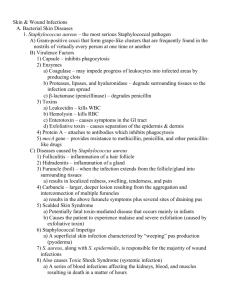
Bacterial skin infections
advertisement

Bacterial & Fungal skin, Soft Tissue & Muscle infections For Second Year Medical Students Prof. Dr Asem Shehabi Infections of Skin & Soft Tissues Infections depends upon the Layers of Skin & Soft Tissues involved ( epidermis, dermis, subcutis, muscle).. Infections may involve one or several skin layers. Skin Infections are associated with: swelling ,tenderness, warm skin, blisters, ulceration, fever headache.. Rarely systemic disease..septicemia. Few Normal Bacteria & Yeast species live in hair follicles- Skin .. may cause inflammation of Hair follicles .. folliculitis, Abscess formation ( Boils).. Type of Skin Infection-1 Skin infection increased by presence of minor skin injuries, abrasions.. Increase production Androgenic Hormones after Puberty.. Increase activities Sebaceous ducts.. secretion Sebum (Fatty Acid+ Peptides) Increase keratin & skin desquamation . Acne vulgaris is the most common skin disorder that affects more Jung male adults than females..Mostly face.. less other body parts due to accumulation of oil sebaceous glands & dead tissues. Causative Agent: Anaerobic Propionibacteria acnes , gram+ve small bacilli excrete Enzymes.. split sebum .. cause mild to severe forms inflammation. Pityrosporum folliculitis is a condition where the yeast invades hair follicles and causes an itchy, Acne-like eruption caused by P.acne Common Normal Skin Flora & Pathogens Staphylococci, hemolytic Streptococci ( Group A) Micrococci, Propionibacteria , Acinetobacter Pityrosporum and other Yeasts..Candida species. S. aureus : coagulase+ve.. Various Enterotoxins & enzymes( Coagulase, DNAse, hyaluronidase), skin infections is the most common & important cause of human Skin diseases. About 15-40 per cent of healthy humans are healthy carriers of S. aureus ..nose or skin..feces. S.epidermidis is also common in skin..less virulent.. No toxins ..opportunistic pathogen.. Clinical features commonly staphylococci: Folliculitis / Furuncles .. Hair follicular-based papules and pustules.. Erythematous lesions.. affect All ages. Skin Infections Staphylococci skin infections S. epidermidis.. normal inhabitants of the skin surface.. but Less Pathogenic. Most its infections occur in normal individuals.. Dry Skin.. Injury.. but underlying illness increase the risk of infection.. Infants.. compromised patients. S.aureus is more associated with serious skin infection due to release of 2 important toxins..not all strains 1-Toxic Schlock Syndrome: TSST-1(Enterotoxin) Super antigens activate T-lymphocytes..Cytokines, caused by localized-systemic infection.. Rash & Skin Desquamation may be associated with sepsis, high fever, multi-organ failure.. kidney failure.. can be fatal. 2-Scalded Skin Syndrome: Epidermolytic/ Exfoliative Toxins (A,B).. Minor skin lesion.. Destruction skin intercellular connection.. Large blisters containing Fluid .. Skin scaling.. Painful.. Common in small children.. Develop specific antitoxins..general massive inflammatory response.. rarely causes kidney failure ..Shock.. Death without antibiotic treatment . Staphylococci are becoming increasingly resistant to many commonly used antibiotics including: Penicillins-Cephalospoins.. Methicillin & flucloxacillin , Augmentin (amoxycillin + clavulonic acid) .. Blactamase-resistant penicillins.. Other antibiotics Worldwide Spread Methicillin resistance (MRSA).. 20-90% ..in Jordan about 60% clinical isolates (2004) Diagnosis &Treatment of staphylococcal infections Lab Diagnosis of staphylococcal infections should be confirmed by: culture, gram-stain, positive cocci, +ve catalase , coagulase test . Effective treatment For MRSA .. Vancomycin, Teicoplanin, Imipenem, Fusidic acid Drainage of pus collections before treatment Surgical removal (debridement) of dead tissue (necrosis) Removal of foreign bodies (stitches) that may be a focus of persisting infection Treating underlying skin disease..Prevent repeat infection..No Vaccine available Streptococcal Skin Infections-1 Streptococcus pyogenes / B-H-Group A) ..Major virulence factors: M-Protein, Hemolysin O & S, Streptokinase (Fibrinolysin-digest Fibrin & Proteins in Plasma), Streptodornase (DNAse) Erythrogenicpyogenic exotoxins,Toxic Shock Syndrome toxin Cellulites/ Erysipelas : Acute Rapidly Spreading Infection in skin & Subcutaneous tissues..Following.. Wounds, Burns.. Highly Communicable..Massive Edema, Lymphatic's inflammation..Children. Impetigo: Pyoderma Superficial Layers Skin.. Epidermis, Blisters, Children.. Highly Communicable..followed Streptococcus Sore Throat or rarely S. aureus wound infection. 2/ – Scarlet fever: Following Group A Strept. Sore throat infection.. Erythematous skin rash due to release Erythrogenic Toxin.. Strawberry tong.. small children.. permanent immunity - Necrotizing fasciitis : Few strains group A , Minor trauma, Invasive infection, pyogenic exotoxins, Subcutaneous tissues & Fascia, Rapid spread necrosis..Sever tissue damage..Pain, Fever, Sever systemic illness.. Fatal without Rapid Antibiotic Treatment - Streptococcal Toxic Shock Syndrome: pyrogenic toxin /superantigens/TSS, Infected Trauma, Bacteremia, Respiratory & Multi Organ Failure.. 30% Death. Skin rash - Scarlet Fever B-H-Streptococci Diagnosis & Treatment Culture on blood, B-Hemolytic reaction, Gram-+ve cocci in chain, catalase-ve, Bacitracin-Susceptible Serotyping should used to confirm group of streptococcal infection.. A, B, C etc. using antisera against group-specific cell wall carbohydrate – Antigens (Lancefield classification) Penicillin is the drug of choice.. All Group A streptococci are very sensitive to penicillin. Patients with penicillin allergy may be given Erythromycin.. Azithromycin.. Less Common Bacterial Skin Infections N.gonorrhoea..Salmonella typhi or paratyphi.. General Skin rash..Rosa spots Soft chancre /chancroid : Haemophilus ducreyi..Gram-ve bacilli, STD.. Painful Skin Ulcer.. Extra Genitalia .. Common in Tropical Region. Syphilis: Treponema pallidum.. Genital ulcers.. Meningococemia: N. meningitidis.. Sepsis, Skin rash & hemorrhage..Thrombosis Rickettsia diseases: Small intracellular bacteria human, R. prowazeki (Typhus), R. rickettsii (Spotted fever).. Transmitted by body lice.. systemic diseases Pseudomonas aeruginosa : Wound infections, Burns /2 Bacillus anthracis.. Cutaneous Black Lesions.. Clostridium perfingens and other sp. : Necrotizing Fasciitis.. Myonecrosis, Cellulitis, tissues putrefaction, gas production/ Gas gangrene.. Surgical/Traumatic wound.. Skin- Subcutaneous (Mixed Infection).. Specific Enzymes & Exotoxins Borrelia Burgdorferi : Lyme disease .. Transmitted by Tick/ Insect bites.. Incub. 1-3 weeks.. Annular Rash.. Chronic Skin Lesion.. Cardiac & Neurological Abnormality.. Arthritis.. Endemic USA, China, Japan Bartonella species: G-ve bacilli Bartonellosis Cat Scratch Fever..followed Cat scratch or bite..Skin lesions.. Subacute regional lymphadenitis..Septicemia. Tuberculosis-Leprosy-1 Cutaneous Tuberculosis (TB).. Cutaneous TB is a relatively uncommon form of extra-pulmonary TB.. Rare M. tuberculosis.. Common M. marinumulcerans.. Low Temperature..Water.. Skin Lesions.. Chronic cutaneous ulcer.. Small granulomas Follow skin injury..Trauma. Leprosy: Chronic bacterial infection caused by M. leprae.. It primarily affects cold body sites skin, mucous membranes.. peripheral nerves ..nose, ears, eye lids and testes. characterized by multiple skin lesions accompanied first by sensation loss/ anesthesia.. sensory loss in the affected areas, toes, finger tips, tissue destructions. Leprosy-2 Leprosy-3 3/ Lebrosy can affect people of all races around the world. However, it is most common in warm, wet areas in the tropics and subtropics. In most cases, it is spread through long-term contact with a person who has the disease but has not been treated. Most people will never develop the disease even if they are exposed to the bacteria.. have a natural immunity to leprosy. Worldwide prevalence is reported to be around 5.5 million, with 80% of these cases found in 5 countries: India, Indonesia, Myanmar, Brazil and Nigeria. Clinical Leprosy-4 Infection incubation period range from 6 months - 40 years or longer. usually begins in the extremities Leprosy forms depend on the person's immune response to the infection. There are several forms of leprosy: Tuberculoid form.. Mild Form.. Few AF Bacilli, Lepromin skin test +ve, Presence nerve sensation lepromatous type Severe form.. Numerous Acid-fast bacilli, Loss nerve sensation.. Lepromin skin test -ve Diagnosis & Treatment Lab Diagnosis: A skin biopsy may show characteristic granulomas (mixed inflammatory cell infiltrate in the deeper layers of the skin, the dermis) with involvement of the nerves. Presence Acid fast bacilli.. number of bacilli visible depending on the type of leprosy.. No Culture.. No Protected Vaccine available.. BCG may help & reduce the severity of disease Treatment: Dapsone, Rifampin, Clofazimine. Life-long Treatment ..No Cure but Less Tissue Damage and Spread of Infection. Common Fungal Skin Infection-1 Superficial & Cutaneous Mycosis: Invade only dead tissues of the skin.. keratinized body tissues.. Skin, Hair, Nails. causes skin peeling, redness, itching, burning.. less blisters and sores. Malnourishment, poor hygiene, suppressed immunity & warm moist climate may increase the incidence fungal skin infection Dermatophytes: Trichopyhton, Microsporum, Epidermatophyton spp., Yeast forms Piytrosporum, Trichosporons ..present in hair follicles & skin folding. Transmission: Usually from person to person or animal to person.. dust particles..common more with chronic skin disorders. Tinea Corporis Tinea pedis -Tinea capitis kerion Skin Fungal Infection-2 Tinea capitis: Hair follicles, scalp circular patches.. Scaling, Hair Loss..Children..Rare adults Tinea corporis: Skin annular-erythematic lesions, Vesicles, Scaling.. Itching.. Rash.. All Ages.. Mostly caused by Dermatophytes ..rarely mixed with Yeast Tinea pedis : Red vesicles.. Interdigital spaces, web lesions, Toes, Plantar surface.. Feet, Itching.. Chronic lesions..Wearing tight shoes/socks, increased feet sweating.. More in Adults than children.. Cased by all Dermatophytes. Tinea cruris: Pelvic area.. Groin.. Erythematic Lesions, Itching, Chronic.. more common in male young adults..mostly Epidermophyton spp Skin Fungal Infection-3 Tina unguium (Onychomycosis): Mostly caused by Trichophyton ,Microsporum.. less Candida..fingernails & toenails. Nails become colorless/dark colored, thicken, disfigure and brittle..Diabetes Psoriasis is a common skin disorder produces thick red plaques covered with silvery scales..can affect the nails, scalp, skin and joints..not caused by fungus and not transmitted to others. Eczema develops due to multiple immunological & other medical conditions.. Skin becomes inflamed or irritated..No infectious agent involved. Aspergillus & Cryptococcus spp. Rare cause localised skin or nail.. Onychomycosis-Psoriasis Skin Fungal Infection-3 Tinea Versicolor/Pityriasis: Malassezia furfur / Piytrosporum folliculitis.. Lipophilic Yeast ..difficult to culture in Labs. Part skin flora.. Endogenous infection.. Skin Moist-Folded Area.. Discoloration.. Red Spots.. Mostly FaceNeck Finger Trunk..Mild..rarely Chronic, Stress conditions, UV-Light, Common in young adults. Head dundruff, Seborrheic dermatitis. White & Black Piedra..Trichosporon spp., Soft to hard nodules. scalp hair & hair shaft , skin face , any body part. Yeat skin infection Candidasis: C. albicans, C. glabrata, C. tropicalis.. Other spp. Endogenous infection..moist folds of skin.. Lesions, finger nails, toenails, Finger webs.. Diabetes, immuno-compromessed.. more common in Infant & women.. Candida infections can look just like other types of dermatitis /eczema or skin allergy. itching, redness..infection Blasmycosis: Blastomyces dermatitidis & Histoplasmosis : Histoplasma capsulatum.. Dimorphic Fungi.. Soil ..Spore Inhalation.. Respiratory infection.. Systemic Infection.. Complications: Skin ulcerations/lesions Granulomas..causes severe damages..common USA, Canada Tinea Pityrisis / versicolor Seborrheic dermatitis Lab diagnosis-4 Direct microscopic examination of skin scales dissolved in a 10 % solution potassium hydroxide (KOH).. demonstrating the fungus as small Filaments / Yeast like structures. Culture: Sabouraud Dextrose agar, Incubation at room temperature & 37 C for 2-6 Weeks. . Slow growth for Dermatophytes..Rapid growth Candida. ChromCandida agar.. used for rapid identification of common Candida species. Treatment: Most skin infections respond very well to topical antifungal drugs..Less systemic drug .. interact with Ergosterol ..causing Fungal Cell membrane disruption.. Imidazole drugs ..miconazole, clotrimazole, econazole, ketoconazole, fluconazole