Assessing Control Adjusting Therapy in Youths > 12 Years of Age Adults
advertisement
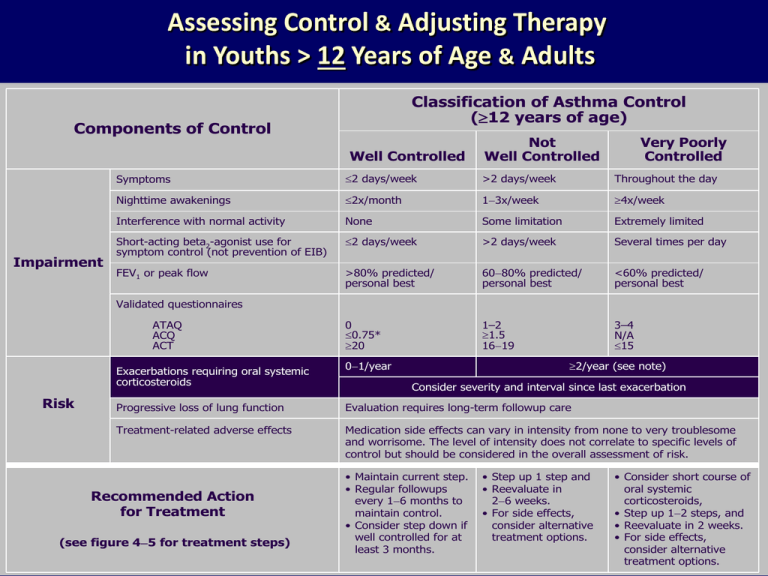
Assessing Control & Adjusting Therapy in Youths > 12 Years of Age & Adults Classification of Asthma Control (12 years of age) Components of Control Well Controlled Impairment Not Well Controlled Very Poorly Controlled Symptoms 2 days/week >2 days/week Throughout the day Nighttime awakenings 2x/month 13x/week 4x/week Interference with normal activity None Some limitation Extremely limited Short-acting beta2-agonist use for symptom control (not prevention of EIB) 2 days/week >2 days/week Several times per day FEV1 or peak flow >80% predicted/ personal best 6080% predicted/ personal best <60% predicted/ personal best 0 0.75* 20 1–2 1.5 1619 3–4 N/A 15 Validated questionnaires ATAQ ACQ ACT Exacerbations requiring oral systemic corticosteroids Risk 2/year (see note) 01/year Consider severity and interval since last exacerbation Progressive loss of lung function Evaluation requires long-term followup care Treatment-related adverse effects Medication side effects can vary in intensity from none to very troublesome and worrisome. The level of intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk. Recommended Action for Treatment (see figure 45 for treatment steps) • Maintain current step. • Regular followups every 16 months to maintain control. • Consider step down if well controlled for at least 3 months. • Step up 1 step and • Reevaluate in 26 weeks. • For side effects, consider alternative treatment options. • Consider short course of oral systemic corticosteroids, • Step up 12 steps, and • Reevaluate in 2 weeks. • For side effects, consider alternative treatment options. Stepwise Approach for Managing Asthma in Youths >12 Years of Age & Adults Intermittent Asthma Persistent Asthma: Daily Medication Consult asthma specialist if step 4 care or higher is required. Consider consultation at step 3 Step 6 Step 5 Step 4 Step 3 Preferred: Low dose ICS Low-dose ICS + LABA OR – Medium dose ICS Alternative: Cromolyn, LTRA, Nedocromil or Theophylline Alternative: Low-dose ICS + either LTRA, Theophylline, or Zileuton Step 2 Preferred: Step 1 Preferred: SABA PRN Preferred: Medium Dose ICS + LABA Alternative: Medium-dose ICS + either LTRA, Theophylline, or Zileuton Preferred High Dose ICS + LABA AND Consider Omalizumab for patients who have allergies Preferred High dose ICS + LABA + oral corticosteroid AND Consider Omalizumab for patients who have allergies Each Step: Patient Education and Environmental Control and management of comorbidities Steps 2 – 4: Consider subcutaneous allergen immunotherapy for patients who have allergic asthma Step up if needed (first check adherence, environmental control & comorbid conditions) Assess control Step down if possible (and asthma is well controlled at least 3 months) •Quick-relief medication for ALL patients -SABA as needed for symptoms: up to 3 tx @ 20 minute intervals prn. Short course of o systemic corticosteroids may be needed. • Use of SABA >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate control & the need to step up treatment. Section 5 Managing Exacerbations of Asthma 3 Key Points – Managing Exacerbations Early treatment of asthma exacerbations is the best strategy for management: Patient education includes a written asthma action plan (AAP) to guide patient self-management of exacerbations – especially for patients who have moderate or severe persistent asthma and any patient who has a history of severe exacerbations A peak-flow-based plan for patients who have difficulty perceiving airflow obstruction and worsening asthma is recommended EPR -3 Pg. 373 4 Key Points – cont. – Recognition of early signs of worsening asthma & taking prompt action – Appropriate intensification of therapy, often including a short course of oral corticosteroids – Removal or avoidance of the environmental factors contributing to the exacerbation – Prompt communication between patient and clinician about any serious deterioration in symptoms or peak flow, decreased responsiveness to SABAs, or decreased duration of effect 5 Exacerbations Defined - RISK Are acute or subacute episodes of progressively worsening shortness of breath, cough, wheezing, and chest tightness? — or some combination of these symptoms Are characterized by decreases in expiratory airflow that can be documented and quantified by spirometry or peak expiratory flow – These objective measures more reliably indicate the severity of an exacerbation than does the severity of symptoms 6 Classifying Severity of Asthma Exacerbations in the UC or ER Setting Severity Mild Symptoms & Signs Dyspnea only with activity (assess tachypnea in young children) Initial PEF (or FEV1) PEF 70 percent predicted or personal best Usually cared for at home Prompt relief with inhaled SABA Possible short course of oral systemic corticosteroids PEF 4069 percent predicted or personal best Usually requires office or ED visit Relief from freq. inhaled SABA Oral systemic corticosteroids; some symptoms last 1–2 days after treatment is begun PEF <40 percent predicted or personal best Usually requires ED visit and likely hospitalization Partial relief from frequent inhaled SABA PO systemic corticosteroids; some symptoms last >3 days after treatment is begun Adjunctive therapies are helpful Moderate Severe Dyspnea interferes with or limits usual activity Dyspnea at rest; interferes with conversation Clinical Course Subset: Life threatening Too dyspneic to speak; perspiring PEF <25 percent predicted or personal best Requires ED/hospitalization; possible ICU Minimal or no relief w/ frequent inhaled SABA Intravenous corticosteroids Adjunctive therapies are helpful Managing Asthma Exacerbations at Home Assess Severity Patients at high risk for a fatal attack (see figure 5–2a) require immediate medical attention after initial treatment. Symptoms and signs suggestive of a more serious exacerbation such as marked breathlessness, inability to speak more than short phrases, use of accessory muscles, or drowsiness (see figure 5–3) should result in initial treatment while immediately consulting with a clinician. Less severe signs and symptoms can be treated initially with assessment of response to therapy and further steps as listed below. If available, measure PEF—values of 50–79% predicted or personal best indicate the need for quick-relief mediation. Depending on the response to treatment, contact with a clinician may also be indicated. Values below 50% indicate the need for immediate medical care. Initial Treatment Inhaled SABA: up to two treatments 20 minutes apart of 2–6 puffs by metered-dose inhaler (MDI) or nebulizer treatments. Note: Medication delivery is highly variable. Children and individuals who have exacerbations of lesser severity may need fewer puffs than suggested above. Good Response Incomplete Response Poor Response No wheezing or dyspnea (assess tachypnea in young children). Persistent wheezing and dyspnea (tachypnea). Marked wheezing and dyspnea. PEF 80% predicted or personal best. Contact clinician for followup instructions and further management. May continue inhaled SABA every 3–4 hours for 24–48 hours. Consider short course of oral systemic corticosteroids. PEF 50–79% predicted or personal best. Add oral systemic corticosteroid. Continue inhaled SABA. Contact clinician urgently (this day) for further instruction. PEF <50% predicted or personal best. Add oral systemic corticosteroid. Repeat inhaled SABA immediately. If distress is severe and nonresponsive to initial treatment: —Call your doctor AND —PROCEED TO ED; —Consider calling 9–1–1 (ambulance transport). To ED. What the EPR -3 Does NOT Recommend – Drinking large volumes of liquids or breathing warm, moist air (e.g., the mist from a hot shower) – Using over-the-counter products such as antihistamines or cold remedies – Although pursed-lip and other forms of controlled breathing may help to maintain calm during respiratory distress, these methods do not bring about improvement in lung function 9