PowerPoint - 埼玉医科大学総合医療センター 内分泌・糖尿病内科
advertisement

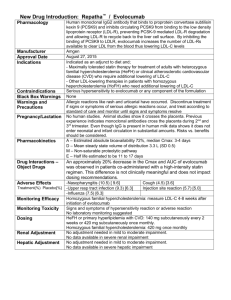
Journal Club Raal FJ, Honarpour N, Blom DJ, Hovingh GK, Xu F, Scott R, Wasserman SM, Stein EA; for the TESLA Investigators. Inhibition of PCSK9 with evolocumab in homozygous familial hypercholesterolaemia (TESLA Part B): a randomised, double-blind, placebo-controlled trial. Lancet. 2014 Oct 1. pii: S0140-6736(14)61374-X. doi: 10.1016/S0140-6736(14)61374-X. Zhao D, Cho J, Kim MH, Friedman DS, Guallar E. Diabetes, Fasting Glucose, and the Risk of Glaucoma: A Meta-analysis. Ophthalmology. 2014 Oct 2. pii: S0161-6420(14)00697-6. doi: 10.1016/j.ophtha.2014.07.051. 2014年10月23日 8:30-8:55 8階 医局 埼玉医科大学 総合医療センター 内分泌・糖尿病内科 Department of Endocrinology and Diabetes, Saitama Medical Center, Saitama Medical University 松田 昌文 Matsuda, Masafumi http://www.pcsk9forum.org/ Treatment of homozygous familial hypercholesterolaemia • • • • • • • • statins ezetimibe partial ileal bypass portacaval shunt liver transplantation LDL apheresis mipomersen lomitapide • (ALN-PCS) • • • alirocumab evolocumab bococizumab PCSK9 target KYNAMROTM (mipomersen sodium) KYNAMROTM is an oligonucleotide inhibitor of apolipoprotein B-100 synthesis Lancet 2010; 375: 998–1006 Lomitapide (INN, marketed as Juxtapid) is a drug for the treatment of familial hypercholesterolemia, developed by Aegerion Pharmaceuticals. It has been tested in clinical trials as single treatment and in combinations with atorvastatin, ezetimibe and fenofibrate. The US Food and Drug Administration (FDA) approved lomitapide on 21 December 2012, as an orphan drug to reduce LDL cholesterol, total cholesterol, apolipoprotein B, and non-high-density lipoprotein (non-HDL) cholesterol in patients with homozygous familial hypercholesterolemia (HoFH). Lomitapide inhibits the microsomal triglyceride transfer protein (MTP or MTTP) which is necessary for very low-density lipoprotein (VLDL) assembly and secretion in the liver. http://en.wikipedia.org/wiki/Lomitapide Proprotein convertase subtilisin/kexin type 9 PCSK9 (neural apoptosis-regulated convertase, NARC-1) is a 692-residue extracellular protein representing the 9th member of the secretory subtilase family expressed primarily in the kidneys, liver and intestines. Genetic studies mapped PCSK9 along with LDLR and APOB to cause autosomal dominant hypercholesterolemia (ADH). Gain-of-function mutations increased plasma levels of low-density lipoprotein cholesterol (LDL-C), whereas nonsense or missense (loss-of-function) mutations, which interfere with folding or secretion of PCSK9, led to a reduction of plasma levels of LDL-C and an 88% decrease in the risk of coronary heart disease (CHD). http://caltagmedsystems.blogspot.jp/2012/04/pcsk9-attractive-drug-target-for.html Lancet. 2014 Jan 4;383(9911):60-8. Alirocumab SAR236553 (REGN727) 抗体治療!! single ascending-dose studies of REGN727 N Engl J Med 2012;366:1108-18. 抗体治療+スタチン Alirocumab SAR236553 (REGN727) primary hypercholesterolemia N Engl J Med 2012;367:1891-900. DOI: 10.1056/NEJMoa1201832 Effect of ALN-PCS treatment on serum LDL cholesterol Lancet. 2014 Jan 4;383(9911):60-8. ALN-PCS:a small interfering RNA that inhibits PCSK9 synthesis Evolocumab (AMG 145) Carbohydrate and Lipid Metabolism Research Unit, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa (Prof F J Raal PhD); Amgen Inc, One Amgen Center Drive, Thousand Oaks, CA, USA (N Honarpour MD, F Xu MS, R Scott MD, S M Wasserman MD); Division of Lipidology, Department of Medicine, University of Cape Town, UCT Faculty Health Sciences, Cape Town, South Africa (D J Blom MD); Vascular Medicine, Academic Medical Centre, Amsterdam, Netherlands (G Kees Hovingh MD); and Metabolic and Atherosclerosis Research Center, Cincinnati, OH, USA (Prof E A Stein PhD) www.thelancet.com Published online October 2, 2014 http://dx.doi.org/10.1016/S0140-6736(14)61374-X Background Homozygous familial hypercholesterolaemia is a rare, serious disorder caused by very low or absent plasma clearance of LDL, substantially raised LDL cholesterol, and accelerated development of cardiovascular disease. Conventional lipid-lowering treatments are modestly effective. Evolocumab, a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 (PCSK9), reduced LDL cholesterol by 16% in a pilot study. We now report results with evolocumab in a randomised, double-blind, placebo-controlled phase 3 trial. Methods This randomised, double-blind, placebo-controlled phase 3 trial was undertaken at 17 sites in ten countries in North America, Europe, the Middle East, and South Africa. 50 eligible patients (aged ≥12 years) with homozygous familial hypercholesterolaemia, on stable lipidregulating therapy for at least 4 weeks, and not receiving lipoprotein apheresis, were randomly allocated by a computer-generated randomisation sequence in a 2:1 ratio to receive subcutaneous evolocumab 420 mg or placebo every 4 weeks for 12 weeks. Randomisation was stratified by LDL cholesterol at screening (<11 mmol/L or ≥11 mmol/L) and implemented by a computerised interactive voice-response system. Patients, study personnel, and the funder were masked to treatment and to the efficacy results by the central laboratory not returning LDL cholesterol or any lipid results to the clinical sites after the baseline visit. The primary endpoint was percentage change in ultracentrifugation LDL cholesterol from baseline at week 12 compared with placebo, analysed by intentionto-treat. This trial is registered with ClinicalTrials.gov, number NCT01588496. Table 1: Baseline characteristics LDL-C 8.7mmol/L=336mg/dL LDL-C 9.2mmol/L=355mg/dL LDL-C 9.0mmol/L=347mg/dL HDL-C 1.0mmol/L=38.6mg/dL TG 1.3mmol/L=115mg/dL 0.0259 for Cholesterol 0.0113 for TG Data are mean (SD), range, n (%), or median (IQR). PCSK9=proprotein convertase subtilisin/kexin type 9.*Ethnicity was self-reported and some patients did not answer this question. Table 2: Efficacy outcomes Data are leastsquares mean (95% CI) except for hsCRP data, which are median (IQR). Least-squares mean is from the repeated measures model, which includes treatment group, stratifi cation factor, scheduled visit, and interaction of treatment with scheduled visits as covariates for all endpoints. PCSK9=proprotei n convertase subtilisin/kexin type 9. hsCRP=highsensitivity Creactive protein. NA=not applicable. *Multiplicity adjustments following the Hochberg procedure were used to control for overall signifi cance at the 0·05 level of signifi cance for the primary and secondary endpoints. Table 4: Adverse events ALT=alanine aminotransferase. AST=aspartate aminotransferase. ULN=upper limit of normal. *Reported in at least one patient in either or both treatment groups. †Searched with use of high-level term grouping, which includes injection-site rash, infl ammation, pruritus, reaction, or urticaria. ‡Searched with use of high-level grouping, which includes deliria (including confusion), cognitive and attention disorders and disturbances, dementia and amnestic disorders, disturbances in thinking and perception, and mental impairment disorders. §Excludes one patient who had a positive binding antibody test at baseline and negative antibody testing at all other study assessments. Findings Of the 50 eligible patients randomly assigned to the two treatment groups, 49 actually received the study drug and completed the study (16 in the placebo group and 33 in the evolocumab group). Compared with placebo, evolocumab significantly reduced ultracentrifugation LDL cholesterol at 12 weeks by 30·9% (95% CI −43·9% to −18·0%; p<0·0001). Treatment-emergent adverse events occurred in ten (63%) of 16 patients in the placebo group and 12 (36%) of 33 in the evolocumab group. No serious clinical or laboratory adverse events occurred, and no anti-evolocumab antibody development was detected during the study. Interpretation In patients with homozygous familial hypercholesterolaemia receiving stable background lipid-lowering treatment and not on apheresis, evolocumab 420 mg administered every 4 weeks was well tolerated and significantly reduced LDL cholesterol compared with placebo. Funding Amgen Inc. Message ホモ接合体家族性高コレステロール血症(FH)患者50人 を対象に、前駆たんぱく質転換酵素サブチリシン/ケキ シン9型(PCSK9)に対するモノクローナル抗体 evolocumabのLDLコレステロール低下効果を第3相試験で 検討(TESLA Part B試験)。12週後、プラセボに比べて evolocumabがLDLコレステロールを30.9%低下させた(P <0.0001)。 大規模臨床治験中(心血管障害リスク者) ODYSSEY (NCT01663402) with alirocumab, FOURIER (NCT01764633) with evolocumab, and SPIRE-1 (NCT01975389) and SPIRE-2 (NCT01975376) with bococizumab, Department of Epidemiology and Welch Center for Prevention, Epidemiology, and Clinical Research, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland. 2 Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Sungkyunkwan University, Seoul, Korea. 3 Biostatistics and Clinical Epidemiology Center, Research Institute for Future Medicine, School of Medicine, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea. 4 Saevit Eye Hospital, Goyang, Gyeonggi-do, Korea. 5 Department of Epidemiology, Graduate School of Public Health, Seoul National University, Seoul, Korea. 6 Wilmer Eye Institute, Johns Hopkins University, Baltimore, Maryland. Topic: We performed a systematic review to summarize the association of diabetes and blood glucose levels with glaucoma, intraocular pressure (IOP), and ocular hypertension in the general population. Clinical Relevance: Diabetes has been proposed as a risk factor for glaucoma, but epidemiologic studies have been inconsistent, and the association is still controversial. Furthermore, no systematic reviews evaluated other metabolic abnormalities, such as the metabolic syndrome, with the risk of glaucoma. Methods: We identified the studies by searching the PubMed and EMBASE databases. We used inversevariance weighted random-effects models to summarize relative risks across studies. http://www.genome.med.kyoto-u.ac.jp/func-gen-redirect/wiki/index.php/Heterogeneity%E3%81%AE%E6%A4%9C%E5%AE%9A Results: We identified 47 studies including 2 981 342 individuals from 16 countries. The quality of evidence generally was higher in the cohort compared with casecontrol or cross-sectional studies. The pooled relative risk for glaucoma comparing patients with diabetes with those without diabetes was 1.48 (95% confidence interval [CI], 1.29-1.71), with significant heterogeneity across studies (I2 = 82.3%; P < 0.001). The risk of glaucoma increased by 5% (95% CI, 1%-9%) for each year since diabetes diagnosis. The pooled average difference in IOP comparing patients with diabetes with those without diabetes was 0.18 mmHg (95% CI, 0.09-0.27; I2 = 73.2%), whereas the pooled average increase in IOP associated with an increase in 10 mg/dl in fasting glucose was 0.09 mmHg (95% CI, 0.05-0.12; I2 = 34.8 %) Conclusions: Diabetes, diabetes duration, and fasting glucose levels were associated with a significantly increased risk of glaucoma, and diabetes and fasting glucose levels were associated with slightly higher IOP. Message PubMedとEMBASEからの既発表論文47件(被験者 約298万人)を対象に、糖尿病(DM)と緑内障リ スクの関連をシステマティックレビューで検 証。非DM患者に対するDM患者のプールされた緑 内障相対リスクは1.48だったが、高い報告間の 異質性が見られた(I2=82.3%)。緑内障リスク はDM診断後1年経過ごとに5%増加した。 緑内障はあまり糖尿病の合併症として考えられ たり管理されていないが...