Respiratory Physiology – Gas Exchange
advertisement

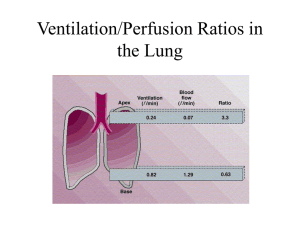
Respiratory Physiology: Gas Exchange Dr Shihab Khogali Ninewells Hospital & Medical School, University of Dundee Understand the difference between pulmonary ventilation and alveolar ventilation, and the significance of anatomical dead space Understand the basic principles of ventilation perfusion matching Understand the significance of alveolar dead space What is This Lecture About? Know that the physiological dead space = anatomical + alveolar dead space Understand the four factors which influence the gas transfer across the alveolar membrane Know the non-respiratory functions of the respiratory system See blackboard for detailed learning objectives Understand the followings in relation to the four factors which influence gas transfer across membranes: The Dalton’s Law of partial pressures. Know that gases move across membranes by partial pressure gradient The role of diffusion coefficient on gas transfer across membranes The effect of membrane surface area and membrane thickness on gas transfer, with the Fick’s Law of diffusion Some inspired air remains in the airways (anatomical dead space) where it is not available for gas exchange Pulmonary Ventilation = tidal volume (ml/ breath) x Respiratory Rate (breath/min) = 0.5 L X 12 breath/min = 6 L/min under resting conditions Alveolar Ventilation is less than pulmonary ventilation because of the presence of anatomical dead space. Alveolar Ventilation = (tidal volume – dead space volume) x Respiratory Rate = (0.5 – 0.15) x 12 = 4.2 L/min under resting conditions. Pulmonary Ventilation & Alveolar Ventilation Fresh air from inspiration Airway dead-space volume (150 ml) Alveolar air After inspiration, before expiration Fig. 13-22, p. 472 Pulmonary Ventilation: Is the volume of air breathed in and out per minute Alveolar Ventilation: Is the volume of air exchanged between the atmosphere and alveoli per minute This is more important as it represent new air available for gas exchange with blood. To increase pulmonary ventilation (e.g. during exercise) both the depth (tidal volume) and rate of breathing (RR) increase. Pulmonary Ventilation & Alveolar Ventilation Fresh air from inspiration Airway dead-space volume (150 ml) because of dead space: It is more advantageous to increase the depth of breathing Alveolar air After inspiration, before expiration It is more advantageous to increase the Depth of Breathing Ventilation Perfusion The transfer of gases between the body and atmosphere depends upon: Ventilation: the rate at which gas is passing through the lungs. Perfusion: the rate at which blood is passing through the lungs Ventilation Perfusion Both blood flow and ventilation vary from bottom to top of the lung Blood Flow 2 Flow V/Q Ratio 1 Ventilation Bottom Lung Position Top The result is that the average arterial and alveolar partial pressures of O2 are not exactly the same. Normally this effect is not significant but it can be in disease. Alveolar Dead Space The match between air in the alveoli and the blood in the pulmonary capillaries is not always perfect Ventilated alveoli which are not adequately perfused with blood are considered as alveolar dead space In healthy people, the alveolar dead space is very small and of little importance (note: the physiological dead space = the anatomical dead space + the alveolar dead space) The alveolar dead space could increase significantly in disease Ventilation Perfusion Match in the Lungs Local controls act on the smooth muscles of airways and arterioles to match airflow to blood flow Accumulation of CO2 in alveoli as a result of increased perfusion decreases airway resistance leading to increased airflow Increase in alveolar O2 concentration as a result of increased ventilation causes pulmonary vasodilation which increases blood flow to match larger airflow Area in which blood flow (perfusion) is greater than airflow (ventilation) Helps balance Large blood flow Helps balance Small airflow CO2 in area O2 in area Relaxation of local-airway smooth muscle Contraction of local pulmonary arteriolar smooth muscle Dilation of local airways Constriction of local blood vessels Airway resistance Vascular resistance Airflow Blood flow Area in which airflow (ventilation) is greater than blood flow (perfusion) Helps balance Helps balance Large airflow Small blood flow CO2 in area O2 in area Contraction of local-airway smooth muscle Relaxation of local pulmonary arteriolar smooth muscle Constriction of local airways Dilation of local blood vessels Airway resistance Vascular resistance Airflow Blood flow Note the Different Effects of O2 1. Partial Pressure Gradient of O2 and CO2 2. Diffusion Coefficient for O2 and CO2 3. Surface Area of Alveolar Membrane 4. Thickness of Alveolar Membrane Four Factors Influence The Rate of Gas Exchange Across Alveolar Membrane Gases move across cell membranes etc by pressure gradient The partial pressure of a gas determines the pressure gradient for that gas The partial pressure of gas (1) in a mixture of gases that don’t react with each other is: The pressure that gas (1) would exert if it occupied the total volume for the mixture in the absence of other components Thus if the total pressure of the gas mixture is 100 kPa; and half of the mixture is gas (1): the partial pressure for gas (1) is 50 kPa What is Partial Pressure of Gas? Dalton’s Law of Partial Pressures The Total Pressure exerted by a gaseous mixture = The sum of the partial pressures of each individual component in the gas mixture Ptotal = P1 + P2 +…+ Pn The partial pressure of gas is: The pressure that one gas in a mixture of gases would exert if it were the only gas present in the whole volume occupied by the mixture at a given temperature. Overview of Respiration Gases move from higher to lower partial pressures (partial pressure gradient) Note units in the diagram (mmHg). Here in UK you we use kPa (kilopascals) but Americans and American texts use mmHg. To convert divide mmHg by 7.5. Across Pulmonary Capillaries: O2 partial pressure gradient from alveoli to blood = Atmospheric air Inspiration Expiration 60 mm Hg (8 kP) Net diffusion gradients for O2 and CO2 between the lungs and tissues 100 – 40 mmHg i.e. (13.3- 5.3 kP) CO2 partial pressure gradient Alveoli from blood to alveoli = 6 mm Hg (0.8 kP) 46 – 40 mmHg i.e. (6.1 – 5.3 kP) Pulmonary circulation Across Systemic Capillaries: O2 partial pressure gradient from blood to tissue cell = > 60 mm Hg (8 kP) 100 – < 40 mmHg i.e. (13.3- < 5.3 kP) Systemic circulation CO2 partial pressure gradient from tissue cell to blood = > 6 mm Hg (0.8 kP) > 46 – 40 mm Hg i.e. (> 6.1 – 5.3 kP) Tissues But the partial pressure gradient for CO2 is much smaller than the partial pressure gradient for O2??? What offset the difference in partial pressure gradient for CO2 and O2? CO2 is more soluble in membranes than O2. The solubility of gas in membranes is known as the Diffusion Coefficient for the gas. The diffusion coefficient for CO2 is 20 times that of O2 The lungs provide a very large surface area with thin membranes to facilitate effective gas exchange Effect of surface Area & Membrane Thickness on Gas Diffusion Fick’s Law of diffusion The airways divides repeatedly to increase the surface area for gas The amount of gas that moves exchange The small airways form outpockets (the alveoli). This help increase the surface area for gas exchange in the lungs The lungs have a very extensive pulmonary capillary network Remember: the pulmonary circulation receives the entire cardiac output across a sheet of tissue in unit time is proportional to the area of the sheet but inversely proportional to its thickness The Respiratory Tree Respiratory Membranes Alveoli: Thin-walled inflatable sacs • Function in gas exchange • Walls consist of a single layer of flattened Type I alveolar cells Pulmonary capillaries encircle each alveolus Narrow interstitial space Four Factors Influence the Rate of Gas Transfer Across The Alveolar Membrane Nonrespiratory Functions of Respiratory System Route for water loss and heat elimination Enhances venous return (Cardiovascular Physiology) Helps maintain normal acid-base balance (Respiratory and Renal Physiology) Enables speech, singing, and other vocalizations Defends against inhaled foreign matter Removes, modifies, activates, or inactivates various materials passing through the pulmonary circulation Nose serves as the organ of smell