MUKHAPAAKA- SARVASARA.
Dr. Pranav Bhagwat.
This is that
Ayurvedic View
Definition
- सुश्रुत नि. १६
हे तु
- वाग्भट उ. २१
- चरक स.ू २४
- भेलसंहहता चच.
६
- भेलसंहहता चच. ६
रूप
- वाग्भट उ. २१
Mukhpaak
laxan
Vataj
Sushrut
Sphotyukta and
arun varniya vranotpatti.
vagbhat
Ulcers are mild red in colour.
Lips are coppery.
Tongue is intolerant to cold,
heavy and cracked.
Patient opens his mouth with
difficulty. (trismus)
Laxan
Pittaj
sushrut
Rakta or pittvarniya
vranotpatti in mukha.
daha.
vagbhat
. daha
tiktvakrata (bitter taste in
mouth)
ulcears appaears as those
produced by application of
kshara.
Laxan
kaphaj
Sushrut
Kandu,
mand vedana
tvak varniya vranotpatti.
Vagbhat
Madhurasyata,
Kanduyukta
picchila vranotpatti
Raktaj
Laxan
Sushrut
Rakt or pitvarniya
vranotpatti in
mukha.
daha
vagbhat
There is daha
Tiktvaktrata.
ulcears appaears as
those produced by
application of kshar
Laxan
Sannipatik
Vagbhat
In sannipatik mukhpaak
tridosha laxanas are
observed.
- भावप्रकाश मख
ु रोग चच.
Mukhpaak samanya chikitsa
Siravedh and shirovirechan
Kaval dharan of madhu, gomutra, dugdha, ghrita.
Kaval dharan of darvi svaras
Gandush of patoladi qwath.
Khadiradi gutika
Patyha vati
Chikitsa for vataja mukhpaak
Pratisarana with panchalavan churna.
Nasya with vaathar dravya siddha oil
Snaihik dhumpaan with drugs lke arjun, erand, khadir, guggul
and jatamansi.
Churna of pippali, saindhav and ela should be applied at the
site of vrana
Chikitsa for pittaj and raktaj
mukhpaak
Firsly shodhan has to be done by vaman and virechan by madhur
and shit dravya.
Gandush done with sugarcane juice or sugar water.
Madhur dravya siddha dugdha used for gandush, kaval dharan
and nasya.
Chewing the leaves of madayantika and spitting it out.
Chikitsa for kaphaj
mukhpaak
Pratisaran with kutaki, kshar and lavan
Gandush done with gomutra added with ash of
palash, mushkaka and amlaki.
Leaves of phanijjaka, nirgundi and surasa(tulasi)
are chewed and spitted out
Chikitsa for sannipatik mukhpaak
Tratment should be done according to
predominance of doshas.
Gorochan, kasis, saurastrika, rasanjan
and mocharas boiled together added with
honey and kept in an iron vesel. After it
dries it is powdered mixed with honey and
applied on ulcers
- भावप्रकाश मख
ु रोग चच.
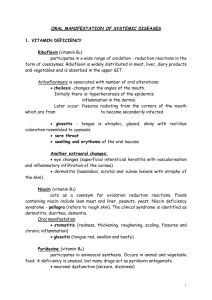
ULCERS OF ORAL CAVITY
INFECTIONS
VIRAL-HERPANGINA, HERPES SIMPLEX
BACTERIAL-Vincent’s infection, TB, syphilis
Fungal: Candidiasis
Immune disorders: Aphthous ulcer, Behcet’s syndrome
Trauma
ill-fitting denture, phenol, aspirin burns, Hot food
Neoplasms
Skin disorders: Erythema multiforme, lichen planus,
BMMP, bullous pemphigoid, lupus erythematosus
Blood disorders: Leukaemia,
agranulocytosis, pancytopenia
Drug allergy: Mouth washes, tooth
paste, etc.
Reactions to systemic drugs
Vitamin deficiencies
Miscellaneous: Radiation mucositis,
cancer chemotherapy, diabetes
mellitus, uraemia
INFECTIONS
HERPANGINA
SYN: Vesicular stomatitis , Acute
lymphonodular pharyngitis
Cause: Enteroviruses-Coxsackie A, EV
71
Characteristic vesicular rash on
tonsillar pillars, soft palate, uvula,
tonsils, posterior pharyngeal wall
Discrete 1- to 2-mm vesicles and ulcers
Enlarge over 2-3 days to 3-4 mm and
are surrounded by erythematous rings
up to 10 mm
1-15 lesions are present, usually
around 5
Usually resolve without complications
Rarely, meningitis
Herpetic gingivostomatitis
Syn: orolabial herpes
Cause: HSV
Primary
Children
Clusters of multiple vesicles ->
ulcers
Fever, malaise and headache , sore
throat and lymphadenopathy.
Secondary
Adults, mild
Vermilion border of the lip > hard
palate and gingiva
Reactivation of dormant virus in
trigeminal ganglion
Acyclovir, 200 mg, five times a day
for 5 days to reduce viral load
Moniliasis (candidiasis)
caused by Candida albicans
Thrush
white grey patches on the
oral mucosa and tongue.
infants and children
systemic malignancy and
diabetes or taking broad
spectrum antibiotics,
cytotoxic drugs, steroids or
radiation.
Thrush can be treated by
topical application of
nystatin or clotrimazole.
Hand, foot and mouth
disease
Cause: Coxsackievirus A16
and enterovirus 71 (EV71)
spread via the fecal-oral and
perhaps respiratory routes
primarily in children
vesicular palmoplantar
eruption and erosive
stomatitis.
Cloudy vesicles with a red
halo are highly characteristic
of this disease.
IMMUNE DISORDERS
Aphthous ulcers
Recurrent and superficial
Aetiology: Unknown. Autoimmune,
Nutritional (Folate, B12, Iron), Viral,
Bacterial, Food allergies, Hormonal,
Stress
usually involving movable mucosa,
i.e. inner surfaces of lips, buccal
mucosa, tongue, floor of mouth and
soft palate, sparing mucosa of the
hard palate and gingivae.
Minor form
more common,
ulcers are 2–10 mm in size and
multiple with a central necrotic
area and a red
They heal in about 2 weeks
without leaving a scar.
Major form, ulcer is very big, 2–4
cm in size, and heals with a scar but
is soon followed by another ulcer.
Behcet’s syndrome (Oculooro-genital syndrome)
Behçet's disease is a complex multisystem disease
characterized by oral and genital ulcers and other
systemic features.
Diagnosis is based on the International Criteria for
Behçet's Disease including:
oral aphthae,
genital aphthae,
ocular lesions,
cutaneous lesions,
and a positive pathergy test.
Cutaneous lesions should display a neutrophilic
vascular reaction on histopathologic examination.
Seen worldwide, with the highest prevalence
reported in Turkey and Japan
prevalence and often the severity is increased
in the Middle East and the Mediterranean
predominantly affect males
Cause and Pathogenesis
Heredity, immunologic factors, infectious
agents, inflammatory mediators, and
clotting factors likely contribute.
Oral aphthae, or Canker sores
are often the initial feature of
Behçet's disease and constitute
a requisite diagnostic feature
usually occur in crops of more
than 3 to 10s
painful and shallow, and they
heal without scarring over 1 to 3
weeks
Genital ulcers typically occur on
the scrotum and penis in males
and on the vulva or vaginal
mucosa in females.
These aphthae are similar in
appearance to oral lesions, but
they have a greater tendency to
scar and may recur less
frequently.[
Cutaneous
erythema nodosum–like lesions,
pyoderma gangrenosum–like lesions,
Sweet's syndrome–like lesions,
cutaneous small vessel vasculitis, and
pustular vasculitic lesions including
lesions induced by trauma—the socalled pathergy lesion.
Pathergy signifies the development
of erythematous pustules or papules
24 to 48 hours following puncture of
the skin with a 20- to 21-gauge
sterile needle.
Specimens from all these lesions
demonstrate a neutrophilic vascular
reaction on histopathologic analysis.
Ophthalmic (83% to 95% of men
and 67% to 73% of women)
anterior and posterior uveitis,
retinal vasculitis, and hypopyon, with
secondary glaucoma,
cataract formation, decreased visual
acuity, and synechiae formation
Arthritis of Behçet's disease is typically a
nonerosive, inflammatory, symmetric, or
asymmetric oligoarthritis
Central nervous system (CNS) involvement is
most commonly characterized by
brain stem or corticospinal tract syndromes
(neuro-Behçet's syndrome),
venous sinus thrombosis,
increased intracranial pressure
isolated headache.
Cardiac complications include
myocardial infarction,
pericarditis,
arterial and venous thromboses, and
aneurysm formation.
Submucous Fibrosis
Definition:
Submucous fibrosis represents a multifactorial
disorder;
with the considered chief etiologic factor being the
consistent and habitual use of areca (betel) nut,
either in the form of chewing or simply placing a quid
of material (paan masala) in the buccal or labial
sulcus several time per day, or in a packaged
powdered form with other components (guthka), over
many years.
premalignant condition with transformation rates as high
as 7.6%
Etiology and pathogenesis:
failure of collagen remodeling
altered epithelial-mesenchymal interactions >formation of collagenous bands and aggregates
within the submucosa and lamina propria.
diminished level of functional collagenase levels
Clinical Features
Changes of submucous fibrosis are
most marked over soft palate, faucial
pillars and buccal mucosa
Initial mucosal alterations: erythema
with or without vesiculation.
Later: slow diminishment of
erythema and a progressive decrease
in the degree of oral opening and
tongue mobility
Pallor of the normally pink mucosa
becomes evident as the underlying
chronic inflammation recedes and
fibrosis and hyalinization progress.
Scar bands may become evident
deep within the buccal soft tissues,
further limiting jaw opening and
function.
Development of squamous cell
carcinoma is characterized by a
gradual thickening of the epithelial
surface with hyperplastic to
verrucous surface qualities becoming
evident.
Histology:
juxtaposition of atrophic
epithelium surfacing a
subjacent fibrosis.
Early connective tissue
alterations are
characterized by delicate
and loosely arranged
collagen fibers with
progressive degrees of
hyalinization
In the late stages:
complete hyalinization
of the supportive
connective tissue.
Variable degrees of
chronic inflammation
occur in the form of
lymphocytes and
plasma cells.
Variable levels of
dysplasia have been
noted.
Management of oral submucous
fibrosis is problematic, particularly in
advanced cases and when the use of
areca-containing products remains in
place.
Medical:
Avoid irritant factors
Topical injection of steroids-Dexamethasone
Treat existent anaemia or vitamin deficiencies
Encourage jaw opening exercises.
Surgical
Surgical release procedures of scar bands have been
only modestly successful.
More recently collagenase and
pentoxifylline administration in separate
studies has been proposed
Other conditions.
Migratory Glossitis
The grooves running laterally
across the tongue are one
obvious diagnosis (fissured
tongue). The white areas
suggest another diagnosis.
Note that some of white areas
form partial rings, a
characteristic of geographic
tongue. Usually the tongue
looks red in the center of the
rings; however, in this case
the entire tongue looks red
obscuring these features
except at the tip where the
typical appearance is
preserved. The two vesicles
on the near lateral surface are
probably related to
geographic tongue
Nicotine Stomatitis
The white color of this patient's
hard palate and the white
elevations with red centers are
characteristic of nicotine
stomatitis. The red dots are the
orifices of minor salivary gland
ducts the epithelium of which
does not keratinize. This patient
should be informed that the
smoking habit has caused these
changes and that a malignancy
may develop here or elsewhere.
Suppurative Apical Periodontitis
The raised, red gingival
lesion is probably
associated with the carious
mandibular first molar
tooth. There probably is a
periapical lesion at the
molar apex that is draining
onto the surface. If so, the
lesion is located at the
drainage site. While the
lesion could be called a
"pyogenic granuloma," it
is commonly called a
"parulis."
Median Rhomboid Glossitis
The rough reddish area in
the midline of the tongue is
median rhomboid glossitis-few other diseases occur
in this location. For years,
it has been assumed that
median rhomboid glossitis
is cause by faulty tongue
development; however,
more recently, Candida
infestation has been posed
as its etiology.
Lichen Planus
The white intersecting lines
affecting this patient's
buccal mucosa is
characteristic of lichen
planus. This condition may
occur on the skin, on the
oral mucosa, or on both
skin and mucosa. It is
usually bilateral and may
sometimes cause ulceration
(erosion) of the mucous
membrane. The red
posterior area may be the
beginning of such "erosive
lichen planus."
Lichen planus
Oral lichen planus (OLP) can occur
without cutaneous disease.
Onset before middle age is rare;
the mean age of onset is in the
sixth decade.
Women outnumber men by more
than 2:1.
Mucous membrane involvement is
observed in more than 50% of
patients with cutaneous lichen
planus
The most common location of OLP
is the buccal mucosa (80% to
90%) followed by the tongue
(30% to 50%)
Lavy white lesions on buccal m
Angular stomatitis
Ulcerative stomatitis