LDL
advertisement

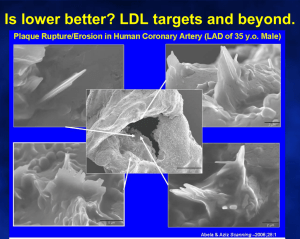
Advances In The Treatment of Hyperlipidemia Hallie Lee PharmD Candidate 2013 Mercer University COPHS December 2012 Objectives Background: Lipoproteins & lipid metabolism Etiologies of lipid disorders NCEP ATP III Guidelines NCEP ATP III 2004 update Treatment Options NCEP ATP IV New Potential Goal Modifiers Plasma Lipids Lipids are transported in the plasma as lipoproteins The major lipid classes present in lipoproteins Triacylglycerols (16%) Phospholipids (30%) Cholesterol (14%) Cholesterol esters (36%) Free fatty acids (4%) Lipoproteins A core of nonpolar cholesteryl esters and triglycerides covered by a polar surface monolayer made up of phospholipids, free cholesterol, and apolipoproteins Lipoprotein components Cholesterol-structural component of all cell membranes and a precursor for steroid biosynthesis and bile acids Present in tissues and in plasma either as free cholesterol or combined with a long-chain fatty acid as cholesteryl ester, the storage form A little more than half comes from the body itself synthesized from acetyl-CoA, the rest comes from the diet Triglyceride-fatty acids used for energy by the liver and peripheral tissues i.e. muscle Phospholipid-component of cell membranes Lipids are water insoluble and require lipoprotein transporters to reach body tissues from the bloodstream Lipoprotein Classes Lipoprotein Density (g/ml) Chylomicrons 0.95 Triglyceride Lipid cholesterol (free/ester) Phospholipid 85-95% 1-3%/2-4% 3-6% VLDL 0.96-1.006 50-60% 4-8%/16-22% 15-20% IDL 1.006-1.019 20-50% 20-40% total 15-25% LDL 1.019-1.063 4-8% 6-8%/45-50% 18-24% HDL 1.063-1.210 2-7% 3-5%/15-20% 26-32% VLDL-very low density lipoprotein IDL-intermediate density lipoprotein LDL-low density lipoprotein HDL-high density lipoprotein Apolipoproteins make up the rest Apoplipoproteins Apolipoproteins carry out several roles: 1. They form part of the structure of the lipoprotein 2. They are enzymes, cofactors, or inhibitors 3. They act as ligands for interaction with lipoprotein receptors in tissues “Nametags” attached as identifiers Apolipoprotein Lipoprotein Function Site of Synthesis Apo A-1 HDL, chylomicrons Structural protein on HDL, activator of LCAT Liver, intestine Apo A-II HDL, chylomicrons Structural protein on HDL Liver Apo A-IV HDL, chylomicrons, VLDL Unknown, possibly facilitates transfer of apos Intestine Apo B-48 Chylomicrons Synthesis/secretion of chylomicrons form the SI Intestine Apo B-100 LDL, VLDL Synthesis/secretion of VLDL from liver, ligand for binding to LDL receptor Liver Apo C-I HDL, chylomicrons, VLDL Activator of Lecithin cholesterol acyltransferase Liver Apo C-II HDL, chylomicrons, VLDL Activator of Lipoprotein lipase Liver Apo C-III HDL, chylomicrons, VLDL May inhibit hepatic uptake of chylomicron and VLDL Liver Apo E HDL, chylomicrons, VLDL Binds to LDL receptor on membrane of liver and macrophage cells Liver Lipid Metabolism Exogenous Endogenous Reverse Transport Lipid Metabolism Exogenous pathway = transport of dietary lipids 1. Lipids from diet absorbed into intestinal villa as fatty acids and cholesterol 2. Re-esterification of fatty acids TG & cholesterol cholesteryl ester occurs in mucosal cells 3. TG and cholsteryl ester combined with Apo B-48 and Apo A-I within intestinal wall to form immature chylomicron particles 4. Chylomircons enter the systemic circulation via the lymphatic system 5. Apo C-II and Apo E transferred to chylomicrons from HDL particles in the bloodstream 6. Apo C-II enhances interactions of chylomicron and lipoprotein lipase on the capillary endothelial cell surfaces in tissues, TG hydrolyzed into free fatty acids for storage or energy use by muscle 7. Remnants are cleared by receptors on surface of liver cells that recognize Apo E Exogenous Pathway Lipid Metabolism Endogenous pathway = transport of lipids produced by the body 1. VLDL assembled and secreted by hepatocytes: TG and cholesterol are packaged with Apo B-100 and phospholipids, Apo C-II and Apo E added after VLDL enters the plasma 2. TG core hydrolyzed by lipoprotein lipase in capillary beds releasing fatty acids into tissues 3. Remaining VLDL is now IDL, most surface apos (minus Apo B100) are transferred to HDL, mediated by cholesteryl ester transfer protein (CETP) 4. IDL removed from liver by Apo E binding to LDL receptor, remaining IDL is converted to LDL via hepatic lipase Endogenous Pathway Lipid Metabolism Reverse cholesterol transport 1. Apo A-I is produced in the liver and intestine, acts as the building block for nascent(immature) HDL 2. Nascent HDL particles act as initial acceptors of free cholesterol from peripheral cells through the receptor ATP binding cassette AI 3. Lecithin cholesterol acetyl transferase (LCAT) converts free cholesterol to cholesteryl ester to form the core of HDL3, LCAT is activated by Apo A-I 4. Enrichment of HDL3 with cholesteryl ester results in formation of HDL2 5. Cholesteryl ester may be transferred from HDL to VLDL, IDL, or LDL (Apo B lipoproteins) in exchange for triglyceride molecules by cholesterol ester transfer protein (CEPT) 6. Cholesteryl ester may be delivered directly to the liver by HDL itself Reverse Cholesterol Transport Etiology Primary hyperlipoproteinemia: lipoprotein abnormalities direct result of specific defects in synthesis/degradation of particles 1. Familial hypercholesterolemia Defective gene for LDL receptor Characterized by sever elevations of LDL, tendon xanthomas, and premature atherosclerosis 2. Polygenic hypercholesterolemia variety of genetic defects resulting in less active LDL receptor Possibly the underlying disorder in as many as 80% of people with hypercholesterolemia Elevated LDL and premature atherosclerosis 3. Familial combined hyperlipidemia Associated with overproduction of VLDL due to increased production of Apo B-100 Elevated LDL and/or TG and premature atherosclerosis Etiology Secondary hyperlipoproteinemia: elevated lipoprotein levels occur as part of an underlying disorder or drug therapy 1. Hypercholesterolemia 2. 3. Hypothyroidism, liver disease, nephrotic syndrome Meds: progestins, thiazides, glucocorticoids, BB, cyclosporine, mirtazepine Hypertriglyceridemia Obesity, DM, Pregnancy, acute hepatitis Meds: alcohol, estrogens, isotretinoin, BB, glucocorticoids, azole antifungals Low HDL Malnutrition, obesity Meds: anabolic steroids, isotretinoin, progestins Disease Terminology Hyperlipoproteinemia - high lipoproteins Hypercholesterolemia -high TC or LDL Hyperlipidemia -high TC, TG, or LDL Hypertriglyceridemia -high TG Dyslipidemia -high TC, TG, LDL or low HDL TC-total cholesterol TG-triglycerides National Cholesterol Education Program Adult Treatment Panel III “NCEP ATP III Guidelines” Current Treatment Guidelines NCEP ATP III Focus All adults ≥ 20 years old should have a fasting lipid panel performed every 5 years A complete lipoprotein profile is preferred Fasting TC, LDL, HDL, and TG Secondary option Non-fasting TC and HDL Proceed to lipoprotein profile if TC ≥ 200 or HDL < 40 LDL is the primary target If TG are > 500mg/dL, TG should be targeted first Once LDL goal is achieved, attention should be focused on the other parameters (non HDL cholesterol) Non HDL-C = Total cholesterol - HDL cholesterol 3 Categories of Risk that Modify LDL Goals* Risk Category LDL Goal (mg/dL) CHD and CHD risk equivalents <100 Multiple (2+) risk factors <130 Zero to one risk factor <160 *Per the 2001 NCEP ATP III Guidelines Risk Factors Positive Risk Factors Age : M ≥ 45 F ≥ 55 Family history : premature CHD in 1st degree relative M <55 F <65 Current smoker HTN >140/90 or on medication Low HDL <40 Negative Risk Factors High HDL ≥ 60 Risk Assessment All patients without CHD or CHD risk equivalents: Count the number of risk factors If multiple risk factors ≥ 2 use Framingham scoring to determine 10 year CHD risk For patient with 0-1 risk factors 10 year risk assessment not required Managing lipids for risk reduction: Focus on the new National Cholesterol Education Program guidelines. Vascular Biology Working Group. University of Flordia 2001. Available at http://www.vbwg.org/quickorder/resource_slides.cfm?itemID=6&TypeID=4&StartRow=6#mark. Accessed December 9, 2012. Managing lipids for risk reduction: Focus on the new National Cholesterol Education Program guidelines. Vascular Biology Working Group. University of Flordia 2001. Available at http://www.vbwg.org/quickorder/resource_slides.cfm?itemID=6&TypeID=4&StartRow=6#mark. Accessed December 9, 2012. CHD and CHD Risk Equivalents Established CHD MI Risk Equivalents CAD Myocardial ischemia Stroke Coronary angioplasty/stent placement TIA Carotid stenosis >50% CABG PAD Prior unstable angina Abdominal aortic aneurysm Diabetes LDL goal is < 100mg/dL for these patients per the 2001 Guidelines Goals LDL Total Cholesterol Optimal < 100 Desirable < 200 Near Optimal 100-129 Borderline 200239 Borderline 130159 High ≥ 240 High 160-189 Very high ≥ 190 Goals Triglycerides HDL Normal < 150 Low < 40 Borderline 150199 High > 60 High 200-499 Very high >500 Calculating LDL LDL = TC – HDL – ( TG/5 ) LDL equals total cholesterol minus HDL minus triglycerides divided by five TG must be <400 to use VLDL = TG/5 Example: TC=225 HDL=32 TG=170 LDL = 225-32-(170/5) = 159 LDL-Lowering Therapies In Patients With CHD and CHD Risk Equivalents Baseline LDL cholesterol ≥ 130 mg/dL Intensive lifestyle therapies Maximal control of other risk factors Consider starting LDL-lowering drugs simultaneously with lifestyle therapies Baseline (or on treatment) LDL 100-129mg/dL LDL lowering therapy; lifestyle therapy or drugs Treatment of metabolic syndrome Weight reduction and increased physical activity Drug therapy for other lipid risk factors LDL-Lowering Therapies In Patients With CHD and CHD Risk Equivalents Baseline LDL < 100mg/dL Further LDL lowering not required Therapeutic Lifestyle Changes (TLC) recommended Consider treatment of other lipid risk factors Ongoing clinical trials are assessing benefit of further LDL lowering LDL-lowering Therapy in Patients With Multiple Risk Factors and 10 Year Risk ≤ 20% 10 Year Risk 10-20% LDL-lowering goal <130mg/dL Aim to reduce short and long term risk Immediate initiation of TLC if LDL goes >130 Consider drug therapy if LDL > 130 after 3 months of lifestyle therapies 10 Year Risk < 10% LDL goal <130mg/dL Aim to reduce long term risk Initiate therapeutic lifestyle changes if LDL > 130 Consider drug therapy if LDL > 160 after 3 months of lifestyle therapies LDL-Lowering in Patients with 0-1 Risk Factor Aim to reduce long term risk LDL goal <160 Initiate therapeutic lifestyle changes is LDL > 160 If LDL is ≥ 190 after 3 months of lifestyle therapies consider drug therapy If LDL is ≥ 160-189 after 3 months of lifestyle therapies drug therapy is optional Summary Treatment Categories Risk Category CHD or CHD risk equivalent 2 Risk Factors 10-yr risk 10–20% 10-yr risk <10% <2 Risk Factors LDL-C Goal Consider Drug Therapy <100 mg/dL 130 mg/dL* <130 mg/dL <130 mg/dL 130 mg/dL 160 mg/dL <160 mg/dL 190 mg/dL * 100–129 mg/dL = after TLC, consider statin, niacin, or fibrate therapy Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001;285:2486-2497. NCEP ATP III 2004 Update For high risk patients: LDL-Lowering Therapies In Patients With CHD and CHD Risk Equivalents LDL goal < 70 in patients with established CHD plus: Multiple risk factors, esp. diabetes Severe or poorly controlled risk factors Metabolic syndrome Acute coronary syndromes Consideration of drug treatment in addition to lifestyle therapy for LDL levels ≥100 mg/dL in high-risk patients, and characterizes drug treatment as optional for LDL<100 mg/dL NCEP ATP III 2004 Update For moderately high-risk patients--Individuals who have multiple (2+) CHD risk factors together with a 10-20% risk for a heart attack within 10 years: The overall goal for moderately high-risk patients is still an LDL < 130 mg/dL There is a therapeutic option to set the treatment goal at LDL <100 mg/dL and to use drug treatment if LDL is 100-129 mg/dL For high-risk and moderately high-risk patients: Advises that the intensity of LDL-lowering drug treatment in highrisk and moderately high-risk patients be sufficient to achieve at least a 30 percent reduction in LDL levels Goals for Therapy: The 2004 Addendum NCEP ATP III guidelines for LDL Therapy LDL-C <160 for 1 or less risk factors LDL-C <130 for 2+ risk factors < 100 is a therapeutic option LDL-C <100 for CAD and CAD equivalents <70 is option for very high risk patients 1. 2. 3. 4. 5. CAD + multiple risk factors, especially diabetes CAD + severe or poorly controlled risk factor(s) CAD + metabolic syndrome Acute coronary syndrome CAD event despite baseline LDL-C < 100 LDL Therapy Lifestyle Changes Statins Bile Acid Sequestrants Ezetimibe Niacin Plant Stanols, Sterols, Phytosterols Therapeutic Lifestyle Changes (TLC) TLC Diet Reduced intake of cholesterol-raising nutrients Saturated fats <7% of total calories Dietary cholesterol <200mg per day LDL-lowering therapeutic options Plant stanols/sterols Soluble fiber 10-25gram per day Weight reduction Increased physical activity Smoking cessation ATP III Guidelines Slide Show. National Heart Lung, and Blood Institute.. Available at http://hp2010.nhlbihin.net/ncep_slds/atpiii/slide31.htm. Accessed December 9, 2012. ATP III Guidelines At a Glance Quick Desk Reference. National Cholesterol Education Program. National Institutes of Health. Available at http://www.nhlbi.nih.gov/guidelines/cholesterol/atglance.pdf. Accessed on December 9, 2012. NCEP ATP IV When will it be available? Draft Completed: Expert panelists have completed a full draft of the systematic review and recommendations. Federal Review Completed: Federal agency representatives of the NHLBI's National Program to Reduce Cardiovascular Risk (NPRCR) coordinating committee provide review and comment. Expert Review Completed: External peer reviewers with expertise in the relevant risk factors provide review and comment. Advisory Council In Progress: The National Heart, Lung, and Blood Advisory Council provides review and comment and recommends approval. Public Comment: The draft will eventually be offered publicly for review and comment. HHS Clearance: The U.S. Department of Health and Human Services provides editorial review, comment, and approval once it is made available. Issues for ATP-IV 1. Should the goals for LDL in primary prevention be lowered? 2. Where does CRP fit in– routine use in risk stratification, secondary target? 3. What about Apo-B? 4. What about secondary targets? 5. Non-HDL-C, HDL-C, LDL Particle concentration? Move from a 10-year to lifetime risk? Potential Goal Modifiers Lp(a)/Apo A Apo AI High sensitivity CRP Lp-PLA2 Metabolic Syndrome Apo B LDL-P vs. LDL-C Apo E and lipoprotein Genetics Definitions LDL-C: amount of cholesterol in LDL particles LDL-P: number of LDL particles Non-HDL: amount of cholesterol in atherogenic particles Apo-B: number of atherogenic particles Lp(a) / Apo a Physiological function is still unknown High level in the blood is a risk factor for CHD, CVD, atherosclerosis, thrombosis, and stroke Desirable: Most LDL-lowering drugs do not effect the blood levels Borderline risk: Apo(a) contains domains that are very similar to plasminogen (PLG) Lp(a) accumulates in the vessel wall and inhibits binding of PLG to the cell surface, reducing plasmin generation which increases clotting Suggests it can cause the generation of clots and atherosclerosis Lp(a) Levels: < 14 mg/dL (< 35 nmol/l) 14 - 30 mg/dL (35 - 75 nmol/l) High risk: 31 - 50 mg/dL (75 - 125 nmol/l) Very high risk: > 50 mg/dL (> 125 nmol/l) Apo AI The American Association of Clinical Endocrinologists (AACE) Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis States: The assessment of Apo AI may be useful in certain cases A normal Apo AI level in a patient with low HDL-C suggests the existence of an adequate number of HDL-C particles that contain less cholesterol and may be an indication of less risk The INTERHEART study found that the Apo B to Apo AI ratio was among the most significant risk factors for MI C-Reactive Protein Produced by the liver Level rises when there is inflammation throughout the body High-sensitivity C-reactive protein (hs-CRP) assay tests are available Determine a person's risk for heart disease Many consider a high CRP level to be a risk factor for heart disease It is not known whether it is merely a sign of cardiovascular disease or if it actually plays a role in causing heart problems According to the American Heart Association: You are at low risk of developing You are at average risk of developing cardiovascular disease if your levels are between 1.0 - 3.0 mg/L You are at high risk for cardiovascular disease if your hs-CRP level is > 3.0 mg/L cardiovascular disease if your hs-CRP level is < 1.0mg/L AACE recommends CRP testing to stratify CVD risk in patients with a standard risk assessment that is borderline, or in those with an LDL-C con- centration < 130 mg/dL Lp-PLA2 A blood enzyme that hydrolyzes oxidized phospholipids, causing atherogenic vascular inflammation Accumulation of macrophages and lymphocytes in atherosclerotic inflammation is accompanied by increased expression of Lp-PLA2 in plaques According to the AACE: There are studies that have demonstrated Lp-PLA2 showing more specificity than highly sensitive CRP, when it is necessary to further stratify a patient’s CVD risk, especially in the presence of systemic highly sensitive CRP elevations Lp-PLA2 : <200ng/mL is normal ≥ 200 and <233 ng/mL is intermediate ≥ 223 ng/mL is high Synergistic with CRP However, CRP is marker of general inflammation and Lp-PLA2 appears to specifically indicate vascular inflammation and not be influenced by obesity Apo B Smaller denser LDL particle A MEDLINE search of the literature published from January 1, 1975, - December 1, 2010 : “Opening a New Lipid ‘Apo-thecary’: Incorporating Apolipoproteins as Potential Risk Factors and Treatment Targets to Reduce Cardiovascular Risk” (Jacobson, T.) “On the basis of data from most population studies, elevated Apo B was more strongly associated with incident coronary heart disease than similarly elevated LDL cholesterol” “Apo B was also a superior benchmark (vs LDL cholesterol) of statins' cardioprotective efficacy” Apo B continued Potentially has a greater propensity to cause oxidative arterial wall damage If a patient has increased levels of Apo B the total number of LDL particles may be higher than the LDL cholesterol level A 1:1 relationship between LDL particles and the total number of atherogenic particles The controversy remains Apo-B Goals A look at the Clinical Trials Trial Apo-B Major Statin Trials 67-98 PROVE-IT 67 JUPITER 71 Fredrickson, S. LDL-C, Apo-B, LDL-P, and The Winner Is Slideshow. March 2012. Available at http://www.acponline.org/about_acp/chapters/va/12mtg/fredrickson.pdf. Accessed December 10, 2012. Apo B Goals AACE recommends: For patients at risk of CAD (including those with diabetes) goal of < 90 mg/dL For patients with established CAD or diabetes who have 1 or more additional risk factor(s) should goal of < 80 mg/dL When the triglyceride level is >150 mg/dL or the HDL-C level is < 40 mg/dL, the Apo B or the Apo B/Apo AI ratio may be particularly useful in assessing residual risk in patients at risk for CAD Apo B measurements to assess the success of LDL-C–lowering therapy Apo B reflects the LDL particle number, which may be elevated in patients at or below LDL-C goal and a more potent predictor of CV disease risk LDL-C vs LDL-P LDL-C is calculated using Friedewalde equation Inaccurate when: TG high Glucose high LDL-C very low LDL-C can underestimate LDL particle number (LDL-P), particularly in patients with insulin resistance CVD risk is more closely associated with number of LDL particles rather than amount of cholesterol carried by LDL particles LDL-C underestimates LDL particle number when cholesterol depleted LDL is present The AACE states LDL particle number is a more potent measure of CVD risk than LDL-C or LDL particle size Cardiovascular Risk is more strongly associated with LDL-P than LDL-C Source: Journal of Clinical Lipidology 2011; 5:338-367 (DOI:10.1016/j.jacl.2011.07.005 ) Metabolic Syndrome A name for a group of risk factors that occur together and increase the risk for CAD, Stroke, and Type II Diabetes The two most important risk factors: Central Obesity-Extra weight around the middle and upper parts of the body Insulin resistance-the the body uses insulin less effectively than normal Diagnosis: three or more of the following signs: Blood pressure ≥ 130/85 mmHg Fasting blood sugar (glucose) ≥ 100 mg/dL Large waist circumference : Men – ≥ 40 inches Women - ≥ 35 inches Low HDL cholesterol: Men - < 40 mg/dL Women - < 50 mg/dL Triglycerides equal to or higher than 150 mg/dL American Association of Clinical Chemistry Contois JH, et al. Clinical Chemistry 2009; 55:407-419 Recommendations from AACC Lipoproteins and Vascular Diseases Division Working Group on Best Practices ► “LDL-C, non-HDL-C, LDL-P, and total apoB are all, to varying degrees, measures of LDL related risk.” ► “These cholesterol and particle measures are highly intercorrelated, which explains why they have all been implicated as predictors of CVD risk in epidemiologic studies, but biologically they reflect different entities.” ► “Despite a high correlation, these markers are only modestly concordant, indicating that one cannot simply substitute for another in classifying patients into risk categories.” ► “We believe that the medical decision cutpoints should be set so that the apoB and LDL-P cutpoints are equivalent to those for LDL-C in terms of population percentiles.” Contois JH, et al. Clinical Chemistry 2009; 55:407-419 Recommendations from AACC Lipoproteins and Vascular Diseases Division Working Group on Best Practices Suggested Treatment Goals LDL-C, mg/Non-HDL-C, ApoB, mg/dL mg/dL dL < 70 < 80 < 100 < 80 < 120 < 100 < 130 < 150 LDL-P, nmol/ L < 1100 < 1400 Contois JH, et al. Clinical Chemistry 2009; 55:407-419 Recommendations from AACC Lipoproteins and Vascular Diseases Division Working Group on Best Practices Use of ApoB and LDL Particle Number in Clinical Management agree that a greater emphasis on non–HDL-C rather than LDL-C will improve patient care. Data from several prospective studies show non–HDL-C to be a better predictor of cardiovascular events than LDL-C. ►We ►In terms of relative risk, non–HDL-C is consistently stronger than LDL-C and, in many studies, equivalent to apoB or LDL-P. ►However, apoB has been more extensively validated in epidemiological studies and clinical trials than non–HDL-C, and non–HDL-C, like LDL-C, reflects the cholesterol content of atherogenic particles and not the number of atherogenic particles. on-treatment non–HDL-C concentrations may not reflect residual risk associated with increased LDL particle number ►Importantly, Contois JH, et al. Clinical Chemistry 2009; 55:407-419 Apo E and Lipoprotein Genetics According to a meta-analysis reviewing the associations of apolipoprotein E genotype and coronary disease: A linear relationships of apo E genotypes with both LDL-C levels and coronary risk exists Compared with individuals with the ε3/ε3 genotype, ε2 carriers have a 20% lower risk of coronary heart disease and ε4 carriers have a slightly higher risk What do the Advancements in the Treatment of Hyperlipidemia mean for the future ? How Should the Guidelines Change? Citations Wasan, K. et al. Impact of Lipoproteins on the biological activity and disposition of hydrophobic drugs: implications for drug discovery. Nat Rev Drug Discov. 2008 Jan;(7):84-99. Kishor M. Wasan, Dion R. Brocks, Stephen D. Lee, Kristina Sachs-Barrable & Sheila J. Thornton. Nature Reviews Drug Discovery 7, 84-99. Talbert RL. Chapter 28. Dyslipidemia. In: Talbert RL, DiPiro JT, Matzke GR, Posey LM, Wells BG, Yee GC, eds. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York: McGrawHill; 2011. http://www.accesspharmacy.com/content.aspx?aID=7974214. Accessed December 8, 2012. Botham KM, Mayes PA. Chapter 25. Lipid Transport & Storage. In: Murray RK, Kennelly PJ, Rodwell VW, Botham KM, Bender DA, Weil PA, eds. Harper's Illustrated Biochemistry. 29th ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=55883242. Accessed December 9, 2012. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001;285:2486-2497. Thomas, A. Lipid Management Standard and Advanced Preview of ATP-IV. Mayo Clinic. 2012. Available at: www.cardiologia.spc.org.py/wp.../Lipid-Talk-Paraguay-final.ppt. Accessed December 9, 2012. Citations Metabolic Syndrome. PubMed Health. US National Library of Medicine. 2012. Available at http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004546/. Accessed December 9,2012. Jacobson, T. Opening a New Lipid “Apo-thecary”: Incorporating Apohpoprotezns as Potential Risk Factors and Treatment Targets to Reduce Cardiovascular Risk. Mayo Clinic Proceedings; Aug 2011. (86):762-780. Fredrickson, S. LDL-C, Apo-B, LDL-P, and The Winner Is Slideshow. March 2012. Available at http://www.acponline.org/about_acp/chapters/va/12mtg/fredrickson.pdf. Accessed December 10, 2012. C-reactive Protein. Medline Plus. US National Library of Medicine. December 2012. Available at http://www.nlm.nih.gov/medlineplus/ency/article/003356.htm. Accessed December 9,2012. Bennet, A. et al. Association of Apolipoprotein E Genotypes With Lipid levels and Coronary Risk. JAMA. 2007;298(11):1300-1311. Jelliger, P. American Association of Clinical Endocrinologists’ Lipid and Atherosclerosis Guidelines. Endocr. Pract. 2012;18(Suppl 1). Available at https://www.aace.com/files/lipid-guidelines.pdf. Accessed December 9, 2012.