OMERACT 8 introducti..
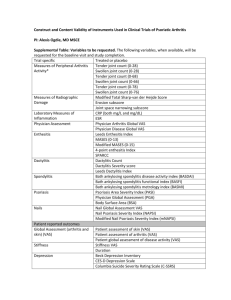
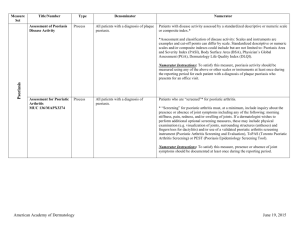
advertisement

OMERACT 8 PsA Module Co-Chairs Dafna Gladman and Philip Mease Steering Committee Alice Gottlieb, Philip Helliwell, Arthur Kavanaugh, Gerry Krueger, Peter Nash, Christopher Ritchlin, Vibeke Stand, William Taylor Psoriatic arthritis An inflammatory arthritis. Associated with psoriasis. Usually seronegative for rheumatoid factor. Associated Features: » » » » » » » Spondylitis, Enthesitis, Dactylitis, Iritis Mucous membrane ulcers Urethritis Other extra-articular features of SpA. CASPAR study Design Prospective, observational study of consecutive clinic patients with PsA and other inflammatory arthritis Target sample size of 1012 in total 30 clinics in 13 countries Gold-standard of diagnosis based on physician’s opinion Data collected 02/02 – 03/04 CASPAR Study: Methods Data collected: – Clinical and examination features – X-rays of spine, sacroiliac joints, hands and feet – Rheumatoid factor, [HLA], anti-CCP, stored blood X-rays were read centrally by 2 readers in tandem, blinded to diagnosis Clinical gold-standard validated by quality control and Latent Class Analysis (statistical modelling) New criteria developed using CART and logistic regression CASPAR Criteria Taylor W, et al. A&R 2006 (in press) Inflammatory musculoskeletal disease (joint, spine, or entheseal) With 3 or more of the following: 1. Evidence of a. Current psoriasis* psoriasis (one b. Personal history of of a, b, c) Psoriatic skin or scalp disease present today as judged by a dermatologist or rheumatologist psoriasis A history of psoriasis that may be obtained from patient, family doctor, dermatologist or rheumatologist c. Family history of psoriasis A history of psoriasis in a first or second degree relative according to patient report 2. Psoriatic nail dystrophy Typical psoriatic nail dystrophy including onycholysis, pitting and hyperkeratosis observed on current physical examination 3. A negative test for rheumatoid factor By any method except latex but preferably by ELISA or nephelometry, according to the local laboratory reference range 4. Dactylitis either a or b a. Current Dactylitis Swelling of an entire digit b. History of Dactylitis Recorded by a rheumatologist 5. Radiological evidence of juxtaarticular new bone formation Ill-defined ossification near joint margins (but excluding osteophyte formation) on plain xrays of hand or foot Specificity 98.7%, sensitivity 91.4%. *Current psoriasis scores 2, others 1. OMERACT 7 PsA Workshop Domains in PsA final vote Item Joint activity Patient Global all 3 components Pain assessment Physical function Skin disease Quality of Life Structural damage Acute Phase Reactant Axial involvement Participation Enthesitis Fatigue Dactylitis Physician Global Tissue histology MRI Morning Stiffness Damage joint count Score 99% 96% 76% 94% 91% 86% 78% 66% 64% 61% 61% 60% 48% 48% 41% 38% 34% 25% 20% OMERACT 7 PsA Workshop Research Agenda Identify optimal joint count. Develop instrument for patient global to incorporate skin and joint question. Identify optimal Skin assessment. Develop tools to define structural damage. Develop instruments for Axial assessment. Develop a tool for the assessment of participation. Develop instruments for the assessment of Enthesitis. Develop tools for the assessment Dactylitis. Imaging modalities to assess inflammation and damage. Differential tissue response to therapies. Study methods to evaluate Fatigue in PsA. Develop Composite responder indices. OMERACT 8: PsA Module Objectives Achieve consensus on the core set of domains to be assessed in PsA clinical trials and in longitudinal observational cohort studies, Review and endorse outcome measures used to assess these domains based on evidence derived from clinical trials and Set up a new research agenda to identify other assessment tools. Assessment of Psoriatic Arthritis Domains Proposed Instruments Joint assessment T/S joint count, ACR, PsARC, DAS Axial assessment Clinical measures, BASDAI, BASFI, BASRI Skin assessment PASI, Target lesion, Global Pain VAS Patient global VAS (global, skin + joints) Physician global VAS (global, skin + joints) Function/QOL HAQ, SF-36, PsAQoL Fatigue Krupp, FACIT, MFI, VAS Enthesitis assessment Mander, MASES, present/absent Dactylitis assessment Helliwell, present/absent, acute/chronic Acute phase reactant ESR, CRP, others Imaging Xray, MRI, ultrasound OMERACT 8: PsA Module Plenary Session Time Title Speaker 08:00-08:05 Introduction D. Gladman 08:05-08:15 Peripheral joints/ clinical trials P. Mease 08:15-08:25 Spinal assessment - INSPIRE D. Gladman 08:25-08:35 Dactylitis P. Healy 08:35-08:45 Enthesitis P. Helliewell 08:45-08:50 Participation W. Taylor 08:50-08:55 QoL D. Veale 08:55-09:00 Patient/physician GA A. Cauli 09:00-09:10 Skin assessment G. Krueger 09:10-09:20 Radiology D. Van der Heijde 09:20-09:30 Immunohistology O. Fitzgerald 09:30-09:35 Patient perspective TBA