Dyslipoproteinemia and
Atherosclerosis
Daniel W. Stock MD
Founding Diplomate, American Board of Clinical
Lipidology
Member, National Lipid Association and Midwest
Lipid Association
Former Adjunct Clinical Professor
Indiana University School of Medicine
Disclosures
Speakers Bureau:
Liposcience Inc.
Lilly Pharmaceuticals Inc.
Warner-Chilcott Inc.
•Framingham showed ↑’ing risk with
↑’ing LDL and ↓’ing HDL cholesterol
CAD
status
LDL-C HDL-C AMCE
∆
4S
LIPID
CARE
2º
2º
2º
188
150
139
46
36
39
34%
34%
22%
WOSCOPS
AFCAPS/TexCAPS
ASCOT-LLA
HPS
1º
1º
1º
1º& 2º
193
150
131
NA
44
36
50
NA
31%
37%
36%
17%
JUPITER
VA-HIT
1º
2º
108
112
49
32
44%
22%
Lipid Analysis Shortcomings
• 50% of Framingham AMCE patients had LDL <130
mg/dl
• 75% of Framingham AMCE patients < 55 yo had
LDL <130 mg/dl
• Majority of lipid trial patients did not benefit from
therapy
• On-treatment lipids did not predict clinical outcome
• Forces the treatment of low-risk individuals in
order to protect high-risk individuals
Number of patients
5
50
500
Beta HCG level
5000
500,000
30
number of patients
25
20
15
10
5
0
0
100
200
300
total cholesterol
400
500
LDL Cholesterol
Number of patients
“Lipids” and Atherosclerosis
• Atherosclerosis occurs because of abnormal
lipoproteins and/or lipoprotein kinetics, not
abnormal lipid levels.
“… all abnormalities in plasma lipid concentrations, or
dyslipidemia, can be translated into dyslipoproteinemia.”
“… the shift of emphasis to lipoproteins offers distinct
advantages in the recognition and management of such
disorders.”
Fredrickson et al., NEJM 1967; 276: 148
Total Cholesterol (+)
VLDL-C
+
LDL-C
(+)
+
+
HDL-C
( -)
+
- --
(+)
IDL
+ +
+
+ +
+
LDL
+
+
Association with CHD: Positive (+) or Negative (-)
++
Lipoprotein Particles
Apolipoprotein
Apolipoprotein
POLAR
SURFACE COAT
NON-POLAR
LIPID CORE
Phospholipid
Free cholesterol
Cholesterol Ester
Triglyceride
Apolipoprotein
Among Individuals At The Same LDL-C
Level, The Number of LDL Particles Vary
At the same LDL cholesterol, with small versus large size LDL Particles
Up to 70%
More Particles
100 mg/dL
100 mg/dL
Large
LDL
Small
LDL
Cholesterol
Balance
Otvos JD, et al. Am J Cardiol 2002;90(suppl):22i-29i
Cromwell WC, et al. J Clin Lipidology. 2007;1(6):583-592.
Among Individuals At The Same LDL-C
Level, The Number of LDL Particles Vary
At the same LDL cholesterol, with the same size LDL Particles
(at any triglyceride level)
Up to 40%
More Particles
100 mg/dL
100 mg/dL
Normal Cholesterol
Carried Per Particle
Less Cholesterol
Carried Per Particle
Cholesterol
Balance
Otvos JD, et al. Am J Cardiol 2002;90(suppl):22i-29i
Cromwell WC, et al. J Clin Lipidology. 2007;1(6):583-592.
LDL-C often fails to reflect the number of
LDL particles and the CHD risk they confer
The number of LDL particles (LDL-P™) varies widely among patients with similar
LDL-C values. In this analysis, patients with an LDL-C between 95 mg/dL and
105 mg/dL have highly variable LDL particles, and thus variable CHD risk.
Otvos JD, Jayarajah E, Cromwell, WC. AJC 2002;90(8A):22i-29i
LDL-C Often Fails to Reflect the
Number of LDL Particles
• LDL particles can be large or small, and the amount of cholesterol
contained within these particles varies widely.
Otvos JD, Jayarajah E, Cromwell, WC. AJC 2002;90(8A):22i-29i
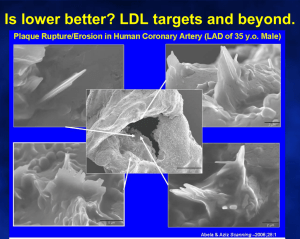
Pathophysiology of Atherosclerosis
–
Particle Movement
Gradient driven
“The rate of passive diffusion is
increased when the circulating
levels of LDL are elevated.” 1
Adhesion
molecules
Enhanced Endothelial
Dysfunction
PAI-1
MCP-1
Monocyte
Colonystimulating
factors
Tissue
factor
Endothelial cells
Mildly modified LDL
Extensively modified LDL
–
Particle Retention
Lipoprotein particle
binding to proteoglycans
1 Weissberg
Oxidative Modification
–
Enhanced
Macrophage Uptake
Modified / retained lipoproteins
PL, Rudd JH. Textbook of Cardiovascular Medicine 2nd ed. 2002. p. 6.
Alternative Measures of LDL as
Predictors of CHD Events in VA-HIT
p<0.001
Odds Ratio per 1-SD Increment
of on-trial value
1.3
1.2
p=0.17
1.1
1
p=0.25
LDL-C
p=0.31
NonHDL-C
Adjusted for treatment, age, hypertension,
smoking, BMI, and diabetes
ApoB
LDL-P
Circulation 2006;113:1556-63
Odds Ratio per 1-SD Decrement
of on-trial value
Alternative Measures of HDL as
Predictors of CHD Events in VA-HIT
1.5
p<0.001
1.4
1.3
1.2
p=0.18
1.1
p=0.42
1
HDL-C
Adjusted for treatment, age, hypertension,
smoking, BMI, and diabetes
ApoA-1
HDL-P
Circulation 2006;113:1556-63
Fig. 2 Survival Curves for Framingham Subjects with
Concordant LDL-C and LDL-P
1.00
0.98
Low LDL-P & Low LDL-C
(n=1,249)
0.96
Event-Free Survival
0.94
0.92
0.90
0.88
High LDL-P & High LDL-C
(n=1,251)
0.86
0.84
0.82
0.80
0.78
0.76
0.74
0
1
2
3
4
5
6
7
8
9
10 11 12 13 14 15 16
Years of Follow-up
Fig. 2 Survival Curves for Framingham Subjects with
Discordant LDL-C and LDL-P
1.00
0.98
0.96
Event-Free Survival
0.94
0.92
0.90
High LDL-C
Low LDL-P
(n=284)
0.88
0.86
0.84
Low LDL-C
High LDL-P
(n=282)
0.82
0.80
0.78
0.76
0.74
0
1
2
3
4
5
6
7
8
9
10 11 12 13 14 15 16
Years of Follow-up
Fig. 2 Survival Curves for Framingham Subjects with
Concordant and Discordant LDL-C and LDL-P
1.00
0.98
Low LDL-P & Low LDL-C
(n=1,249)
0.96
Event-Free Survival
0.94
0.92
0.90
0.88
High LDL-P & High LDL-C
(n=1,251)
0.86
High LDL-C
Low LDL-P
(n=284)
0.84
Low LDL-C
High LDL-P
(n=282)
0.82
0.80
0.78
0.76
0.74
0
1
2
3
4
5
6
7
8
9
10 11 12 13 14 15 16
Years of Follow-up
NMR LDL-P vs. Lipids
NMR LDL-P significantly better risk predictor
than all lipid panel parameters
Framing. Offspring Study*†
Cardiovascular Health Study*
VA-HIT*†
PLAC-1*
Healthy Women Study*
MESA*†
NMR LDL-P significantly better risk predictor
than all lipid panel parameters except
TC/HDL-C
Women’s Health Study*†
LDL pattern not an independent predictor of
risk after NMR LDL-P adjustment
Framing. Offspring Study*†
VA-HIT*†
Women’s Health Study*†
MESA*†
* Independent of sex, age, smoking status and BP
† Superior predictor to and independent of apo B-100
NMR HDL-P vs. HDL-C
NMR HDL-P better risk predictor Framing. Offspring Study*†
than HDL-C
PLAC-1*
VA-HIT*†
MESA*†
Women’s Health Study*†
NMR HDL-P better predictor of
therapy response that HDL-C
PLAC-1*
VA-HIT*†
* Independent of sex, age, smoking status and BP, and all lipid panel parameters
† Superior predictor to and independent of apo B-100
Treatment Summary
LDL-P
Small
LDL-P
LDL
Size
HDL-P
Large
VLDL-P
or or
any
Ezetimibe
or or
any
Niacin
?
any
BAS
Fibrates/
pioglitazone
Only
Only
Only
Statins
Ω-3 FA
Patient Bradley
• 65 YO WM, 71” tall 198#, BP 110/70m, never smoker, neg FHx of
premature atherosclerosis, Dx of BPH, Dyslipoproteinemia, Atrial
fibrillation, ED
• Lipoprotein Therapy: Pravastatin 20 MG QD
TC = 145
LDL-C = 93 (15th)
HDL-C = 39 (20th)
TG = 66
Non HDL-C = 106 (10th)
LDL-P = 1560 (60th)
HDL-P = 28.7 (40th)
Small LDL-P = 1369
LDL Particle Size = 19.8
Large HDL-P = 6.8 (50th)
Large VLDL-P = 0.1
Pattern B = 20.5-18.0
Patient Bradley
• 65 YO WM, 71” tall 198#, BP 110/70m, never smoker, neg FHx of
premature atherosclerosis, Dx of BPH, Dyslipoproteinemia, Atrial
fibrillation, ED
• Changed from pravastatin to rosuvastatin 10 MG QD.
TC = 123
LDL-C = 68 (3rd)
HDL-C = 42 (25th)
TG = 63
Non HDL-C = 81 (2nd)
LDL-P = 1045 (20th)
HDL-P = 27.7 (38th)
Small LDL-P = 722
LDL Particle Size = 20.9
Large HDL-P = 9.0 (75th)
Large VLDL-P = 0.2
Pattern A = 23.0-20.6
Patient Gregory
• 43 YO WM, 68” tall 155#, BP 110/80m, never smoker, non-drinker,
regular exercise,+ FHx of premature atherosclerosis, No medical
diagnoses.
• Lipoprotein Therapy: None
TC = 199
LDL-C = 132 (50th)
HDL-C = 54 (75th)
TG = 67
Non HDL-C = 145 (40th)
•
•
CXR: Mild Aortic Calcification
Carotid U/S: minimal non-calcifying plaque L CCA and bilat ICA
LDL-P = 1147 (30th)
HDL-P = 25.0 (18th)
Small LDL-P = 517
LDL Particle Size = 21.6
Large HDL-P = 9.3 (80th)
Large VLDL-P = 0.7 (20th)
Pattern A = 23.0-20.6
Patient Gregory
• 43 YO WM, 68” tall 155#, BP 110/80m, never smoker, non-drinker,
regular exercise,+ FHx of premature atherosclerosis, No medical
diagnoses.
• Lipoprotein Therapy: simvastatin 20 MG QD
TC = 118
LDL-C = 69 (< 2nd)
HDL-C = 42 (28th)
TG = 33
Non HDL-C = 76 (< 2nd)
LDL-P = 808 (3rd)
HDL-P = 26.2 (21st)
Small LDL-P = 508
LDL Particle Size = 21.1
Large HDL-P = 8.3 (78th)
Large VLDL-P = 0.0 (5th)
Pattern A = 23.0-20.6
Patient Gregory
• 43 YO WM, 68” tall 155#, BP 110/80m, never smoker, non-drinker,
regular exercise,+ FHx of premature atherosclerosis, No medical
diagnoses.
• Lipoprotein Therapy: lovastatin/ER niacin 1000/40 MG QD
TC = 152
LDL-C = 97 (19th)
HDL-C = 50 (65th)
TG = 25
Non HDL-C = 102 (10th)
LDL-P = 907 (7th)
HDL-P = 31.0 (60th)
Small LDL-P = 563
LDL Particle Size = 21.1
Large HDL-P = 12.4 (95th)
Large VLDL-P = 0.1 (10th)
•
Pattern A = 23.0-20.6
Carotid U/S: No demostrable plaque either carotid artery
Patient Fancher
•
•
•
53 YO WF, 64” tall, 158#, BP 120/80, Never smoker, Dx IFG (FBS 110),
menopause, s/p Radical Urinary Cystectomy and continent colon reservoir
for Transitional Bladder CA
Current Meds: None
Lipoprotein therapy: None
TC = 187
LDL-C = 84 (4th)
HDL-C = 55 (52th)
TG = 242
Non HDL-C = 132 (30th)
LDL-P = 763 (3rd)
HDL-P = 40.6 (80th)
Small LDL-P = 443
LDL Particle Size = 21.1
Large HDL-P = 5.4 (60th)
Large VLDL-P = 5.9
Pattern A = 20.5-18.0
Patient Chew
•
•
•
46 YO WF, 67” tall, 202#, BP 120/76, no tobacco since 93, 16 pack-year hx
previously, Dx of menopause, Dyslipoproteinemia, IFG, Hepatic steatosis
Current Meds: levothyroxine 150 MCG QD, spironolactone 50 MG QD, CEE
0.625 QD, HCTZ 12.5 QD, escitalopram 20 MG QD, buproprion 150 MG
QD
Lipoprotein therapy: rosuvastatin 10 MG QD
TC = 192
LDL-C = 73 (2nd)
HDL-C = 58 (55th)
TG = 303
Non HDL-C = 134 (30th)
LDL-P = 1913 (85th)
HDL-P = 39.7 (80th)
Small LDL-P = 1404
LDL Particle Size = 20.4
Large HDL-P = 12.3 (95th)
Large VLDL-P = 13.7
Pattern B = 20.5-18.0
Patient Chew
•
•
•
46 YO WF, 67” tall, 202#, BP 120/76, no tobacco since 93, 16 pack-year hx
previously, Dx of menopause, Dyslipoproteinemia, impaired fasting glucose,
Hepatic steatosis
Current Meds: levothyroxine 150 MCG, spironolactone 50 MG QD, CEE
0.625 QD, HCTZ 12.5 QD, lexapro 20 MG QD, buproprion 150 MG QD
Added Omega-3 Fatty Acid Ethyl Esters 4 G QD to rosuvastatin 10 MG QD
TC = 146
LDL-C = 62 (1st)
HDL-C = 48 (18th)
TG = 181
Non HDL-C = 98 (7th)
LDL-P = 1434 (50th)
HDL-P = 36.2 (70th)
Small LDL-P = 1103
LDL Particle Size = 20.45
Large HDL-P = 7.2 (60th)
Large VLDL-P = 2.6
Pattern B = 20.5-18.0
Patient Jones
•
•
•
60 YO BM, 72” tall, 194#, 150/70, never smoker, Dx HTN,
Dyslipoproteinemia
Current Meds: ramipril 10 MG QD, spironolactone/HCTZ 12.5/12.5 MG QD
Lipoprotein Therapy: lovastatin/ER niacin 1000/40 MG QD
TC = 158
LDL-C = 80 (5th)
HDL-C = 62 (75)
TG = 79
Non HDL-C = 96 (5th)
LDL-P = 1459 (50th)
Small LDL-P = 1067
LDL Particle Size = 20.7
Large HDL-P = 6.8 (50th)
Large VLDL-P = 0.1
Pattern A = 23.0 - 20.6
Patient Jones
•
•
•
60 YO BM, 72” tall, 194#, 150-70, never smoker, Dx HTN,
Dyslipoproteinemia
Current Meds: Altace 10 MG QD, spironolactone/HCTZ 12.5/12.5 MG QD
Changed to rosuvastatin 10 MG QD and ER niacin 1000 MG QD
TC = 135
LDL-C = 86 (10th)
HDL-C = 63 (75th)
TG = 62
Non HDL-C = 72 (1st)
LDL-P = 953 (10th)
Small LDL-P = 652
LDL Particle Size = 20.9
Large HDL-P = 10.1 (90th)
Large VLDL-P = 0.2
Pattern A = 23.0 - 20.6