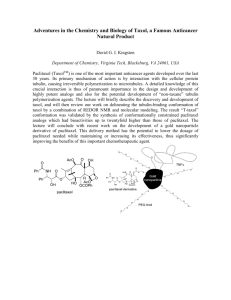
Marth - the Gynecologic Cancer InterGroup

Ovarian Cancer
Diagnosis
Surgery
First-line Chemotherapy
Consolidation
Platinum-sensitive Recurrence
Surgery
Chemotherapy
Platinum-resistant Recurrence
Closed Trials
Ovarian Cancer
Diagnosis
Open Trials
EORTC 55971
CHORUS
Surgery
EORTC 55971/CHORUS
Upfront Surgery vs Neoadjuvant Chemotherapy
Patients
Leading closed / 550
EORTC
Participating NCIC CTG
Presentation planned at IGCS 2008
Closed Trials
AGO-OVAR-9
CT ± GEM
SCOTROC-4
ICON-7
GOG-218
EORTC 55041
Tarceva
Ovarian Cancer
Open Trials
First-line
Chemotherapy
Consolidation
AGO-OVAR-9
Carbo Paclitaxel +/- Gemcitabine
Patients closed 1742
Leading AGO-OVAR
Participating GINECO, NSGO,
SCOTROC 4
Carbo Flat Dosing vs Intrapatient Dose Escalation
Patients
Leading closed 932
SGCTG
Participating ANZGOG
Tarceva Trial EORTC 55041
Primary Chemotherapy
Tarceva consolidation 2 years
Control
Patients closed / 835
Leading EORTC
Participating AGO-AUSTRIA, ANZGOG, GINECO,
MRC/NCIC, MANGO
ICON-7
TC ± BEVACIZUMAB
Patients
Leading closed / 1520
MRC/NCRI
Participating NCIC CTG, AGO OVAR, GINECO, GEICO
EORTC, ANZGOG, NSGO
GOG 218
CT vs CT + Bevacizumab Placebo vs
CT + Bevacizumab concurrent and extended
Patients closed / 1800
Leading GOG
Participating ECOG, NCCTG, NSABP, SWOG
Closed Trials
AGO-OVAR OP-2
Desktop II
CALYPSO
Ovarian Cancer
Platinum-sensitive
Recurrence
Surgery
Chemotherapy
Open Trials
Platinum-resistant
Recurrence
AGO-OVAR-OP.2 DESKTOP II
Evaluation of predictive factors for complete resection in platinum-sensitive recurrent ovarian cancer
Patients
Leading closed/412
AGO-OVAR
Participating AGO-AUSTRIA, MITO, selected Canadian+Australian centers
Report IGCS 2008
AGO DESKTOP OVAR II – FLOW CHART
08/06 – 03/08: Screening of 516 pts with platinum-sensitive relapse in 46 centres
Score positive
261 pts (51%)
Score negative
255 pts (49%)
Surgery
148 pts
(57%)
No surgery
113 pts
(43%)
Surgery
80 pts
(31%)
No surgery
175 pts
(69%)
Study collective:
AGO score +
1st relapse
129 pts (87%)
2nd relapse
19 pts
(13%)
1st relapse
64 pts
(80%)
2nd relapse
16 pts
(20%)
Selection process:
228 pts (44.2%) had cytoreductive surgery for recurrent OC
-> Primary study collective (AGO score +, 1st relapse) : 129 pts (25%)
© P. Harter 2008
50
40
30
20
10
0
100
90
80
70
60
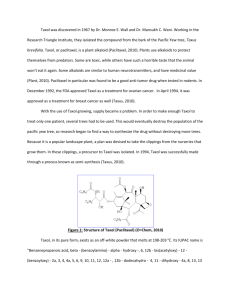
AGO DESKTOP OVAR II – SURGICAL RESULTS
Frequency of complete resection by applying the AGO Score
75 76
68
DESKTOP
Hypothesis
Score positive all patients
Score positive
1st relapse
Score positive
2nd relapse complete resection in 76% of the study collective =
AGO score could predict complete resection in at least 2 out of 3 patients
© P. Harter 2008
AGO DESKTOP OVAR II: CONCLUSIONS
A surgical multicentre study within the GCIG is feasible and could answer complex questions in an appropriate interval
The AGO-Score is a useful and reliable tool to predict complete resection in at least 2 out of 3 patients
First score succesfully validated in surgery for ovarian cancer
The comorbidity is comparable to surgery in primary ovarian cancer
Outcome in the score negative subgroup will be further analysed
© P. Harter 2008
C
ALYPSO
TC vs C + Caelyx
Patients
Leading closed / 976
GINECO
Participating
AGO-AUSTRIA, AGO-OVAR,
ANZGOG, EORTC, MANGO,
MITO, NCIC/CTG, NSGO
Presentation ASCO 2009
Closed Trials
Ovarian Cancer
Diagnosis
Open Trials
EORTC 55971
CHORUS
Surgery
AGO-OVAR OP-3
LION
AGO – OVAR OP.3 (LION)
L ymphadenectomy I n O varian N eoplasms epithelial invasive ovarian cancer
FIGO IIB - IV
System. Lymphadenectomy
pelvic
para-aortic
ECOG 0/1 and no CI against LNE no visible extraand intra-abdominal tumor residuals
R n = 640 no Lymphadenectomy no bulky lymph nodes
Endpoints: OS, PFS, QoL Strata: centre, PS ,age
Supported by Deutsche Forschungsgemeinschaft
Participating groups/sites:
AGO Study Group (24 centres initiated)
MITO (11 centres planned – ethical approval 06/09
)
KGOG
AGO Austria
Single sites: Leuven
Recruitment: 26 / 640 pts
Closed Trials
AGO-OVAR-9
CT ± GEM
SCOTROC-4
ICON-7
GOG-218
EORTC 55041
Tarceva
Ovarian Cancer
First-line
Chemotherapy
Consolidation
Open Trials
JGOG-3017
Clear cell carcinoma mEOC
MITO-7
JGOG IP Trial
AGO-OVAR-12
AGO-OVAR-16
VEG 110655
MITO-7
Weekly CT vs 3-weekly CT (QoL)
Patients
Leading
25 / 500
MITO
Participating MaNGO, AGO-OVAR
First line weekly carboplatin and paclitaxel vs every 3 weeks carboplatin/paclitaxel in patients with ovarian cancer: the MITO – 7 trial
Aim of the trial is to compare the two schedules in terms of quality of life
Risk of progression at 18 months as primary end-point
RANDOM
Carboplatin AUC 6
Paclitaxel 175 mg/mq day 1 - every 21days
Carboplatin AUC 2
Paclitaxel 60 mg/mq day 1,8 15 - every 21days
JGOG IP Trial
IP vs IV carboplatin + weekly Paclitaxel
Patients
Leading
Participating
JGOG
P LANNED J APANESE IP T RIAL
Epithelial Ovarian Cancer
Stages II-IV
Excluding Clear Cell Carcinoma
Randomization
Paclitaxel 80 mg/m2 IV Weekly
Carboplatin AUC 6 IV
Q21, 6-8 Cycles
Paclitaxel 80 mg/m2 IV Weekly
Carboplatin AUC 6 IP
Q21, 6-8 Cycles
Primary Endpoint: PFS
Secondary Endpoint: OS, Toxicity, QOL, Cost
NCIC CTG OV.21
IP/IV Platinum/T vs IV CT optimally debulked following NACT
Patients
Leading
0 / 780
NCIC CTG
Participating GEICO, NCRI, SWOG
Basic Design
Patients with EOC
3-4 cycles neoadjuvant chemo
Initial surgery: < 1 cm residual
3 cycles
IV Carbo/Taxol
3 cycles IP/IV platinum and taxol
Endpoints: PFS and OS
R
Phase II
IV Carbo
IV Taxol
IP Carbo (Taxol)
IV Taxol
IP Cisplatin (Taxol)
IV Taxol
Then…..
This or…..
R
Phase II
IV Carbo
IV Taxol
IP Carbo (Taxol)
IV Taxol
IP Cisplatin (Taxol)
IV Taxol
Phase III
IV Carbo
IV Taxol
IP Carbo (Taxol)
IV Taxol
This…..
R
Phase II
IV Carbo
IV Taxol
IP Carbo (Taxol)
IV Taxol
IP Cisplatin (Taxol)
IV Taxol
Phase III
IV Carbo
IV Taxol
IP Cisplatin (Taxol)
IV Taxol
Study Arms: Phase II
Arm 1
Day 1:Paclitaxel 135 mg/m2 IV day 1 plus carboplatin AUC 5 (measured)/ AUC
6 (calculated) IV
Day 8:Paclitaxel 60 mg/m2 IV day 8
Q 21 days x 3 cycles
Study Arms: Phase II
Arm 2
Day 1: Paclitaxel 135 mg/m2 IV plus
Cisplatin 75 mg/m2 IP
Day 8: Paclitaxel 60 mg/m2 IP
Q 21 days x 3 cycles
Study Arms: Phase II
Arm 3
Day 1: Paclitaxel 135 mg/m2 IV plus carboplatin AUC 5 (measured)/ AUC
6 (calculated) IV IP
Day 8: Paclitaxel 60 mg/m2 IP
Q 21 days x 3 cycles
Statistics Phase III Portion
• Progression free survival:
– Seek improvement of IP over control with hazard ratio of 0.8 (Median increase PFS 4.3 mo, 17
21.3 mo)
– 80% power, 2-sided alpha 0.05
– Need 631 progression events
– To detect need additional 630 patients randomized after phase II completed
– Overall Survival: Same numbers will detect hazard ratio of 0.80 once 631 deaths seen (10 month increase in median survival)
– Total no of patients =780
AGO-OVAR-12
Carbo Paclitaxel +/- BIBF 1120 (Vargatef)
Patients 0 / 1300 (2:1 random)
Leading AGO-OVAR
Participating
AGO Austria, BGOG, GINECO,
MANGO, MITO, NSGO, US Oncology
AGO-OVAR12
Multicenter, randomised, double-blind, Phase III trial to investigate the efficacy and safety of Vargatef (BIBF 1120) in combination with standard treatment of carboplatin and paclitaxel compared to placebo plus carboplatin and paclitaxelin patients with advanced ovarian cancer
C
T
C
T
C
T
C
T
C
T
C
T = Vargatef 2 x 200 mg po qd
S
U
R
G
E
R
Y
R
2
1
C = Carboplatin AUC 5-6 d1
T = Paclitaxel 175 mg/m 2 (3h) d1 q21d / 6 courses
Vargatef / Placebo :
- no intake on days of chemotherapy
- dose: 200 mg po bid (combi + mono)
- dose adaptation in case of undue toxicity
- max. duration of 120 weeks in non-progressing pts
C
T
C
T
C
T
C
T
C
T
C
T
= Placebo n=1300
120 weeks
AGO-OVAR 16
First Line Chemotherapy
Pazopanib consolidation 1 yr
Control
Patients
Leading
0 / 900
AGO-OVAR
Participating AGO Austria, ANZGOG, BGOG, GEICO, GINECO,
ICORG, JGOG, KGOG, MANGO, MITO, NSGO, US-Sites: California
Consortium, NY GOG, SWOG
AGO-OVAR16
A Phase III Study to Evaluate the Efficacy and Safety of Pazopanib
Monotherapy Versus Placebo in Women Who Have not Progressed after First Line Chemotherapy for Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
First-line
Chemotherapy
(allow ip, neoadj)
Screening
Baseline
If not PD
R
A
N
D
O
M
I
Z
E
Treatment
Period
Pazopanib
(12 months)
Post-Treatment
Period
Observation
(to PD)
Placebo
(12 months)
Follow-up
Period
Survival
Follow-up
(post-PD)
ICON8 Stage 1 trial design
Randomisation weighted in favour of research arms 1:2:2:2:2:2
Number of patients requires further discussion on what is needed to demonstrate feasibility
Primary surgery
Randomised after surgery
NAC
Randomised before neoadjuvant chemo to 3 cycles chemo, surgery, then 3 cycles chemo)
Standard
ARM1: C q 3/52
P q 3/52
GOG218 15m bevacizumab 15mg/kg
(concurrent and extended) or bevacizuamb 15mg/kg 6 cycles
(concurrent only)
ICON7 12 months treatment with bevacizumab 7.5mg/kg
ICON8: bevacizumab 7.5mg/kg for 6 cycles (concurrent only)
~GOG218 & ICON7
ARM2: C q 3/52
P q 3/52
Bevacizumab q 3/52
JGOG study
ARM3: C q 3/52
P q 1/52
Novel
ARM4: C q 3/52
P q 1/52
Bevacizumab q 3/52
Proposed MITO
ARM5: C q 1/52
P q 1/52
NOVEL
ARM6: C q 1/52
P q 1/52
Bevacizumab q 3/52
Aim of stage 1 is to establish which arms should be taken into stage 2 based.
Primary outcome measures:
Toxicity
Feasibility
ICON8 Stage 2 trial design if ICON7 and GOG 218 are positive are ‘positive’ for PFS
Option 1 2:1 randomisation*
Total 2000 patients
~GOG218 & ICON7
ARM2: C q 3/52
P q 3/52
Bevacizumab q 3/52
GOG218 concurrent arm not worse than control will provide support for
6 cycles of bevacizumab
JGOG study
ARM3: C q 3/52
P q 1/52
Subgroup analyses to explore effect of effect of treatments in subgroups defined by primary surgery or NAC
Primary surgery
Randomised after surgery
NAC
Randomised before chemo to 3 cycles chemo, surgery, then 3 cycles chemo)
NOVEL
ARM4: C q 3/52
P q 1/52
Bevacizumab q 3/52
Proposed MITO
ARM5: C q 1/52
P q 1/52
NOVEL
ARM6: C q 1/52
P q 1/52
Bevacizumab q 3/52
2:1 randomisation in favour of standard arm ( 800 patients) and 400 in each research arm gives 1,200 patients in each pairwise comparison loses a little power but will save patients (total 2000)
PRIMARY OUTCOME MEASURE:
OS
SECONDARY OUTCOME MEASURES:
PFS
TOXICITY
HE
QOL
TR
ICON 8 If bevacizumab trials ‘negative’ for PFS
3 arm 1:1: 1 randomisation
600 patients per arm, Total 1800- 3yrs recruitment 2 years follow up
Primary surgery
Randomised after surgery
Neoadjuvant chemotherapy randomised before chemo to 3 cycles chemo, surgery, then
3 cycles chemo)
Standard
ARM1: C q 3/52
P q 3/52
JGOG study
ARM3: C q 3/52
P q 1/52
Aim of trial is to compare efficacy of dose dense chemotherapy against standard 3 weekly regimens
(Arm 1 vs Arm 2 and Arm 1 vs Arm 3
If dose dense regimens both better than standard, compare dose dense paclitaxel with dose dense carboplatin and paclitaxel (Arm 2 vs Arm 3)
Subgroup analyses to explore effect of effect of treatments in subgroups defined by primary surgery or NAC
Proposed MITO
ARM5: C q 1/52
P q 1/52
3 weeks out of 4
Primary outcome measure:
OS
Secondary outcome measures:
PFS
Toxicity
HE
QoL
TR
Closed Trials
AGO-OVAR OP-2
Desktop II
CALYPSO
Ovarian Cancer
Platinum-sensitive
Recurrence
Surgery
Chemotherapy
Open Trials
AGO-OVAR OP-7
Desktop III
HECTOR
C-Topo vs CT or CG
ICON-6
MITO-8
Platinum-resistant
Recurrence
SGCTG / NCRI
AGO-OVAR-OP.4 DESKTOP III
Cytoreductive surgery vs NO surgery in platinum-sensitive recurrent EOC
Patients
Leading
Participating ?
0 / 385
AGO-OVAR
AGO-OVAR DESKTOP III (Protocol AGO - OVAR OP.4)
A randomized trial evaluating cytoreductive surgery in patients with platinum-sensitive recurrent ovarian cancer
Complete resection seems feasible and a positive AGO-score
Strata:
Platinum-free-interval
6-12 vs > 12 months
1st line platinum based chx: yes vs no
R
A
N
Cytoreductive surgery platinum-based chemotherapy* recommended D
O no surgery
M
* Recommended platinum-based chemotherapy regimens:
- carboplatin/paclitaxel
- carboplatin/gemcitabine
- carboplatin/pegliposomal doxorubicin
(if calypso-trial shows equivalence to carboplatin-paclitaxel)
or other platinum combinations in prospective trials
HECTOR
Carbo Topo vs Chemo (CT or CG) in recurrent
Platinum-sensitive ovarian cancer
Patients
Leading
452 / 550
NOGGO/AGO-OVAR
Participating AGO-AUSTRIA, GEICO
MITO-8
PLD vs CT cross-over in 6-12 m platinum-free interval
Patients 25 / 253
Leading MITO
Participating MaNGO, AGO-OVAR
Trial design
The objective of this trial is the efficacy determined through analysis of overall survival (OS) of the different sequence
(CP →PLD vs PLD→CP) in recurrent ovarian cancer patients with platinum-free interval 6-12 months
CARBOPLATIN AUC 5 +
PACLITAXEL 175 mg/mq day1 every21gg
LIPOSOMAL
DOXORUBICIN
40 mg/mq day1 every 28 days
RANDOM
Cross-over at
Progression
LIPOSOMAL
DOXORUBICIN 40 mg/mq day1 every 28 days
CARBOPLATIN AUC 5 +
PACLITAXEL 175 mg/mq day1 every 21 days
Ovarian Cancer
Closed Trials
AGO-OVAR-9
CT ± GEM
SCOTROC-4
ICON-7
GOG-218
EORTC 55041
Tarceva
AGO-OVAR OP-2
Desktop II
CALYPSO
Diagnosis
Surgery
First-line Chemotherapy
Consolidation
Platinum-sensitive Recurrence
Surgery Chemotherapy
Platinum-resistant Recurrence
Open Trials
JGOG-3017
Clear cell carcinoma mEOC
MITO-7
JGOG IP Trial
AGO-OVAR-12
AGO-OVAR-16
VEG 110655
AGO-OVAR OP-7
Desktop III
HECTOR
C-Topo vs CT or CG
ICON-6
MITO-8
SGCTG / NCRI
GCIG has demonstrated to perform very efficient important clinical trials which have changed the standard of care in the treatment of ovarian cancer
Main focus has been first-line chemotherapy
Surgical questions have been raised recently
Treatment options in platinum-resistant recurrent disease should be further develloped