Acute Postoperative
advertisement

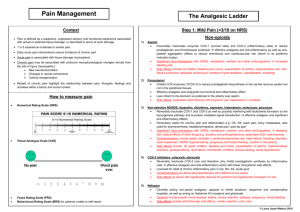
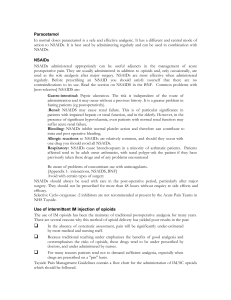
Management of Acute Postoperative Pain Dr Alice Man Department of Anaesthesia & Intensive Care The Chinese University of Hong Kong Prince of Wales Hospital Case scenario You are a houseman in an acute hospital • “By any reasonable code, freedom from pain should be a basic human right, limited only by our knowledge to achieve it” • - Liebeskind JC & Melzack R IASP definition of Pain • An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. Why should we treat postoperative pain? Principles of postop pain Mx Factors affecting postop pain • A. Surgical factors: • 1. site of incision and nature of the surgery • upper abdomen > thoracotomy > lower abdomen > limbs • 2. complications, eg wound infection, intraabdominal sepsis, distension • B. Patient factors: • Psychology, genetic, hx of substance abuse, hx of chronic pain Causes of postop pain • 1. Incisional- skin and subcutaneous tissue • 2. Deep- cutting, coagulation, trauma • 3. Positional- bed sore, nerve compression & traction • 4. IV site- needle trauma, extravasation, venous irritation • 5. Tubes- drains, nasogastric tube, ETT • 6. Respiratory- from ETT, coughing, deep breathing • 7. Rehab- physiotherapy, movement, ambulation • 8. Surgical- complication of surgery • 9. Others- cast, dressing too tight, urinary retention Acute pain service • 1. Education • 2. introduction and supervision of more advanced analgesic techniques e.g. iv PCA • 3. improvement of traditional analgesic Tx • 4. standardization of equipment, standing order, guidelines, protocol • 5. 24-hr availability of pain service personnel • 6. collaboration and communication with other medical staff • 7. audit of pain service • 8. research How can we assess pain? Pharmacology What drug to give? Analgesic • 1. Simple analgesic • Paracetamol-for mild pain, caution with liver impairment • Dologesic- paracetamol+propoxyphenemild to moderate pain • • • • 2. NSAID Mild and moderate pain Opioid sparing SE: peptic ulcer and bleeding, platelet aggregation inhibition, bronchospasm, renal impairment, allergy • CI: bleeding, hypovolaemia, GIB, pregnancy, breast feeding, hypersensitivity, renal impairment, asthma • 3. Opioid • e.g. morphine, pethidine, fentanyl , codeine phosphate, methadone, dextro-propoxyphene • Desirable effects: Analgesia, Sedation • Adverse effects: Over sedation, Respiratory depression, Nausea & vomiting, Pruritus, Urinary retention, Constipation, Dysphoria, hallucination, Addiction • • • • 4. Local anaesthetics e.g. bupivacaine (marcain), lignocaine used in epidural and regional analgesia features of LA toxicity : perioral numbness, dizziness, tinnitis, diplopia, drowsiness, convulsion coma, respiratory depression, CVS depression How to give? Methods of postop analgesia • 1. Oral/ PR • 2. Intramuscular • 3. intravenous-intermittent bolus, continuous infusion 4. Epidural analgesia 5. Spinal 6. Regional block-brachial plexus block Patient controlled analgesia Non-pharmacological • 1. Psychotherapy: distraction, information • 2. Behavioral therapy: modification • 3. Physical therapy: TENS, acupuncture, cryoanalgesia, heat therapy Postop Nausea & vomiting Consequence of PONV • Delayed in oral intake, dehydration, e imbalance • Tachycardia, arrhythmia, salivation, pallor • Oesophageal tear, disruption of surgical anstomosis, wound dishiscence, increased ICP, IOP, haematoma • Aspiration pneumonia • Delayed in discharge, unplanned hospital admission Case scenario You are a houseman in an acute hospital Case 1 • While u are having dinner in the canteen, a ward nurse call u, “Mrs Chan came back from OT just now and her recent blood pressure is 70/40. She has an epidural.” • What are u going to do? • What is the definition of “shock”? • Any investigation? Hypotension • Epidural analgesia- sympathetic blockade, iv PCA • Ddx: hypovolaemia, cardiogenic, distributive, obstructive • Mx: • 1. Assess patient, recheck BP • 2. ABC • 3. give O2 • 4. stop epidural infusion, iv PCA • 5. iv fluid challenge, vasopressor • 6. exclude other causes e.g. haemorrhage Case 2 • Mr Chan, 50yr old gentleman, postop D2, on iv PCA LOC • What will u do? • What are the differential diagnosis? • What is the management for opioid overdose? Opioid overdose • Causes: human error, equipment malfunction, patient risk factors, • Presentation: Altered conscious state, slow RR, desaturation, small pupil • Ddx: stroke, electrolyte disturbance, hypoxaemia, hypercarbia, hypotension Mx • • • • • • • 1. ABC 2. ? drowsy, rousable 3. stop PCA/ Continuous infusion 4. give O2 via mask, ambu bag 5. monitor closely 6. inform APS 7. give 0.1mg naloxone iv and repeat 3-5min as necessary Case 3 • • • • • • 60 years old female morbidly obese evidence of obstructive sleep apnoea on DVT prophylaxis - fraxiparine require anterior resection You are an anaesthetist, what mode of postop analgesia would you choose? • Any precautions concerning the postop analgesia? Choice of analgesic modality • 1. Patient factors: physical conditions, age, cognitive ability, previous experience, psychological state, oral diet, drug interaction • 2. Surgical factors: type and extent of surgery, surgical complication • • 3. Anaesthetic factors: anasthetic technique, expertise, available resource, ward nurse training Considerations • • • • • abdominal surgery adverse effect of pain to heart effect of systemic opioid effect of anti-coagulant technical difficulty on epidural insertion Options: • Options – opioid - IV PCA – epidural - PCA Pethidine – epidural infusion - LA + fentanyl • Note – anticoagulant and epidural Case 4 • Miss J, a 20 yr old patient just had a laparoscopy performed and asked u, “ Can I get some antiemetic?” • What would u do? • What are the risk factors for postop nausea & vomiting? • Any treatment? High risk of PONV • Patient: young, F, early preg, previous hx of PONV, motion sickness, anxiety • Increased gastric vol: obesity, blood in stomach • Anaesthetic technique: RA vs GA, N2O, opioid • Surgical: duration, laparoscopy, eye, ear operation • Post op: pain, movement, hypotension, forced oral fluid Mx • Ensure pain control, adequate hydration, oxygenstion, slow and deep breath, stable BP, gentle handling of pt Pharmacological • • • • • • • -Anticholinergic: scopolamine -Phenothiazine: prochlorperazine, promethazine -Butyrophenones: droperidol -Benzamides: metoclopramide -Antihistamine: cyclizine, diphenhydramine -Corticosteroid: dexamethasone, betamethasone -5-HT antagonist: ondansetron, topisetron Non-pharmacological • NGT? • Acupuncture Thank you.