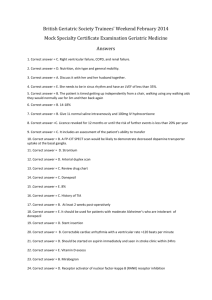
Introduction
advertisement

Introduction:Alzheimer's disease (AD) is one of the most common neurodegenerative diseases, characterized by central cognitive dysfunction, disorder in memory and movement, etc.With the aging of population, more and more people are afflicted with dementia. As reported in World Alzheimer Report 2016, 47 million people are suffering from dementia, and it is estimated to increase to over 132 million by 2050. Tremendous human, material and financial resources have been annually devoted into clinical study and therapy of AD. Funding on treatment of AD in 2015 was 818 billion, and this number will break through one trillion by 2018. However, due to the severity and complexity of AD, few drugs have been clinically applied in curing this disease. Limited number of approved drugs and their poor efficacy lead AD to be incurable. Thus, to surmount this difficulty, numerous researches have put foci on pathology and etiology of AD. Several hallmarks have been reported and verified to be relevant with pathophysiology and progress of this disease, involving multiple systems and factors of nerves, immunity and blood circulation. As demonstrated in many excellent papers, pathological changes and dysfunction of neuro-cholinergic system, b-amyloid (Ab) tangles and aggregations inducing neural apoptosis, tauprotein hyper-phosphorylation forming senile plaque (SP) and neurofibrillary tangles (NFT), neuro-inflammation and increasing level of reactive oxygen radical, etc. are all responsible for the pathogenesis of AD. However, none theory has been clearly claimed to be related with AD. Donepezil As one of the approved drugs for treatment of AD. It generates pharmacological effects by affecting cellular and molecular processes of neuro-degeneration. On account of deficient activity of central cholinergic system, donepezil could inhibit cholinesterase and alleviate neuronal degeneration caused by damage of cholinergic transmission. As a non-competitive and reversible cholinesterase inhibitor of second generation AD drug, donepezil has high selectivity in both targets and tissues. It has been demonstrated in in vitro experiments that donepezil could selectively inhibit AChE 1000-fold against BuChE and the concentration ratio of AChE inhibition in brain and plasma is 6.1e8.4. Donepezil declines the reduction of expression in cerebral cortex and prevents the decrease in nicotinic binding that associated with disease severity. It reduces glutamate neurotoxicity and inhibits excitotoxic injury to maintain neuro-protective actions. Donepezil has potentially confirmed to fight against free radicals and alleviate the effects of oxidative stress in a streptozotocininduced model of AD mice. Donepezil presents significant efficacy in reducing the severity of neuropsychiatric symptoms in patients with mild-to-moderate AD. It can not only impair cognitive dysfunction, but also meet the demand for maintaining or even enhancing a desirable life quality. AD patients with a donepezil regiment were found to better behaved in several tasks, like household appliances, managing personal mail, understanding explanations or new locations, maintaining leisure activities, etc. donepezil cannot completely penetrate blood-brain barrier (BBB). High doses of donepezil may lead to diverse side events, like gastrointestinal upset, nausea, vomiting, diarrhea and muscle cramping. A certain percent of participants did not tolerate even after the dose was reduced. Nevertheless, doses up to 23 mg/day can merely cause side-effects. Although donepezil is an effective, safe, tolerated and meaningful drug approved in market by FDA and widely applied in clinic, it still has various problems. It can only delay AD progression and attenuate the symptoms but cannot terminate the course or completely eliminate the cognitive dysfunction. In other words, donepezil exhibits very limited potential in treatment of severe and advanced AD. Hence, effort to prolong the effective time of donepezil is still in urgent need.