on donepezil. Am J Ger Psych 2006;14(5):428-37. Reisberg B, Doody R, Stoffler A, et al. Memantine in moderate-severe Alzheimer’s Disease. NEJM 2003;348(14):1333-41. Livingston G, Katona C. The place of memantine in the treatment of Alzheimer’s disease: a number needed to treat analysis. Int J Ger Psych 2004;19:929-25. Reisberg B, Doody R, Stoffler A, et al. A 24-week open-label extension study of memantine in moderate-severe Alzheimer Disease. Arch Neurol 2006:63:49-54. Winblad B, Poritis N. Memantine in severe dementia: results of the 9M-BEST study (benefit and efficacy in severely demented patients during treatment with memantine). Int J Ger Psych 1999;14:135-46. 20