Visual field evaluation
advertisement

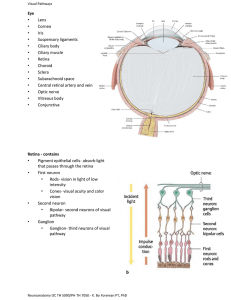
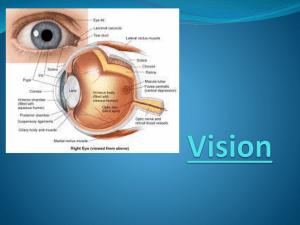
Visual field evaluation ESCRS Dr Fiona Rowe University of Liverpool Goals • Visual pathway anatomy • Methods of perimetry use for Humphrey visual field analyser, Goldmann perimeter, Octopus 900 perimeter • Visual field printout options • Interpretation of results using statistical packages provided by the perimeter systems • Discussion of the ocular symptoms and signs associated with lesions along the various parts of the visual pathway • Possible localisation of lesion according to type of visual field defect plotted • Artefacts of visual field defects and their avoidance. Visual pathway and topography • • • • • • • • Retina Optic disc Optic nerve Optic chiasm Optic tract Lateral geniculate body Optic radiations Visual cortex Retina • • • • • Papillomacular bundle – fovea Nasal retina Superior retina Inferior retina Temporal retina • Central fibres develop first Optic disc • Representation of retinal nerve fibres Optic nerve • Fibres become myelinated • Representation of retinal nerve fibres Optic chiasm • 13mm wide • Surrounded by pituitary gland, third ventricle, thalamus, cavernous sinus • Crossing of nasal retinal fibres • Superior (above), inferior (below), macular (central) Optic tract • Sweep laterally from chiasm around hypothalamus and ventral portion of midbrain • Regroup of fibres – inexact pairing • Ipsilateral temporal and contralateral nasal retinal fibres • Superior (superomedially), inferior (inferolaterally) Lateral Geniculate Body • Diencephalon, midbrain • First synapse of retinal nerve fibres • Rotate through 90 degrees • Superior (medial), inferior (lateral) • 6 layers • Macular fibres in all 6 layers • Ipsilateral temporal fibres; 2, 3, 5 • Contralateral nasal fibres; 1, 4, 6 Optic radiations • • • 90 degree realignment of nerve fibres Superior (above), inferior (below) 3 groups – Upper and central pass directly to visual cortex via posterior temporal and parietal lobes – Lower loops anteriorly and laterally around inferior horn of lateral ventricle (Meyer’s loop) via temporal lobe to visual cortex Visual Cortex • Termination of visual nerve fibres – synapse • Occipital lobe – calcarine fissure • Fovea; tip of occipital pole (posterior) • Temporal crescent; most anterior • Superior (above), inferior (below) Humphrey Analysis • Threshold or suprathreshold analysis – Off-centred equal spacing of central stimuli – Disease specific peripheral presentations Octopus Analysis • Physiology related test pattern – Higher density of stimuli in central field – Follow nerve fibre bundle layer patterns Analysis • • • • • • • • Values Comparison Probabilities Defect (Bebie) curve Diffuse defect Global indices Cluster Graph Polar Graph • Global Trend • Cluster Trend • PolarTrend • • • • • • • • Absolute thresholds Scales and defect depth Percentile of normality Ranking of defect values Deviation from 50th % Mean sensitivity and defect Analysis of regional deviations from normal All local defects mapped to a representation of the optic disc for structure/function comparison • Change rate, fluctuation and significance calculation • Regional change rate and significance calculation • Pointwise linear regression analysis mapped to the optic disc Structure versus Function • Correlation between structural changes (imaging of retinal nerve fibre layer) and functional changes (visual field result) • Structural changes at the optic nerve head and/or retinal nerve fibre layer tend to precede visual field changes early in the disease Polar analysis • Topographic map correlating areas of the visual field (A) with areas of the optic disc (B). Function specific perimetry • Standard achromatic perimetry (white on white) detectable only when a substantial number of ganglion cells lost (≈ 30%) • Functional evaluation of retinal ganglion cells for early detection of glaucoma • Temporally modulated stimuli are more sensitive than WW perimetry • Functional tests isolate subpopulations of retinal ganglion cells which lose function earlier than other ganglion cell types • ≈80% parvocellular ganglion cells – Sensitive to colour and contrast – High pass resolution perimetry • ≈ 15% magnocellular ganglion cells – Sensitive to temporally modulated stimuli – Critical fusion frequency – Frequency doubling technology • ≈ 5% koniocellular ganglion cells – Sensitive to blue-yellow components – B-Y perimetry Function specific perimetry • HRP: High-pass resolution perimetry • Ring shaped targets of 14 different sizes used to determine resolution of central 30 degrees of visual field Function specific perimetry • CFF: Critical fusion frequency perimetry • Measurement of flickering stimulus at different locations ranging from slow to fast (0-50Hz) speed until the stimulus appears to be a continuous light rather than flickering • Not sensitive to lens changes, e.g. cataract • FDT: Frequency doubling technology • Detects the sensitivity for discriminating the frequency doubling stimulus • Stimulus is a large 10 x 10 square of black and white bars, flickering at 25 Hz Function specific perimetry • SWAP: Short-wavelength automated perimetry • Isolates blue sensitivity (S cones) from green (M) and red (L) cones by suppressing the relative sensitivity of M and L cones with a bright yellow background and using a blue stimulus • S- cones become more sensitive • Practical restrictions: – – – – – Cataract Increased variability of threshold Tiring and difficult test – reliability issues Long test duration Considerable learning curve Factors influencing visual fields; Artefacts • • • • • • • • Anatomical features of the face Ptosis Miotic pupil Uncorrected refractive error Refractive corrections Cataract Attention of the patient Technique of the examiner Aids to interpretation Knowledge of visual pathway and: • Related visual field defects • Related signs • Related symptoms Retina and optic disc • • • • • Reduced visual acuity Afferent pupillary defect Reduced colour vision Reduced contrast sensitivity Perceptual problems Optic nerve • • • • Reduced visual acuity Afferent pupillary defect Reduced colour vision Reduced contrast sensitivity Optic chiasm • • • • Postfixational blindness Hemifield slide See saw nystagmus Bowtie atrophy Optic tract • Afferent pupillary defect • Optic atrophy; asymmetrical Optic radiations • Temporal lobe lesion – central achromatopsia, agnosia, alexia, hallucinations, seizures, Bell’s reflex – normal depth and motion • Parietal lobe lesion – reduced stereopsis, spatial localisation and motion, agnosia, reduced OKN, poor fixation, left/right confusion, Bell’s reflex, hemiparesis – normal colour and form, discrimination and recognition of faces Visual cortex • 90% without other neurological signs • Reading difficulties • Cortical blindness – Riddoch phenomenon – Anton’s syndrome Differential diagnosis • Horizontal meridian respected in retinal and optic nerve head lesions • Vertical meridian respected in chiasmal and post chiasmal lesions • Bilateral defects in post chiasmal lesions • Deterioration of vision, RAPD, fundus abnormalities seen in pre chiasm lesions • Case history Perimeter comparison Surface luminance (apostilb:asb) Stimulus luminance •Luminance adjusted by combination of neutral-density filters •Graded in decibels (dB). Each dB equivalent to 0.1 log unit •10dB equals 1 log unit or 10-fold change in intensity Stimulus luminance •Goldmann and Octopus perimeters generate a maximum stimulus luminance (0 dB) of 1,000 asb •Humphrey perimeter uses a 10,000-asb bulb (0 dB) •Range of stimulus intensity greater for Humphrey Perimeter comparison Surface background luminance •Goldmann and Humphrey instruments use 31.5 asb, while past Octopus models use 4 asb •Octopus 900 use 31.4 asb Stimulus duration •100ms for Octopus •200ms for Humphrey Programme strategies •Humphrey perimetry: SITA analysis and threshold standard or fast bracketing strategies •Octopus perimetry: Peritrend analysis and threshold dynamic or TOP strategies Choice of Perimeter Goldmann Octopus Humphrey Manual Kinetic Peripheral Blind spot Poor VA / fixation Advanced defects Driving Manual Automated Kinetic Static Peripheral Central Sensitive to early loss Repeatability Blind spot Poor VA / fixation Advanced defects Driving Automated Static Central Sensitive to early loss Repeatability Driving Common choices • First visit – Screen – Screen: glaucoma – Pathology • Follow-up • • • • Constricted field Hydroxychlorequine Peripheral pathology DVLA 24-2 SITA fast, G TOP 24-2SITA standard, G dynamic 24-2 SITA standard, G dynamic 24-2/30-2 standard, G dynamic 10-2, LV Macula, M dynamic 60-4, Kinetic Estermann Over to you! Summary • Visual pathway anatomy • Visual field results for kinetic and static perimetry • Artefacts of visual fields • Aids to interpretation and localisation of lesion rowef@liv.ac.uk