Cardio-11-06
advertisement

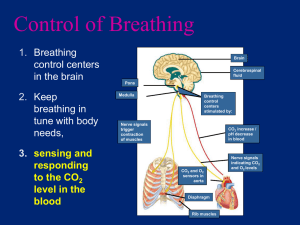
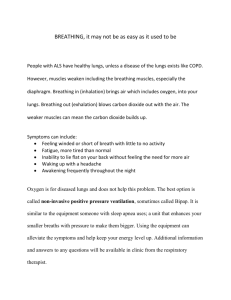
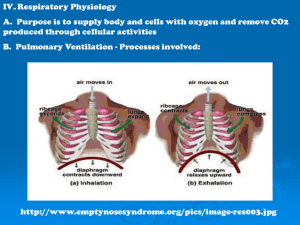
Cardio Notes: 11-06-98 Ventilation = air in and out of the lungs (respiratory zone) Respiration – ability of the body to exchange CO2 and O2 – gas exchange In health, if you increase breaths per minute (BPM), you increase ventilation. In a patient with pneumonia, an increase in breaths per minute does not cause an increase in ventilation. In a patient with atelectasis, an increase in breaths per minute does not cause an increase in ventilation. In fact, if prevents air from getting into the lungs. Hyperventilation syndrome – only healthy lungs can do this. This forces the PaCO2 down in a patient with healthy lungs. Correspondingly, the pH increases and the patient feels dizzy. Kussmaul Respiration – Body’s attempt to increase pH. Happens in diabetic ketoacidosis. 7.35 – 7.45 in the normal range for pH. If the pH drops below 7.30, there is serious acidosis. The fastest way to increase pH is to hyperventilate and and blow off the CO2. This results in Kusmaul Respiration and the patient has ketone (alcohol) breath. If the patient is diabetic and had COPD, this won’t work because the lungs can’t hyperventilate. Hyperventilation is not a disease. It’s a sign of health; an indication that things are working properly. If a person is breathing a lot, but the CO2 levels are increasing, this leads to respiratory failure which lead to death. “Ventilatory failure” = “respiratory failure”. A person should never have a problem getting rid of CO2; it diffuses 8x easier than O2. There are 2 possible causes: hypoventilation and hypoperfusion. Consequently, a V/Q imbalance results from: hypoventilation: decrease in # of breaths per minute (air is not getting to where it needs to go) independent of breaths per minute ( e.g. swallowing a ping pong ball) both restricted AND obstructive lung diseases cause this V decreases so RATIO DECREASES (all pulmonary diseases decrease V/Q) ex: Hamman-Rich syndrome, TB, lung cancer remember: Lung = Low V/Q hypoperfusion: not enough blood getting to lungs infarcts can keep blood from getting to lungs; also pulmonary embolism and gunshot to lungs all circulatory diseases create a high V/Q Peripheral chemoreceptors most sensitive to O2 and pH (text includes CO2 [as if any of us would know] but Dr. Christy likes O2 and pH) carotid bodies: CN IX aortic bodies: CN X A PaO2 < 60mmHg will fire the peripheral chemoreceptors. If the PaO2 falls below 30, however, they will stop firing. An acidotic state (pH < 7.35) regardless of CO2 levels, will also fire these receptors. Either of the above conditions will cause the chemoreceptors to send a message to the respiratory control center in the brain to increase breaths per minute and depth of breathing. They are responsible for HYPOXIC DRIVE: faster, deeper breathing to increase V when PaO2 falls below 60. Atherosclerotic plaques in the aortic and carotid bodies will cause a drop in blood flow. The decreased blood flow will cause the chemoreceptors to fire since there is less total O2. A decrease in blood pressure will also cause these to fire. Central chemoreceptors Quickly stimulated by increasing CO2 (from either hypoventilation or hypoperfusion) CO2 easily diffuses into CSF, causing a decrease in the pH which fires the central chemoreceptors which increases breaths per minute. CO2 + H2O H+ + HCO3Normally, bicarbonate does not cross the blood-brain barrier, but in chronic hypercapnea (>6 weeks duration) the body will begin actively transporting HCO3- into the CNS. This will increase the pH around the chemoreceptors and they will cease to fire. In emphysema (or COPD) the central chemoreceptors become inactive, so only the peripheral chemoreceptors are functioning (hypoxic drive). If O2 levels rise (from patient being placed in an O2 tent) above 60, the hypoxic drive will then shut down and the respiratory center will decrease the rate and depth of breathing. THIS IS BAD!! The body has already compensated for the increased pH by having the kidneys retain more HCO3-. The moral of the story is: don’t put COPD patients on O2. Case: COPD patient BPM = 32 (normal is 12-18) pH = 7.34 (normal is 7.35-7.45) PaCO2 = 65mmHg (normal is 45) HCO3- = 34mEq/L (normal is 21-24 or 25) PaO2 = 50mmHg (normal is 95) the patient is hypercapneic and hypoxic If given O2, the patient gets sleepy and breathes less BPM = 10 pH = 7.26 PaCO2 = 80 HCO3- = 35 PaO2 = 95 leads to ventilatory failure The patient is dying because giving him O2 suppressed the hypoxic drive, which was the only thing telling his body to breathe. Ventilatory failure: defined by CO2 levels and pH, not O2 it is a lung problem ER Mentality: the brain will die without O2, so O2 must be given to the patient. They ignore other metabolic information, not realizing that the patient is relying on increased breaths per minute to live. Giving the patient O2 will decrease breaths per minute and consequently the patient will die (due to V/Q imbalance) Respiratory Therapy: run a tube into the lungs and inflate them. If this works, then CO2 levels decrease. This cannot be done for too long because it can damage lung tissue. It is better than giving O2 through the nose and mouth, but should be administered carefully. Emphysema Patient may be allowed to use an O2 tank for short periods of time. If too much O2 is used, this leads to decreased hypoxic drive and the patient becomes lethargic. Shortness of Breath (SoB): does NOT mean decreasing O2 levels. SoB is due to mechanoreceptors. These mechanoreceptors go all the way to the cortex (feedback). Chemoreceptors do not go to the cortex, so we are not consciously aware of O2 and CO2 levels. Mechanoreceptors: type I and II receptors the muscle spindles in the diaphragm and intercostal muscles monitor expansion of the lungs/ chest costovertebral joints also monitor this the J-receptors in the lungs also contribute Inhalers: work by opening up airways, dilating blood vessels, and firing off mechanoreceptors so that the patient feels better Dyspnea and SoB do NOT equal hypoventilation (different receptors are involved) Controls of Ventilation: Irritant reflex: vagus (parasympathetic) has irritant receptors (peri-bronchial) these increase BPM, but when stimulated chronically, lead to laryngeal constriction, which causes stridor (barking) (the reflex is then out of control) J-receptor reflex: from vagus and spinal afferents, located peri-alveolar (juxta-alveolar) these increase BPM and cause peripheral vasoconstriction in asthmatics, exercise can induce asthma because it bothers these receptors Stimulation of alpha-1 receptors by norepinephrine (NE) decreases the firing threshold of the J-receptors, which causes them to be hypersensitive. An increase in NE can be caused by sympatheticotonia (T-spine subluxations) which may be relieved by thoracic adjustments. Hering-Breuer reflex: smooth muscle afferents suppress ventilation and decrease BPM inflation reflex Deflation reflex: increases BPM happens in pneumonia, atelectasis, pneumothorax, etc. when an area of the lung is deflated, the Hering-Breuer reflex is knocked out