Level 3 - Acute Care Section-APTA
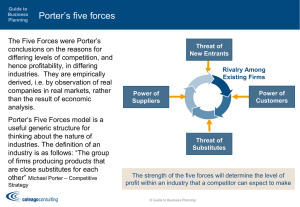
advertisement

ACUTE CARE THERAPISTS CAN SURVIVE AND THRIVE IN UNCERTAIN TIMES Combined Sections Meeting 2015 February 6th, 2015 Indianapolis, IN Speakers Baylor Institute for Rehabilitation System Directors of Acute Care Therapy Services: • Brian Hull, PT, MBA • Cathy Thut, PT, DPT, MBA • Donna Fitch Kaufhold, OTR • Sharon Cheng, PT, MBA, MSPT Course description The current environment of health care reform and cost cutting require hospital therapists take significant steps to manage their culture and actual practice patterns. The physical therapy profession consistently promotes advancement, but are hospital therapy programs consistently following through with true best practice top to bottom? Are hospital therapists aware of health care system politics? Do hospital therapists have strategies to successfully navigate politics and influence change? How is a therapy department viewed by executive leadership in a hospital? How can hospital therapy programs ensure they are seen in a positive light? This course will discuss the urgent need to manage culture to help lead health care reform change in today’s hospitals to avoid becoming irrelevant. Objectives Upon completion of this course, you will be able to: 1. Recognize the impact of health care reform on acute care therapy practice. 2. Determine the correlation between hospital finances and therapy productivity. 3. Evaluate perceptions and its implications to the future of therapy programs. 4. Create strategies to advance professionalism within hospital practice. What Problems are we Facing Today? The Harsh Reality International Comparison of Spending on Health Health Care Expenditure as % of GDP United States 17.7 Norway 11.6 Switzerland 11.6 Canada Denmark Germany France 11.3 11.5 11.6 11.8 2012 The Organisation for Economic Co-operation and Development (OECD) USA Health Care Outcomes Uninsured Rates for Adults Ages 18-64 The Baker Institute 2014 Health Reform Monitoring Survey Texas % Uninsured by Federal Poverty Level The Baker Institute 2014 Health Reform Monitoring Survey Disproportionate Share Hospital Allotments Kaiser Family Foundation 2014 More People and Better Service and Higher Quality and Better Outcomes with Less Money to Pay for it all??? This Is Too Much! How much of this $ is from PT? Where does all the money go? Margin 4.5% Non-Medical Supplies 100.0 Leases, Utilities, Operations 90.0 Depreciation/Interest 80.0 70.0 Medical Services 60.0 Drugs 50.0 Other Expenses 40.0 Physician Expenses 30.0 Medical Supplies 20.0 Purchased Services 10.0 0.0 Salaries/Benefits Hospital Expense Breakdown Where does all the money go? Margin $816 $18,000 Non-Medical Supplies $16,000 Leases, Utilities, Operations $14,000 Depreciation/Interest $12,000 Medical Services $10,000 Drugs $8,000 Other Expenses $6,000 Physician Expenses $4,000 Medical Supplies $2,000 Purchased Services $0 $ Per Discharge Salaries/Benefits Money in my Wallet How much raise do you expect each year? 2% 3% 5% 7% The Universal Equation Total Value Added ______________________________ Total Cost of Services The Universal PT Equation Uncertainty of Total Value Added ______________________________ $92,000 per Acute PT *Source: APTA. http://www.apta.org/WorkforceData/ The Universal Acute PT Equation Uncertainty of Total Value Added ______________________________ $1,988,764,000 The Universal Acute Care Equation Uncertainty of Total Value Added ______________________________ $3,380,908,000 Health Care Expenditure as % of GDP United States 17.7 Norway 11.6 Switzerland 11.6 Canada Denmark Germany France 11.3 11.5 11.6 11.8 2012 The Organisation for Economic Co-operation and Development (OECD) The Universal PT Equation Uncertainty of Total Value Added ______________________________ $92,000 per Acute PT *Source: APTA. http://www.apta.org/WorkforceData/ Productivity! Pop Quiz! When was the theory behind productivity first developed? 1881 1909 1934 1953 The Impressive History of Productivity Measurement Does This Encourage Quality Outcomes? Level 1 Level 2 Level 3 Level 4 Doing What We Do True Best Practice Ideal Hospital Stay Population Management Level 1 Doing What We Do Level 2 Level 3 Level 4 Level 1 Level 2 True Best Practice Level 3 Level 4 Level 1 Level 2 Level 3 Ideal Hospital Stay Level 4 Level 1 Level 2 Level 3 Level 4 Population Management Value added Level 1 Level 2 Level 3 Level 4 Doing What We Do True Best Practice Ideal Hospital Stay Population Management What Do Other People Say About You? What Are You Going to do About It? How other professions see you How do doctors and nurses ask about how patients are doing? How do many PTs answer these simple questions someone asks about the pt? How are you branded? SBAR Situation Background Assessment Recommendation Low Potential Referrals The Universal PT Equation Uncertainty of Total Value Added ______________________________ $92,000 per Acute PT Value added Level 1 Level 2 Level 3 Level 4 Doing What We Do True Best Practice Ideal Hospital Stay Population Management Best Practice? Clinical Practice Guidelines? Evidence Based Practice? Changing Practice Patterns May 2013 June – Oct 2013 Dec 2013 Have we achieved Value – Added Therapy? The Outcome Measure Hierarchy Health status achieved Process of Recovery Tier 1 Tier 2 • Survival • Degree of Health/Recovery • Time to recovery and return to normal activities • Disutility of care or treatment Recurrences Sustainability of health Tier 3 • Sustainability of health/recovery Care induced illness • Long term consequences of therapy Porter, 2010 An Example from our BPG on Falls TiTer Tier 1 1 Tier Tier 2 2 Tier Tier 3 3 • Survival • Degree of Health/Recovery • Time to recovery and return to normal activities • Disutility of care or treatment • Sustainability of health/recovery • Long term consequences of therapy • • • • • • • • • • Mortality Functional level achieved Pain level achieved Return to Prior level of Function Time to treatment Time to return to PLOF Pain, LOS, PE, DVT, delirium Maintain functional level Ability to live independently Loss of mobility due to recurrent falls • Risk of fracture • Reduced mobility Comparison of Pre & Post Data: Falls October & November 2013 January & February 2014 January thru February 1-17, 2014 February 18-28, 2014 Education Education Education Education PT: 0/80 (0.00%) OT: 1/59 (1.69%) PT: 33/77 (42.86%) OT: 12/71 (16.90%) PT: 27/67 (40.30%) OT: 7/63 (11.11%) PT: 6/10 (60.00%) OT: 5/8 (62.50%) Special Test Special Test Special Test Special Test PT: 0/80 (0.00%) OT: 0/59 (0.00%) PT: 39/77 (50.65%) OT: 28/71 (39.44%) PT: 31/67 (46.27%) OT: 21/63 (33.33%) PT: 8/10 (80.00%) OT: 7/8 (87.50%) Pre & Post-Data Results for Falls: Graph Falls Special Testing Falls Education 70% 100% 90% 60% 80% 50% 70% 40% 60% 30% PT 50% PT OT 40% OT 30% 20% 20% 10% 10% 0% 0% Oct & Nov 2013 Jan & Feb 2014 Feb 18 - 28, 2014 Oct & Nov 2013 Jan & Feb 2014 Feb 18 - 28, 2014 National Stats on CPGs • • • • 1/3 are aware of CPGs 13% know how to access 9% have “easy” access < 50% use them frequently Culture Changes Every minute = value It’s all about me It’s only me…. Strategy vs Culture “Culture eats strategy for lunch” ~Peter Drucker “Culture Eats Strategy for Breakfast, Lunch, Dinner and a Midnight Snack” ~Sharon Cheng “In reality, culture does not trump strategy, rather they work together to enhance the success of one another.” ~Mike Myatt Definition of Culture “Culture is the deeper level of basic assumptions and beliefs that are shared by members of an organization, that operate unconsciously and define in a basic ‘taken for granted’ fashion an organization's view of its self and its environment.” ~Edgar Schein Polynesian Culture White Star Lines Best Practice Guidelines Why were we more successful than literature suggests? Roadblocks • Group leaders didn’t understand the goal • Team members new to reading research • Team members were assigned 40-50 articles to read per week Roadblocks • Staff didn’t use existing clinical practice guidelines and systematic reviews • Staff didn’t implement guidelines because too busy and didn’t see the need for them Shifting Culture • Partner therapists strategically • Select your groups purposefully • Keep groups small, 6 to 8 people Shifting Culture • Members should be skilled in critical thinking and group dynamics • The leader should be skilled in keeping the group on task Delancey Street Foundation • Started in 1971 • No government funding • Average resident: – convicted felon – high school dropout – substance abuser – illiterate Delancey Street Foundation Results • Over 10,000 people have received high school equivalency degrees • Over 1000 graduates from their state accredited vocational three-year program How Was It Done? • Teach people to find and develop their strengths • The best way to learn is to teach • Function as an extended family, a community in which every member helps the others Teach people to find and develop their strengths • Who is good at reading research? • Who is clinically experienced? • Who can help these two groups communicate with each other? The best way to learn is to teach • Let your staff do the teaching • You may need to train your staff to teach Function as an extended family, a community in which every member helps the others • The each-one-teach-one process • Use a diverse group of trainers by discipline and generation The Blame Game It’s All Healthcare Reform’s Fault Reality Check • US healthcare is not the best • We cannot sustain the current percentage of GNP for substandard results It’s management’s job to tell us what we need to do Reality Check Therapists have the most knowledge about how to best prioritize patient care I can’t do any more than what I’m doing now Reality Check • You probably can’t do more if you continue to do things the way you have always done them • Are you still focusing on units/visits? • Are you consistently using evidence-based practice? This Change is All About YOU “If you do not change direction, you may end up where you are heading.” ~ Lao Tzu No More Blame Game • Successful people focus on their strengths • The best way to learn is to teach • Function as an extended family, a community in which every member helps the others Therapists Can Add Value • Active participation in decreasing Average Length of Stay (ALOS) • Active leadership in fall reduction • Minimize low potential referrals and treatments • Intervene purposefully using our strengths How YOU Can Survive and Thrive • • • • Define your passion Share with your manager Share with your work support system Share with your home support system What if You are a Team of One? What if You are a Team of Many? How YOU Can Survive and Thrive • • • • Find out if you are a team of one or many Pick your first project Figure out what support you need Ask for support “The greatest danger in times of turbulence is not the turbulence – it is to act with yesterday’s logic.” ~Peter Drucker Contact Info • • • • Brian.Hull@BaylorHealth.edu CathyT@BaylorHealth.edu DonnaFi@BaylorHealth.edu Scheng@bir-rehab.com References Abrahams J, Zucker D., Zucker J., Airplane [DVD]. United States: Paramount Pictures: 1980. By the Numbers. (2014, July). PT in Motion, 64-64. Dunleavy J, Steffes, L. Managing the Transition from Volume to value: Productivity Standards. APTA Webinar Series: April 17, 2014 Federal Medicaid Disproportionate Share Hospital (DSH) Allotments. (n.d.). Retrieved May 5, 2014, from KFF.Org Francke, A. L., Smit, M. C., de Veer, A. J., & Mistiaen, P. (2008). Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC medical informatics and decision making, 8(1), 38. Frederick Winslow Taylor. (n.d.). Retrieved November 4, 2014, from http://www.ibiblio.org/eldritch/fwt/taylor.html Grimshaw, J., Thomas, R., MacLennan, G., Fraser, C., Ramsay, C. R., Vale, L., ... & Donaldson, C. (2004). Effectiveness and efficiency of guideline dissemination and implementation strategies. References Grol, R., & Wensing, M. (2004). What drives change? Barriers to and incentives for achieving evidence-based practice. The Medical Journal of Australia, 180(6 Suppl), S57-60. Ho, V., Marks, E., and Bray, P.G. James A. Baker III Institute for Public Policy, Rice University, The Episcopal Health Foundation, Health Reform Monitoring Survey – Texas, Issue Brief #3. Houston, Texas: 2014. Jette, A. M. (2012). Face into the storm. Physical therapy, 92(9), 1221-1229. K. Davis, K. Stremikis, C. Schoen, and D. Squires, Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally, The Commonwealth Fund, June 2014 Kaplan, R. S., & Porter, M. E. (2011). How to solve the cost crisis in health care. Harv Bus Rev, 89(9), 46-52. Kocher, R. P., & Adashi, E. Y. (2011). Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA, 306(16), 1794-1795. Kotter, John P., and James L. Heskett. Corporate Culture and Performance. New York: Free, 2011. Print. Orszag, P. R., & Emanuel, E. J. (2010). Health care reform and cost control. New England Journal of Medicine, 363(7), 601-603. References Our Accomplishments. Delancey Street Foundation Web site. http://www.delanceystreetfoundation.org/accomplish.php. Published 2007. Accessed November 3, 2014. Ploeg, J., Davies, B., Edwards, N., Gifford, W., & Miller, P. E. (2007). Factors Influencing Best‐Practice Guideline Implementation: Lessons Learned from Administrators, Nursing Staff, and Project Leaders. Worldviews on Evidence‐Based Nursing, 4(4), 210-219. Polynesia’s Genius Navigators. PBS.org Web site. http://www.pbs.org/wgbh/nova/ancient/polynesia-geniusnavigators.html. Published February 15, 2000. Accessed November 4, 2014. Porter, M. E. (2010). What is value in health care?. New England Journal of Medicine, 363(26), 2477-2481. Porter, M. E. This framework paper is Supplementary Appendix 1 to Porter ME. What is value in health care? New England Journal of Medicine, 363(26), 2477-2481. References Porter, M. E. This framework paper is Supplementary Appendix 2 to Porter ME. What is value in health care? New England Journal of Medicine, 363(26), 2477-2481. Pravikoff, D. S., Tanner, A. B., & Pierce, S. T. (2005). Readiness of US nurses for evidence-based practice: many don’t understand or value research and have had little or no training to help them find evidence on which to base their practice. AJN The American Journal of Nursing, 105(9), 40-51. Prior, M., Guerin, M., & Grimmer‐Somers, K. (2008). The effectiveness of clinical guideline implementation strategies–a synthesis of systematic review findings. Journal of evaluation in clinical practice, 14(5), 888-897. RMS Titanic. Titanic Pages: Titanic History Web site. http://www.titanicpages.com/ Published 2007. Updated 2014. Accessed October 3, 2014. Rothstein JM. Thirty-Second Mary McMillan Lecture: Journeys beyond the horizon. Phys Ther. 2001;81:1817–1829 References Shore, S., & Griggs, G. K. (2010). Health Care Reform. NC Med J, 71(5). Sood, N., Huckfeldt, P. J., Escarce, J. J., Grabowski, D. C., & Newhouse, J. P. (2011). Medicare’s bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Affairs, 30(9), 1708-1717. Thurber RM, Terry Tate, Office Linebacker [TV]. Canton, MA: Reebok; 2002