Treatment of Hot Flashes - Indiana Pharmacists Alliance
advertisement
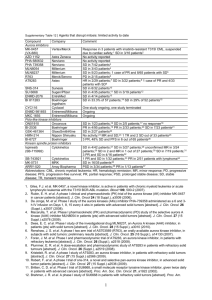
Turn down the heat! Treating hot flashes Amanda Place, PharmD, BCACP St Vincent Joshua Max Simon Primary Care Center September 2014 I HAVE NO ACTUAL OR POTENTIAL CONFLICT OF INTEREST IN RELATION TO THIS PROGRAM OR PRESENTATION. Objectives Describe both symptoms and possible mechanisms of hot flashes Discuss benefits and risks of estrogencontaining products in the treatment of hot flashes Identify the utility of and evidence supporting non-estrogen treatment alternatives Define the role of complementary and alternative medicine therapies in the treatment of hot flashes What is a hot flash? Sudden sensation of heat (face, neck and chest) Skin flushing, sweating May be accompanied by anxiety, irritation Often followed by chills J Support Oncol 2006;4:315-320 Ann N Y Acad Sci 1990;592:52-86 Prevalence 70-80% of women will experience hot flashes Average duration: 2-5 years 15-20% of women may have ongoing hot flashes Greater severity in patients with chemical or surgical menopause, or premature menopause (<40 yrs of age) Am J Epidemiol 2000; 152:463 Am J Public Health 2006; 96: 1226 Arch Intern Med. 2008;168(8):840-846 Pathophysiology Exact mechanism for vasomotor flushing not yet identified Several proposed mechanisms ◦ Decrease in hormones ◦ Changes in the hypothalamus ◦ Other factors implicated Prostaglandins Endorphins Neurotransmitters Acta Oncologica 2002;41:269-75 Ann Pharmacother1997;31:915-7 ONF 2002;29: 33-40 Ann Pharmacother2002;36:433-6 Contributing Factors Modifiable ◦ ◦ ◦ ◦ ◦ BMI Smoking Avoidance of triggers Exercise Depression/anxiety Difficult to modify ◦ Cause of menopause ◦ Genetics ◦ Socioeconomic factors Am J Epidemiol 2000; 152:463 Am J Public Health 2006; 96: 1226 Assessment Tools Patient history and recall Hot flash diary Validated tools: ◦ ◦ ◦ ◦ Hot Flash Score Greene Climacteric Score Modified Kupperman Index Utian Quality of Life Scale Menopause 2002; 9(6):402-410 J Clin Oncol 2001; 19:4280-4290 Maturitas 2012 March;71(3):213-216 Treatment Options Lifestyle modifications Hormonal Therapies SSRI/SNRI Gabapentin Clonidine CAM modalities Endocr Pract 2011;17 (suppl 6) Menopause 2012;19(3):257-271 Climacteric 2014;17:1-16 Lifestyle Modification Decrease BMI Decrease caffeine Modify or eliminate alcohol use Increase exercise Improve dietary habits Layered clothing Stress reduction/paced respirations Menopause 2004;11:11 Menopause 2012;20(2):179-184 Menopause 2012;19(7):749-759 Estrogen Replacement (ET) Considered most effective agent Agent Initial dose Conjugated 0.3 mg equine estrogens (CEE) 17βEstradiol 0.5 mg Transdermal 0.025 mg estradiol Estradiol gel 0.5 mg High dose 1.25 mg 2 mg 0.1 mg 1.5 mg Endocr Pract 2011;17(Suppl 6) Menopause 2012;19(3):257-271 Climacteric 2014;17:1-16 ET Risks and Benefits Benefits Risks Vasomotor symptoms Vaginal symptoms Sexual function Coronary heart disease Stroke Venous thromboembolism Urinary tract health Osteoporosis Quality of life Endometrial cancer Breast cancer Effect of ET on ovarian cancer, lung cancer, mood, dementia, and mortality remain mixed. Endocr Pract 2011;17(Suppl 6) Menopause 2012;19(3):257-271 Climacteric 2014;17:1-16 ET Considerations Transdermal = risk Duration of use Appropriate dose Need for progestin Choice of progestin Taper vs. stop Bioidentical ET Menopause 2010;17:946-954 Menopause 2006;13:370-376 Endocr Pract 2011;17(Suppl 6) Menopause 2012;19(3):257-271 Assessment question According to data from the Women’s Health Initiative, which of the following is a benefit of using estrogen to treat hot flashes? 1. Increase or maintenance of bone mass 2. Decrease in cardiovascular risk because of increase in good cholesterol 3. Decrease in the risk of endometrial cancer 4. All of the above Assessment question A 50 yo female would like to start estrogen therapy for hot flashes. She has no allergies and no significant medical or surgical history. Which would be a good initial choice for her? 1. 2. 3. 4. Estradiol 0.025 mg/24 hr transdermal patch once weekly Estradiol 0.5 mg /norethindrone acetate 0.1 mg daily CEE 0.625 mg/medroxyprogesterone 2.5 mg daily Estradiol cream 0.1 mg/gm: 2 gm intravaginally once daily at bedtime Bazedoxifene/CEE (Duavee) Tissue-selective estrogen complex Indications Precautions/ warnings Dose Cost Vasomotor symptoms, prevention of postmenopausal osteoporosis Refer to CE CEE 0.45 mg and bazedoxifene 20 mg ≈$140 per month Safety data for up to 2 years Lexi-Comp, Inc. (Lexi-DrugsTM ). Lexi-Comp, Inc.; Version1.13.0 Accessed July 28th, 2014 Menopause 2009;16(6):1116-1124 Menopause 2012;19(4):479-485 Clinical study limitations Small sample sizes Outcomes based on patient-reported data Many studies focus on patients with breast cancer history Large placebo effect: 20-30% reductions in hot flash score/frequency Limited duration of trials Non-estrogen therapies Menopause 2008;15:655 Progestational agents Megestrol acetate • 20-80 mg daily Medroxyprogesterone acetate • 400 mg depot Norethindrone acetate • 10 mg daily N Engl J Med 1994;331(6);347 J Clin Oncol 2008;26(10):1650 J Clin Oncol 2006;24(9):1409 Ann Oncol 2002;13(6):883 Progestational agents Weight gain Adrenal suppression Bone loss Clotting risk Breast cancer risk SSRIs/SNRIs Mechanism: increases available neurotransmitters Doses differ if only treating hot flashes Serotonin syndrome risks Product selection: ◦ ◦ ◦ ◦ Drug interactions Cost Evidence Co-morbid conditions Paroxetine ® (Brisdelle ) Approved 2013 Trial #1 at 4 wks VMS frequency vs placebo ↓ 1.2 /day Trial #2 at 4 wks Trial #1 at 12 wks Trial #2 at 12 wks ↓ 1.3/day ↓ 0.9/day ↓ 1.7/day Cost ~$150/month Brisdelle PI, Noven Therapeutics, LLC, Miami, FL Other antidepressants Drug Daily Dose Outcomes Fluoxetine 20 mg ↓ monthly hot flash score Sertraline 50-100 mg ↓ weekly frequency Citalopram** 20-40 mg ↓ hot flash scores Escitalopram 10-20 mg ↓ daily frequency Venlafaxine 37.5-75 mg ER ↓ hot flash scores Desvenlafaxine 100 mg ↓ daily frequency Duloxetine 60 mg ↓ VMS ** showed efficacy as an add-on to HRT as well References provided at end of presentation Antidepressant safety T/F May inhibit platelet aggregation T/F May be associated with bone loss/fracture risk T/F Don’t need to be tapered when used for hot flashes T/F May decrease the efficacy of antibiotics T/F May decrease the efficacy of tamoxifen T/F May increase risk of suicidality Antidepressant pearls Which one must have a wash-out? fluoxetine Which ones should be cross-tapered? paroxetine or venlafaxine Which one to choose if a patient takes clopidogrel? citalopram or venlafaxine Which one causes the MOST hypertension? venlafaxine The gabas Mechanism: GABA vs. Norepinephrine Lower doses than used in neuropathic pain Drug interactions: CNS depressants Monitoring: renal function Adverse effects: drowsiness, dizziness, rash, peripheral edema, weight gain Gabapentin dose range J Clin Oncol 2009; 27:2831-2837 Gabapentin ER interrupted FDA declined approval in May 2013 Trial VMS change VMS change @ @ 4 weeks 12 weeks Breeze 1: 1200 mg ↓ 0.96/day ↓ 0.56/day** Breeze 1: 1800 mg ↓ 1.51/day ↓ 1.53/day Breeze 2: 1200 mg ↓ 1.61/day ↓ 1.56/day Breeze 2: 1800 mg ↓ 1.51/day ↓ 1.12/day Breeze 3: 1800 mg ↓ 1.69/day ↓ 1.14/day ** not statistically significant www.clinicaltrials.gov accessed 2/13/14 Pregabalin Not seeking FDA approval Daily dose 75 mg BID 150 mg BID Change in hot flash frequency ↓ 1.7/day ↓ 2.0/day Cost: pregabalin = gabapentin x 10 J Clin Oncol 28:641-647 Gabas’ safety T/F These should not be used in pts with NYHA class 3 HF T/F These drugs should be dose adjusted for hepatic function T/F Since these agents are hepatically metabolized, they have many drug interactions T/F Dizziness/somnolence may go away over time Gabas’ pearls Possible to direct switch Gabapentin 0-900 mg per day 901-1500 mg per day Pregabalin 150 mg per day 225 mg per day 1501-2100 mg per day 300 mg per day Gabapentin dosing regimen may differ from pain dosing: ◦ 600-900 mg hs vs. 300 mg TID Pain Med. 2010; 11(3): 456-465 Clonidine Mechanism: decreases available neurotransmitters Dose range: 0.1 to 0.2 mg per day- oral or transdermal Drug interactions: antihypertensives, SNRIs Adverse effects: drowsiness, dizziness, fatigue, dry mouth, orthostatic hypotension, dermatologic reactions with transdermal form Obst Gynecol 1982;60:583-586 J Clin Oncol 1994;12:1155-158 Comparator Trials (Gabapentin = estrogen) >placebo Venlafaxine preferred vs gabapentin Gabapentin = gabapentin + SSRI/SNRI MPA = megestrol Fluoxetine = citalopram = placebo MPA > venlafaxine Venlafaxine > clonidine (Estradiol ≈ venlafaxine) > placebo JAMA Intern Med 2014;174(7):1058-1066 J Clin Oncol 2010;28:147-5152 Ann Oncol 2002;13:883-888 J Clin Oncol 2006:24:1409 Obstet Gynecol 2006;108:41-48 J Clin Oncol 2007;25:308-312 Menopause 2005;12(1):18-26 Ann Oncol 2007;18:689-693 Assessment question Which of the following drug classes have NOT shown efficacy in the treatment of hot flashes: 1. Estrogens 2. Dihydropyridine calcium channel blockers 3. α-2-δ ligands 4. Serotonin/norepinephrine reuptake inhibitors Assessment question A 47 yo female with a strong family of breast cancer would like to start drug treatment for hot flashes. She takes tamoxifen 20 mg and a multivitamin daily. Blood pressure at most recent visit was 114/74 mm Hg. What would you recommend? 1. 2. 3. 4. Paroxetine 7.5 mg daily Estradiol 0.5 mg/norethindrone acetate 0.1 mg daily Clonidine 0.1 mg/24 hr transdermal patch weekly Gabapentin 300 mg in the morning and 600 mg before bedtime CAM Hormonal agents Alfalfa Black Cohosh Chasteberry DHEA Dong Quai Flaxseed Hops Kudzu Licorice Panax Ginseng Red clover Soy Wild Yam CAM Hormonal agents Alfalfa Black Cohosh Chasteberry DHEA Dong Quai Flaxseed Hops Kudzu Licorice Panax Ginseng Red clover Soy Wild Yam CAM Treatments for Hot Flashes Likely safe Possibly safe Flaxseed Soy foods Black Cohosh Soy extracts Insufficient evidence Chasteberry Ginkgo Vitamin E Alfalfa DHEA (short term) Hops Kudzu Licorice Valerian Possibly ineffective Evening Primrose oil Dong Quai (short term) Red Clover Wild Yam Panax Ginseng Effective Likely effective Possibly effective Adapted from Natural Medicines ComprehensiveDatabase-Accessed 5/17/2010 CAM Hormonal agents General cautions: ◦ ◦ ◦ ◦ Unknown or questionable estrogenic activity Standardization of products/preparations Consistent quality of products Lack of high quality evidence Acupuncture Difficult to determine a true “placebo” group Differing disciplines of acupuncture Pt expectations Lack of understanding about physiologic effects of acupuncture Menopause 2010;17(2):228-230 Menopause 2009;16:1065-1073 Conclusions Choice of agent should be made with patient-specific variables as a guide. Patient expectations may impact efficacy. Different agents or combinations may need to be tried to achieve desired benefit. Turn down the heat! Treating hot flashes Amanda Place, PharmD, BCACP St Vincent Joshua Max Simon Primary Care Center September 2014 Slide 17 References Obst Gynecol 1982;60:583-586 J Clin Oncol 1994;12:155-158 J Clin Oncol 2002;20:1578-1583 Lancet 2000;356:2059-2063 J Clin Oncol 2010;28:3278-3283 JAMA 2001;305(3):267-274 J Clin Oncol 2009;27:2831-2837 Drugs 2011;71(3):287-304 Pharmacotherapy 2009;29(11):1357-1374