Respiratory Physiology
advertisement
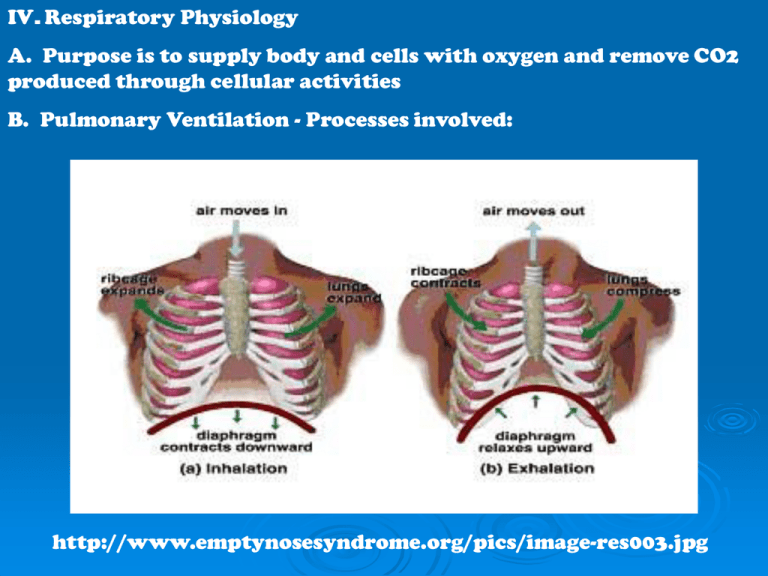
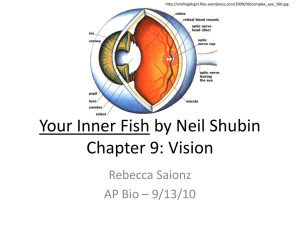
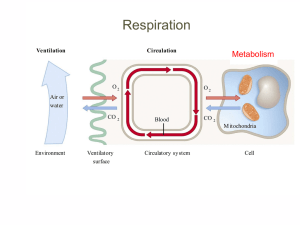
IV. Respiratory Physiology A. Purpose is to supply body and cells with oxygen and remove CO2 produced through cellular activities B. Pulmonary Ventilation - Processes involved: http://www.emptynosesyndrome.org/pics/image-res003.jpg 1. INSPIRATION a. Occurs when alveolar pressure falls below atmospheric pressure b. Contraction of the diaphragm and external intercostal muscles increase the volume in the thorax so the lungs expand c. Expansion of the lungs decreases alveolar pressure so air moves along the pressure gradient from the atmosphere (high pressure) into the lungs (low pressure) d. During forced inspiration accessory muscles of respiration are used. http://faculty.stcc.edu/AandP/AP/imagesAP2/respiration/inspire.jpg 2. EXPIRATION a. Occurs when alveolar pressure is higher in than atmospheric pressure b. Relaxation of the diaphragm and intercostal muscles decrease lung volumeso air moves out of the lungs c. Forced expiration involves contraction of the internal intercostal muscles and abdominal muscles d. A collapsed lung is caused by air in the pleural cavities, airway blockage or a lack of surfactant e. Average respirations = 12/min at rest http://cache.eb.com/eb/image?id=92936&rendTypeId=34 http://www.nlm.nih.gov/medlineplus/en cy/images/ency/fullsize/19589.jpg http://images.emedicinehealth.com/images/eMedicineH ealth/illustrations/pneumothorax.jpg http://www.ispub.com/xml/journals/ija/vol6n2/anastomosis-fig1.jpg V. Pulmonary Air Volumes and Capacities A. Pulmonary Volumes 1. TIDAL VOLUME -Volume of air inspired or expired. (Average tidal volume = 500 mL ) 2. IRV – Inspiratory Reserve Volume – Excess air inhaled during a deep breath (3100 mL above tidal volume) 3. ERV – Expiratory Reserve Volume – the excess air that can be forced out after a normal inhalation (1200mL) 4. MINIMAL VOLUME – the air remaining after the thoracic cavity is opened and the pressure balances, forces out excess volume Provides a medical and legal tool for determining the time of death of a newborn (before or after birth) B. Lung Capacities 1. IC - Inspiratory Capacity – total inspiratory ability of the lungs following a normal expiration 2. FRC – Functional Residual Capacity – the volume of air remaining in lungs after a normal expiration 3. VITAL CAPACITY – the maximum amount of air that can be expired following maximum inpiration 4. TLC – Total Lung Capacity – the maximum amount of air in the lungs following maximal inspiration (sum of all volumes) http://www.geocities.com/doctor_uae/genpath4_img.gif VI. Gas Exchange A. Partial Pressure (p) 1. The pressure exerted by a gas in a mixture of gases. 2. Each gas in a mixture exerts its own pressure; it behave as if it were alone. B. External (pulmonary) Respiration 1. Movement of O2 and CO2 between alveoli of the lungs and the pulmonary area where partial pressure is lower. 2. Each has moves independently 3. High altitude sickness results from lower pO2 so less O2 diffuses into the blood C. Internal (tissue) Respiration 1. Movement of O2 and CO2 between tissues capillaries and tissue cells. 2. O2 and CO2 exchange as a result of difference of p of O2 and CO2 3. Cells are producing CO2 as a result of cell processes Gas exchange animation http://highered.mcgrawhill.com/sites/0072437316/student_view0/chapter44/animations. html# D. Transport 1. Most oxygen is carried by the iron atoms in the heme of the hemoglobin 2. CO combines with hemoglobin much like oxygen but the combination is 200 times stronger 3. HYPOXIA – deficiency of oxygen at the tissue level. http://www.nlm.nih.gov/medlinep lus/ency/images/ency/fullsize/1951 0.jpg 4. CO2 is transported in plasm, combines with globin and 70% is converted to bicarbonate ions (HCO31-) http://www.buteyko.eu/hemoglobinOK.JPG VII. Control A. Nervous Control – The respiratory center consists of the medullary rhythmicity area, the pneumotaxic area and the apneustic area. 1. Medullary sets the rhythm 2. Pneumotaxic and apneustic coordinate inspiration and expiration. http://www.emptynosesyndrome.org/pics/image-res003.jpg