Dr David Straton
SSRIs
Brands
Citalopram
Cipramil, Celapram, Talam, Talohexal
Escitalopram
Lexapro, Esipram
Fluoxetine
Prozac, Auscap, Fluohexal, Lovan, Zactin
Fluvoxamine
Luvox, Faverin, Movox
Paroxetine
Aropax, Oxetine, Paxtine
Sertraline
Zoloft, Concorz, Eleva, Setrona, Xydep
SNRIs
Brands
Desvenlafaxine
Pristiq
Duloxetine
Cymbalta
Venlafaxine
Efexor
Others
Bupropion (NDRI)
Zyban
Buspirone (Piperazine)
Buspar
Mianserin (Tetracyclic)
Tolvon, Lumin
Mirtazapine (NaSSA)
Avanza, Axit 30, Mirtazon, Remeron
Moclobemide (RIMA)
Aurorix, Arima, Clobemix, Maosig, Mohexal
Reboxetine (NRI)
Edronax
Tranylcypromine (MAOI) Parnate
Normal Synapse
Serotonin
Synapse in depression
SSRI increases serotonin
5HT1a
Some receptors may upregulate
SSRI effects
5HT1a Anxiety down, mood up
5HT2a Insomnia, sex problems
5HT2c Agitation
5HT3
Nausea
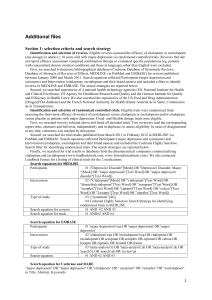
Major studies and meta-analyses 2008-9
STAR*D (Sequenced Treatment Alternatives to Relieve Depression).
26th Feb 2008, PLoS Medicine published the Hull meta-analysis of anti
depressant trials from the FDA.
18th Nov 2008, the American College of Physicians published two
background papers on anti-depressants.
28th Jan 2009, the Lancet published online a major meta-analysis of
antidepressants.
3rd Feb 2009, the Canadian Medical Association Journal published a
review of studies about whether SSRIs increase the risk of suicide.
June 2009, the Journal of Clinical Psychopharmacology published a
meta-analysis of anti-depressant related sexual dysfunction.
In August 2009, the BMJ published a meta-analysis on suicidality.
STAR*D
(Sequenced Treatment Alternatives to Relieve Depression)
The Hull meta-analysis
Attempt to avoid publication bias.
FOI on FDA, all clinical trials, both published and
unpublished.
Trials with no benefit + no data left out. (Citalopram and
sertraline).
Most trials only 6 weeks duration.
Conclusion, drug only beat placebo in most severe
depressions.
Hull
The American College of Physicians Reviews
• ‘Overall, no substantial differences in efficacy’
• Fluvoxamine lost every comparison test for efficacy
• Venlafaxine prone to nausea
• Sertraline prone to diarrhoea
• Mirtazapine prone to weight gain
•Venlafaxine and paroxetine prone to discontinuation syndrome
Fluvoxamine compared to other anti-depressants
ACP
Fluvoxamine compared to other anti-depressants
ACP
Fluvoxamine compared to other anti-depressants
I.e Fluvoxamine lost every drug-to-drug contest
ACP
Lancet meta-analysis
Odds of being most effective
1) Mirtazapine
24.4%
2) Escitalopram
23.7%
3) Venlafaxine
22.3%
4) Sertraline
20.3%
5) Citalopram
3.4%
6) Milnacipran
2.7%
7) Bupropion
2.0%
8) Duloxetine
0.9%
9) Fluvoxamine
0.7%
10) Paroxetine
0.1%
11) Fluoxetine
0.0%
12) Reboxetine
0.0%
Lancet
Odds of being most acceptable
1) Escitalopram
27.6%
2) Sertraline
21.3%
3) Bupropion
19.3%
4) Citalopram
18.7%
5) Milnacipran
7.1%
6) Mirtazapine
4.4%
7) Fluoxetine
3.4%
8) Venlafaxine
0.9%
9) Duloxetine
0.7%
10) Fluvoxamine
0.4%
11) Paroxetine
0.2%
12) Reboxetine
0.1%
Lancet
Lancet
Suicide Risk (CMAJ)
CMAJ
CMAJ
Odds of suicidality (ideation or worse) for active drug relative to placebo by age in adults
Stone, M. et al. BMJ 2009
Copyright ©2009 BMJ Publishing Group Ltd.
Suicide risk (BMJ)
Suicidality risk vs placebo (ideation or worse) in adults
Drug
n
%
Placebo
n
%
Odds ratio
Escitalopram
10
3130
0.32%
5
2604
0.19%
2.44
Citalopram
24
2661
0.90%
7
1371
0.51%
2.11
Fluvoxamine
22
2187
1.01%
13
1828
0.71%
1.25
Mirtazapine
8
1016
0.79%
6
644
0.93%
0.97
Paroxetine
50
9919
0.50%
29
6972
0.42%
0.93
Duloxetine
25
2327
1.07%
18
1460
1.23%
0.88
Venlafaxine
29
5593
0.52%
30
3904
0.77%
0.71
Fluoxetine
81
7180
1.13%
67
4814
1.39%
0.71
Sertraline
18
6363
0.28%
28
5081
0.55%
0.51
All drugs
314
50043
0.63%
197
27164
0.73%
0.83
BMJ
Sexual Side-effects
Total
Severe
Mild
Nil
Desire
Arousal
Orgasm
Sertraline
27
Citalopram
55
Citalopram
82
Clomipramine 42
Venlafaxine
25
Paroxetine
47
Venlafaxine
54
Paroxetine
18
Citalopram
20
Fluoxetine
46
Paroxetine
44
Venlafaxine
16
Paroxetine
17
Sertraline
43
Sertraline
39
Sertraline
15
Fluoxetine
16
Venlafaxine
23
Fluoxetine
31
Citalopram
14
Duloxetine
4
Fluvoxamine
6
Duloxetine
11
Fluoxetine
12
Escitalopram
3
Mirtazapine
6
Fluvoxamine
7
Mirtazapine
4
Fluvoxamine
3
Duloxetine
5
Mirtazapine
4
Escitalopram
4
Mirtazapine
2
Moclobemide
4
Moclobemide 2
Fluvoxamine
3
Placebo
1
Escitalopram
1
Placebo
1
Placebo
1
Moclobemide
0.2
Placebo
1
Escitalopram
0.7
Moclobemide
0.4
Serretti
S-(+)-citalopram (Escitalopram)
R-(-)-citalopram
50/50 mixture of both = Citalopram
Treatment algorithm: plan A
Escitalopram. 2.5mg rising to 20 mg.
Similar to Level 1 in STAR*D
2nd for efficacy in Lancet meta-analysis
1st for acceptability in Lancet meta-analysis
Mild sex side-effects
Trial should last at least 2 months.
Possible disadvantage if suicide risk high (BMJ)
Treatment algorithm: plan B
(in no particular order)
Add thyroxine, esp if T4 <14 mmol/L
Add mianserin, esp if 5HT-2 related side-effects
Change to mirtazapine 30 – 60 mg. Advantage with panic
and insomnia. (Beware weight)
Change to sertraline 50 – 100 mg. Possible advantage
with suicide risk. (Beware diarrhoea and sex problems).
Change to venlafaxine (Beware nausea, sex problems,
discontinuation symptoms, and risk of suicide in
adolescents)
Treatment algorithm: plan C
California rocket-fuel
Combination of:
Venlafaxine 75 – 300 mg
Mirtazapine 30 – 60 mg
Treatments to abandon
Fluvoxamine
Reboxetine
Augmentation with lithium for unipolar depression
Treatments to downplay
Paroxetine
Antidepressants in adolescents, especially venlafaxine
and paroxetine
Treatments in danger of being
abandoned prematurely
Tranylcypromine.
'Approximately 30% of participants in the tranylcypromine
group had less than 2 weeks of treatment, and nearly half
had less than 6 weeks of treatment‘ (STAR*D)
Papers mentioned available here:
psyberspace.com.au/depression




![[FM] - International Journal of Neuropsychopharmacology](http://s3.studylib.net/store/data/005833877_1-45d158206af02f12fa92b0dbd0c16478-300x300.png)