Improving Drug Utilization Review Controls in
advertisement

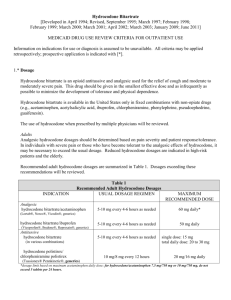
Improving Drug Utilization Review Controls in Part D Brian Martin, Pharm.D. Deputy Director, Division of Formulary and Benefit Operations 1 Improving Drug Utilization Review Controls in Part D • Part D sponsors are, and have been, responsible for establishing reasonable and appropriate drug utilization management programs that assist in preventing overutilization of prescribed medications • CMS has determined that sponsors need to employ more effective concurrent and retrospective drug utilization review (DUR) programs to address overutilization of medications in order to protect beneficiaries, to comply with drug utilization management (DUM) requirements, and to reduce fraud, waste and abuse in the Part D program 2 2013 Requirements (Call Letter) • Level One: Improved Use of Concurrent Claim Edits (Safety Controls at POS) • Level Two: Improved Use of Formulary Utilization Management Designs (QLs at POS) • Level Three: Improved Retrospective DUR Programming and Case Management • Data Sharing Between Sponsors 3 Level One: Improved Use of Concurrent Claim Edits (Safety Controls at POS) • As long as they are consistent with FDA labeling, the safety edits at this level can be implemented without submission to or approval by CMS • Applies to all drugs (including the six protected classes and controlled substances) • Edits include: early refill edits, therapeutic duplication edits and dose limitations at or above the maximum dose • Level One controls should be applied to all medications 4 Level Two: Improved Use of Formulary Utilization Management Designs (QLs at POS) • QLs/At or Above FDA Maximum Dose (No HPMS Submission) • Part D sponsors are permitted to apply QLs at or above the FDA maximum approved dosing to covered Part D drugs, including drugs within a protected class, in order to promote safe use (by not allowing dosages beyond maximum dose or unsafe dosages) and to decrease fraud, waste and abuse • QLs/No FDA Maximum Dose (HPMS Submission) • Part D sponsors may also apply QLs to drugs, as appropriate, for which there is no clearly defined maximum dose in the approved labeling, such as most opioid analgesics, to ensure safety, promote cost-effectiveness through dose optimization, and to decrease fraud, waste and abuse • QLs/Below FDA Maximum Dose (HPMS Submission) • Part D sponsors may submit QLs, as appropriate, below the FDA maximum approved dosing to promote cost-effectiveness through dose optimization, and to decrease fraud, waste and abuse, if the approved maximum dose is accessible on the plan formulary 5 Level Two Cont’d. • HPMS Formulary Submission Requirements: • QLs for drugs that have no FDA-labeled maximum dose • QLs for drugs below the FDA-labeled maximum dose • Dose-optimization edits • QLs/edits that prevent the dispensing of drugs above the FDA-labeled maximum dose are not required to be submitted on the HPMS formulary 6 Level Three: Improved Retrospective DUR Programming and Case Management • For 2013, Level Three controls apply to opioids • Sponsors should have DUR programming (that is, retrospective report-generation criteria) that identifies patterns which suggest that the identified patients may be at risk of overutilization, so that these cases may be further analyzed clinically for possible overutilization • Part D sponsors should create and monitor Part D utilization reports to identify patterns of apparent duplicative drug use over sustained periods of time and/or across multiple drug products • We expect sponsors to implement programs in a manner that eliminates the need to review borderline cases 7 Level Three Cont’d. • When warranted by review of the retrospective DUR programmed reports and the beneficiaries’ medication histories, clinical staff should communicate with prescribers and beneficiaries to ascertain medical necessity • This clinician-to-clinician communication should include information about the existence of multiple prescribers and the beneficiary’s total opioid utilization, as well as elicit any complicating factors • Results of case management may confirm that the current level of opioids is medically necessary, or in some cases, that a lower level or no opioids, are warranted 8 Level Three Cont’d. • To the extent that a Part D sponsor has identified a bona fide safety concern, the sponsor may move forward with an overutilization protocol; provided, the sponsor has made reasonable efforts to contact the prescriber and beneficiary • If medical necessity cannot be established, sponsors may implement beneficiary-level edits at POS at all network pharmacies that will result in the rejection of claims, or rejection of quantities in excess of plan established limits for the beneficiary • While the end result of a case management approach may be that prescriptions from certain prescribers who do not communicate with the sponsor may be denied, this is not the same thing as the sponsor restricting (or “locking-in”) the beneficiary to certain providers in advance 9 Data Sharing Between Sponsors • HIPAA permits such data sharing between sponsors • Sponsors can share the record and actions generated by overutilization review, e.g., the record from the retrospective DUR review/case management, as well as beneficiaryspecific POS edits, with the successor sponsor • CMS will develop a process for sponsors to share data 10 Reporting Suspected Fraudulent Activity • Sponsors are reminded that if a sponsor believes a beneficiary, prescriber, and/or pharmacy is involved in fraudulent activity, they should make referrals to the appropriate agencies in accordance with the policy set forth in Chapter 9 of the Medicare Prescription Drug Benefit Manual • The MEDIC may be reached at the following number 1-8777SAFERX (1-877-772-3379) 11 CMS Overutilization Analysis • Conducted an analysis of methods utilized by a sample of Part D sponsors to detect and manage overutilization of opioid analgesics • Identified 20 high-utilizing outlier beneficiaries of opioids per plan based on: • • • • • Total claims Total days supply Average daily dose Number of prescribers Number of pharmacies • Cancer patients were excluded based on specific RxHCC categories • Requested responses from each plan about their utilization management process for each of the outlier beneficiaries 12 CMS Overutilization Analysis • • • Did you previously identify this beneficiary as having a potential pain medication overutilization problem? Had you reviewed this beneficiary’s pain prescription records prior to receiving this inquiry from CMS? Based on your review (now or previously) of the claims information: • • • • Do you have concurrent drug utilization review edits (e.g. maximum dose, early refill, therapeutic duplication) in place to control overutilization of the identified drugs? • • Did you find at least one medically acceptable indication for the beneficiary’s high utilization of pain medication(s)? What was the diagnosis (ICD-9 or condition)? If an acceptable diagnosis was not identified, what was the justification for the high utilization of pain medication(s)? Was a concurrent drug utilization review edit to control overutilization of pain medications exceeded for any of the beneficiary’s pain medications? Did you contact anyone or utilize any type of intervention in relation to this beneficiary’s utilization of pain medications? 13 CMS Overutilization Analysis • 24% of beneficiaries were not previously identified by the sponsor as potentially over utilizing opioid analgesics • Of the beneficiaries identified, 45% would not have experienced a POS edit as a result of their utilization • A medically accepted indication for the identified utilization of the opioid analgesic was not identified for 34% of beneficiaries 14 Case Studies from Overutilization Analysis 15 Case 1. Medications. • Oxycodone/APAP 10/325 mg #180 per 30 days filled once monthly • Hydrocodone/APAP 10/325 mg #360 per 30 days filled once monthly • Hydrocodone/APAP 7.5/750 mg #60 per 10 days filled once monthly • Several chronic meds filled regularly 16 Case 1. Prescribers. • Oxycodone/APAP 10/325 mg – Routinely prescribed by psychiatrist who also prescribes beneficiary’s chronic mental health drugs • Hydrocodone/APAP 10/325 mg – Routinely prescribed by same psychiatrist • Hydrocodone/APAP 7.5/750 mg – Routinely prescribed by internist who prescribes beneficiary’s chronic meds • Occasional prescriptions for opioid analgesics from other providers 17 Case 1. Pharmacies and Fill Dates. • Oxycodone/APAP 10/325 mg – Only fills this drug at independent pharmacy A • Hydrocodone/APAP 10/325 mg – Fills on the same day as Oxy/APAP each month, along with chronic meds, at independent pharmacy B • Hydrocodone/APAP 7.5/750 mg – Fills between chain A and chain B, along with rare fills for chronic meds 18 Case 1. Discussion 19 Case 2. Medications. • Multiple fills for various strengths of Oxycodone/APAP, Hydrocodone/APAP, Codeine/APAP • October 2010: • • • • • • • Codeine/APAP 60/300 mg #100 per 8 days Oxycodone 10/325 mg #180 per 30 days Hydrocodone/APAP 7.5/750 mg #100 per 20 days Hydrocodone/APAP 10/650 mg #120 per 20 days Hydrocodone/APAP 5/500 mg # 60 per 30 days Hydrocodone/APAP 10/500 mg #120 per 30 days Codeine/APAP 30/300 mg #100 per 8 days 20 Case 2. Prescribers. • A surgeon prescribed: • Codeine/APAP 300/60 mg #100 per 8 days • Hydrocodone/APAP 7.5/750 mg #100 per 20 days • Codeine/APAP 300/30 mg #100 per 8 days • Remainder prescribed by three different internists and an ER physician 21 Case 2. Pharmacies. • The following were filled at the same chain pharmacy: • • • • Codeine/APAP 300/60 mg #100 per 8 days Oxycodone 10/325 mg #180 per 30 days Hydrocodone/APAP 7.5/750 mg #100 per 20 days Codeine/APAP 300/30 mg #100 per 8 days • The following were each filled at different chain pharmacies: • Hydrocodone/APAP 10/650 mg #120 per 20 days • Hydrocodone/APAP 5/500 mg # 60 per 30 days • Hydrocodone/APAP 10/500 mg #120 per 30 days 22 Case 2. Discussion 23 Next Steps for CMS • Collect implementation comments: • Submit comments to PartDformularies@cms.hhs.gov by April 30, 2012 • “Improving DUR Controls” in subject line • Continue to monitor outlier sponsors: • Excessive acetaminophen doses; • Continued, high utilization of opioid analgesics • Develop model notices for prescribers and beneficiaries • Initiate educational campaigns for prescribers, pharmacies, and beneficiaries with respect to overutilization control efforts 24 CMS Oversight • Oversight of Level Three Controls • CMS will be reviewing case files for any complaints relating to the implementation of controls: • Evidence of overly restrictive controls • Outreach methods and attempts • Provider communication • Analyses to look behind Part D sponsors to ensure effective identification of potential overutilizers 25 Summary • Part D sponsors should optimize their use of Level One and Level Two drug utilization review controls • The implementation of beneficiary-level edits at POS, when warranted, is not the same as pharmacy/prescriber lock-in as it currently exists outside of Part D • Part D sponsors are responsible for identifying beneficiaries for Level Three controls, but CMS will monitor the effectiveness of sponsors’ efforts • Improving drug utilization review controls is not a substitute for referrals to MEDIC, local law enforcement, etc • CMS will provide additional guidance, model documents, and educational materials 26