Factors Affecting the Postoperative Pain
advertisement

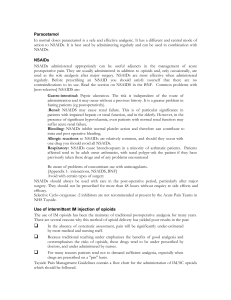
Management of Postoperative Pain Dr Alice Man Department of Anaesthesia & Intensive Care The Chinese University of Hong Kong Prince of Wales Hospital “By any reasonable code, freedom from pain should be a basic human right, limited only by our knowledge to achieve it” - Liebeskind JC & Melzack R IASP definition of Pain: An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. Physiological mechanism of acute pain: 1. Nociceptors 2. Peripheral chemical mediators 3. Pain transmission pathways 4. Pain modulation Why should we treat postoperative pain? Possible harmful effects of untreated severe acute pain: A. Cardiovascular- activation of sympathetic nervous system→ 1. hypertension, tachycardia, ↑ myocardial contraction, vascular resistance→↑ myocardial O2 demand 2. decreased coronary vasoconstriction→ ↓ myocardial O2 supply →myocardial ischaemia B. Respiratory- surgical incision and pain→ 1. splinting diaphragm, reflex inhibition of phrenic nerve→ decreased lung volume, atelectasis 2. poor cough, sputum retention→postoperative pneumonia, hypoxaemia C. Gastrointestinal- activation of spinal reflex arc→impaired gastric and intestinal motility→ ileus D. Genitourinary- Urinary retention E. Neuroendocrine: release of stress hormones e.g. catecholamines, GH, cortisol, glucagons ACTH, ADH, rennin, angiotensin II and interleukin→ Hyperglycaemia, increased coagulability, protein breakdown, negative nitrogen balance, impairment of wound healing, immune function, Na and water retention, increased metabolic demand F. Musculoskeletal 1. muscle spasm→Reduce resp function 2. immobility→ increased venous stasis, DVT G. Psychological Anxiety, fear, insomnia, fatique, aggressive behaviour H. Chronic pain Inguinal hernia, mastectomy, thoractomy General Principles of Pain management: 1. Proper assessment (site, nature of severity) and control of pain require patient involvement. 2. Effective analgesia requires flexibility and tailoring of Tx to individual patient: route, dose of medication 3. While it is not always possible to completely alleviate pain, it should be possible to reduce pain to a tolerable or comfortable level. 4. Reevaluate for effectiveness, SE of Tx and treat accordingly. Factors Affecting the Postoperative Pain: A. Surgical factors: 1. site of incision and nature of the surgery upper abdomen > thoracotomy > lower abdomen > limbs 2. complications, e.g. wound infection, intraabdominal sepsis, distension B. Patient factors: Psychology, genetic, hx of substance abuse, hx of chronic pain Causes of Post-Operative Pain: 1. incisional skin and subcutaneous tissue 2. deep cutting, coagulation, trauma 3. positional bed sore, nerve compression & traction 4. IV site needle trauma, extravasation, venous irritation 5. tubes drains, nasogastric tube, ETT 6. respiratory from ETT, coughing, deep breathing 7. rehab physiotherapy, movement, ambulation 8. surgical complication of surgery 9. others cast, dressing too tight, urinary retention Acute Pain Service (APS): 1. Education 2. introduction and supervision of more advanced analgesic techniques e.g. iv PCA 3. improvement of traditional analgesic Tx 4. standardization of equipment, standing order, guidelines, protocol 5. 24-hr availability of pain service personnel 6. collaboration and communication with other medical staff 7. audit of pain service 8. research Pain assessment: 1. Simple ranking: no pain, mild pain, moderate pain, severe pain 2. Verbal numeric scale (VNS): 0 1 2 3 4 5 6 7 8 9 10 no pain unbearable 3. faces rating scale (for children): Pharmacology 1. Simple analgesic Paracetamol-for mild pain, caution with liver impairment Dologesic- paracetamol+propoxyphene- mild to moderate pain 2. NSAID e.g. ketorolac, diclofenacl naproxen, piroxicam, ibuprofen, indomethacin - Mild and moderate pain - Opioid sparing - SE: peptic ulcer and bleeding, platelet aggregation inhibition, bronchospasm, renal impairment, allergy - CI: bleeding, hypovolaemia, GIB, pregnancy, breast feeding, hypersensitivity, renal impairment, asthma 3. Opioid e.g. morphine, pethidine, fentanyl , codeine phosphate, methadone, dextro-propoxyphene Desirable effects – Analgesia – Sedation Adverse effects – Over sedation – Respiratory depression – Nausea & vomiting – Pruritus – Urinary retention – Constipation – Dysphoria, hallucination – Addiction 4. Local Anaesthetic e.g. bupivacaine (marcain), lignocaine -used in epidural and regional analgesia -features of LA toxicity : perioral numbness, dizziness, tinnitis, diplopia, drowsiness, convulsion coma, respiratory depression, CVS depression Methods of Acute Postoperaive Pain Relief: A. Pharmacological 1. Oral e.g. paracetamol, NSAID -if patient can tolerate oral intake 2. PR e.g. paracetamol, voltaren, tramadol -unpleasant -delayed onset -variable absorption 3. Intramuscular -often ineffective -individual patient variation in dose-response -fluctuating blood level on prn basis -delay in injection and absorption -pain on injection 4. Intravenous -intermittent bolus: fast onset, need close monitoring, need repeated small bolus, fluctuating blood level -continuous infusion: need close monitoring, more steady blood level, dfficult to judge optimal dose 5. Patient Control Analgesia (PCA) - sense of being in control of analgesia, no delay, higher satisfaction, therapeutic level maintained, ? lower dose of overdose 6. Epidural analgesia Mode of administration – intermittent opioid bolus – PCA opioid – continuous infusion - LA+opioid Advantages – most effective analgesia – systemic effect of opioid minimal – pre-empty analgesia – reduce incidence of thromboembolism Side Effects From the technique – dural puncture – epidural haematoma – epidural abscess – nerve root trauma From LA – hypotension – paraesthesia – motor weakness From opioid – delay resp depress – urinary retention – pruritus – herpes simplex 7. Intrathecal 8. Regional block 9. Transnasal e.g. Butorphanol 10. transmucusal e.g. fentanyl lollipop 11. sublingual e.g. Buprenorphine B. Non-Pharmacological Methods 1. Psychotherapy – distraction – information 2. Behavioral therapy – modification 3. Physical therapy – TENS – acupuncture – cryoanalgesia – heat therapy Choice of analgesia modality: 1. Patient factors – physical conditions – age, cognitive ability – previous experience – psychological state – oral diet ? – drug interaction 2. Surgical factors – type and extent of surgery – surgical complication 3. Anaesthetic factors – anasthetic technique – expertise – available resource – ward nurse training Emergency! Opioid overdose: Causes: human error, equipment malfunction, patient risk factors, Presentation: Altered conscious state, slow RR, desaturation, small pupil Ddx: stroke, electrolyte disturbance, hypoxaemia, hypercarbia, hypotension Mx: 1. ABC 2. ? drowsy, rousable 3. stop PCA/ Continuous infusion 4. give O2 via mask, ambu bag 5. monitor closely 6. inform APS 7. give 0.1mg narloxone iv and repeat 3-5min as necessary Hypotension: Epidural analgesia- sympathetic blockade, iv PCA Ddx: hypovolaemia, cardiogenic, distributive, obstructive Mx: 1. Assess patient, recheck BP 2. ABC 3. give O2 4. stop epidural infusion, iv PCA 5. iv fluid challenge, vasopressor 6. exclude other causes e.g. haemorrhage Nausea and vomiting Ddx: residual anaesthetic effect, pain, hypoxaemia, hypotension, mechanical (abdominal distension, ileus) Mx: 1. assess patient: check BP, pulse, conscious level, Sa O2 2. exclude other causes 3. reassure patient 4. give antiemetic 5. alternative analgesia if necessary Pruritis Opioid, esp intrathecal, epidural use Ddx: local irritation Mx: 1. assess patient, ?skin rash, local irrtation 2. give chlorpheniramine iv, oral 3. if severe, alternative analgesia 4. low dose naloxone Urinary retention sympathetic blockade Ddx: obstructive Mx: 1. assess patient, palpate bladder 2. bladder catheterization 3. low dose naloxone Leg weakness/ Paraesthesia Motor/ sensory fibre blockade by epidural LA Ddx: spinal cord compression e.g. epidural haematoma, abscess, spinal cord ischaemia due to surgery, severe hypotension, toxic effect of LA on nerve and spinal Cord Mx: 1. assess, exclude other causes (check back pain, sensory and motor deficit, bowel and bladder incontinence) 2. reassure patient and ensure no injury to limbs w/ weakness 3. inform APS Postop Nausea & Vomiting Pathophysiology of Nausea & Vomiting High risk of PONV: • Patient: young, F, early preg, previous hx of PONV, motion sickness, anxiety • Increased gastric vol: obesity, blood in stomach • Anaesthetic technique: RA vs GA, N2O, opioid • Surgical: duration, laparoscopy, eye, ear operation • Post op: pain, movement, hypotension, forced oral fluid Mx: 1. identify cause of PONV and ensure pain control, adequate hydration, oxygenstion, slow and deep breath, stable BP, gentle handling of pt 2. pharmacological tx: -Anticholinergic: scopolamine -Phenothiazine: prochlorperazine, promethazine -Butyrophenones: droperidol -Benzamides: metoclopramide -Antihistamine: cyclizine, diphenhydramine -Corticosteroid: dexamethasone, betamethasone -5-HT antagonist: ondansetron, topisetron 3. Non-pharmacological: NGT? Acupuncture