Sodium Bicarbonate - use in critical care
advertisement

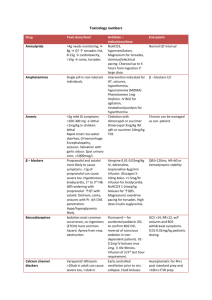
Matt Van Zetten ICU SRMO Metabolic Acidosis Hyperkalaemia Toxicology Cardiac arrest RTA CRRT Others? NaHCO3 Available in 8.4% solution, 10/50/100 ml 1mmol per ml Sodibic capsule 840mg = 10mmol Alkalinising agent / buffer Na+ and HCO3- dissociate HCO3- + H+ -> H2CO3 -> H20 + CO2 Adverse effects: Cardiovascular Myocardial dysfunction / decreased cardiac output Arrhythmias Decreased TPR / hypotension Decreased sensitivity to catecholamines Pulmonary vasoconstriction Neurological Decreased LoC Metabolic Insulin resistance Inhibition of glycolysis Treatment Correction of underlying disorder i.e. hypoxia / sepsis / hypoperfusion / DKA Mixed opinion in literature regarding buffer therapy No evidence that routine buffer use improves outcome Studies have shown no improvement in myocardial contractility with NaHCO3 administration Alternative buffers researched, but not in clinical practice Buffer therapy generally reserved for severe MA Threshold of “severe” MA varies Based on Base Excess (to correct 50% of deficit) <5kg BE x weight/4 Child BE x weight/6 Adult BE x weight/10 Toxicology / Arrest 1-2 mmol/kg/dose Increased CO2 load Worsening of intracellular acidosis Hypokalaemia Hypernatraemia Hypervolaemia Hypocalcaemia (decreased ionised Ca) Metabolic alkalosis Worsening of lactic acidosis Decreased O2 delivery to tissues Decreased acidosis inhibition of anaerobic metabolism Only advised if life threatening and associated with metabolic acidosis Facilitates intracellular shift of K in exchange for extracellular movement of H Temporising measure similar to salbutamol / Insulin I.E. K >7 with ECG changes + acidosis Toxic effects via: Blockade of fast cardiac Na channels Noradrenaline reuptake inhibition alpha blockade Anticholinergic action Clinically Tachycardia, QRS / QT / PR prolongation, hypotension Confusion, drowsiness/coma, fever Acidosis (mixed) Hypokalaemia NaHCO3 MOA: Alkalinisation increases TCA protein binding ?Correction of acidosis -> improved myocardial function ?via increasing extracellular sodium Volume loading Therapeutic goal Resolution of hypotension, QRS prolongation 1-2mmol/kg boluses Target pH 7.5-7.55 NB: Hyperventilation and HTS have also been shown to be effective in reducing QRS prolongation Propanolol overdose Chloroquine Overdose Class 1a / 1c antiarrhythmics overdose Venlafaxin overdose Bupropion overdose Therapeutic goals 1-2mmol/kg every 2-3 minutes Until hypotension and QRS complexes resolve Toxic effects via: Direct stimulation of respiratory centre Increased endogenous acid production Acidity of salicylate itself Uncoupling oxidative phosphorylation Inhibiting Krebs cycle enzymes Inhibiting amino acid synthesis. Clinically: Raised anion gap acidosis Hyperventilation Hyperthermia Hypotension Neurological – Tinnitus / Deafness / N+V / Confusion / Seizures NaHCO3 MOA: Enhances urinary drug elimination Increases elimination from tissue and serum Prevents redistribution to CNS Treatment Goal Serum pH <7.5 Urinary pH >7.5 Toxic effects via Toxic metabolites (first enzyme is ADH) (glycoaldehyde, glycolic acid, glyoxylate, oxalic acid) Deposition of calcium oxalate in tissues (e.g. kidneys) Clinically Apparent drunkenness N+V Seizures Coma Raised anion/osmolar gap metabolic acidosis Hyperosmolality ATN / Renal Failure NaHCO3 MOA: Correct acidosis Increase elimination of glycolic acid by kidneys Inhibit precipitation of calcium oxalate crystals Therapeutic Goal: Metabolic acidosis with an arterial pH < 7.3 should be treated with a sodium bicarbonate infusion to keep the pH between 7.35 and 7.45 Aim for urinary pH >7.0 Toxic effects via: Metabolism in liver via ADH to formaldehyde -> formic acid Clinically: Drunkenness Headache / nausea / vomiting Blindness (optic nerve damage) Drowsiness / coma Seizures Raised anion/osmolar gap acidosis NaHCO3 MOA: Correcting metabolic acidosis Decreasing formic acid level Therapeutic Goal Metabolic acidosis with an arterial pH < 7.3 should be treated with a sodium bicarbonate infusion to keep the pH between 7.35 and 7.45 Routine use of sodium bicarbonate is not recommended for cardiac arrest by the ARC Studies have shown no improvement in outcome ?Related to worsened intracellular acidosis Consider administration in: TCA overdose Hyperkalaemia Pre-existing metabolic acidosis Prolonged cardiac arrest ARC guidelines recommend NaHCO3 as 2nd line therapy for several conditions PEA As acidosis /hypovolaemia may predispose to PEA Asystole / Severe Bradycardia Refractory VF/VT Distal RTA Reduced H+ secretion in DCT Na / K wasting Hyperchloraemic MA Typically require 1-4 mmol/kg/day of Sodibic Proximal RTA Impaired HCO3 reabsorption in PCT K wasting May require up to 10mmol/kg/day NaHCO3 used as buffer in dialysate fluid CRRT rather than NaHCO3 can be used to treat severe metabolic acidosis Also useful to dialyse toxins Preventing contrast induced nephropathy Mixed outcomes from research in recent years Some trials show decreased AKI with NaHCO3 pre- hydration Meta-analysis (Eur J Radiology 2009) Many included trials not of high quality OR for CIN 0.33 with NaHCO3 vs. NaCl No difference in death / CCF / RRT requirement Not routinely recommended Further research ongoing