The RPR and VDRL tests - Course Materials in Medical Laboratory
advertisement
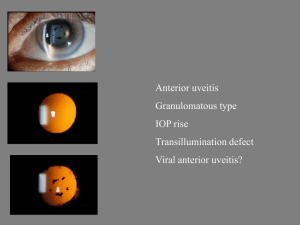
The Rapid Plasma Reagin Test and the Venereal Disease Research Laboratory Assay (VDRL) Serological Diagnostic Screening Tests for Syphilis Syphilis: Causative Agent and Disease Description Treponema pallidum - the causative agent for the disease known as syphilis. Order: Spirochaetales Family: Treponemataceae. Genus: Treponema, a slender, tightly coiled, pointed-ended, 6-10 axial filamentous gram negative rod. Causative Agent T. pallidum- a microaerophilic, obligate parasite that requires mammalian cells for survival. Covered in a sheath, aids this organism in it’s pathogenicity by reducing or limiting antigenic stimulation of the host’s immune system. Members of this genus contain of a number of species that can exist as either commensal flora or human pathogens. Treponema Speciation Nonpathogenic-exists as commensal flora of the oral cavity, gastrointestinal and urogenital tract. Are also considered to be strict anaerobes. Pathogenic-transmitted by person-to-person contact. The microaerophilic subspecies of pallidum are associated with various TreponemaRelated Diseases in humans Treponema pallidum sub speciation T. pallidum subspecies pallidum - syphilis T. pallidum subspecies pertenue - yaws T. pallidum subspecies endemicum - non-venereal (endemic) syphilis/bejel T. carateum - pinta Species- indistinguishable serologically and morphologically. Differentiation- based on clinical & epidemiological characteristics. Disease State Untreated, syphilis is a chronic infectious disease with many clinical manifestations that occur in distinct stages consisting of subacute symptomatic periods separated by asymptomatic intervals. Initially, T. pallidum penetrates intact mucous membranes or enter the body through tiny defects in the epithelium. Upon entrance, the microorganism is carried by the circulatory system to every organ of the body. Clinical Manifestation The progression of untreated syphilis is generally divided into into four stages: Primary, Secondary, Latent and Tertiary (Late) Syphilis, with Tertiary Syphilis being further divided into Neurosyphilis and Congenital Syphilis. Spirochetemia occurs very early in infections before the appearance of the first lesion or reactive blood test described as clinical or serological detection. In this state, syphilis appears to be in an incubating state that can range from 10 to 90 days. Primary Syphilis Small, solitary nodule at the point of initial inoculation. Primary inflammatory lesion enlarges and ulcerates developing into a characteristic painless ulcer or chancre that heals spontaneously. Chancre are located on vaginal mucosa or cervix of the female and external genitalia of the male. Secondary Syphilis Systemic: within 2-8 weeks of visible chancre. Generalized illness being with viral-like symptoms: headache, sore throat, low-grade fever and occasionally a nasal discharge. Generalized rash of skin and mucous membranes. Secondary Syphilis Development of lymphadenopathy and lesions of the skin and mucous membranes. Lesions contain a large number of spirochetes and are highly contagious when exposed on the skin surface. Macular lesion and/or condylomata lata-flat lesions resembling warts in moist areas of the body (around the anus or vagina). Latent Syphilis Latency- exhibit no clinical symptoms, a noninfectious state which diagnosis can be made only by serologic methods. During the first 2-4 years, patient may exhibit one or more mucocutaneous relapses of secondary syphilis manifestation. During these relapses, patient is highly infectious and may transmit the disease. Tertiary Syphilis Characterized by the presence of destructive granulomas that produce lesions resembling segments of circles that heal with superficial scarring. Exhibited 3-10 years after primary infection. Skeletal system involvement Cardiovascular system-involves the aortic endothelium, weakening the blood vessels of the aortic arch known as syphilitic aneurysm. Other Clinical Manifestations of Tertiary Syphilis Neurosyphilis: Asymptomatic involvement of the CNS and detected only by examination of cerebrospinal fluid (CSF). Congenital Syphilis: Caused by maternal spirochetemia and transplacental transmission of microorganism. Neurosyphilis Acute syphilitic meningitis Meningovascular syphilis manifested as a seizure. Cerebrovascular accident - stroke General paresis, personality changes, dementia and delusional states. Tabes dorsalis- involvement of the posterior column and dorsal root, characterized by broadbased gait with impotence and bladder dysfunction. Congenital Syphilis Hutchinsonian triad: Hutchinson’s teeth, interstitial keratitis, and nerve deafness. Other characteristics- fissuring around the mouth and anus, skeletal lesions, perforation of the plate and collapse of nasal bones to produce a saddle-nose deformity. Immunological Manifestations Specific antibodies- produced against T. pallidum are IgM and IgG antibodies. Detected by Treponemal serological procedures Nonspecific antibodies-produced against the protein antigen group common to pathogenic spirochetes formed and are known as nontreponemal antibodies. Detected by nontreponemal serological procedures Diagnostic Evaluation The diagnosis of syphilis is based on the clinical picture in conjunction with demonstration of microorganisms in a lesion and serologic testing. Darkfield Microscopy Nontreponemal Methods- Venereal Disease Research Laboratory (VDRL) and the Rapid Plasma Reagin (RPR) procedures are used to screen patient’s serum. Treponemal Methods-Fluorescent Treponema pallidumabsorbed (FTA-ABS) and the microhemagglutination Treponema pallidum [MHA-TP]are used for confirmation. Clinical Limitations Associated with Serological Testing Infectious disease - measles, chicken pox, hepatitis, infectious mononucleosis, leptospirosis, malaria, leprosy, rickettsial disease, trypanosomiasis, lymphogranuloma venereum (LGV) Noninfectious conditions - autoimmune disorders, drug addiction, old age, pregnancy and recent immunization RPR test The RPR test is a nontreponemal testing procedure for the serologic detection of syphilis. Principle of RPR The RPR Card antigen suspension is a carbon particle cardiolipin antigen that detects reagin. Reagin is an antibody like substance present in serum or plasma from individuals with syphilis. The reagin binds to the test antigen which consists of cardiolipin-lecithin coated particles that cause macroscopic flocculation. Principle of RPR When a specimen such as serum or plasma contains antibody, flocculation occurs with the resulting aggregation of the carbon particles. The flocculation appears as black clumps against the white background of the plastic coated card. Principle of RPR Antibodies associated with syphilis begin to appear in the blood 4 to 6 weeks after infection. Nontreponemal tests determine the presence of reagin. Reagin is a nontreponemal autoantibody directed against cardiolipin antigens. Materials for RPR RPR Test Cards RPR Control Cards RPR Antigen Distilled Water Dispenstirs Rotator RPR Test Background The RPR test uses a white plastic coated card that consist of several circles that are 18 mm in diameter. The controls which are strongly reactive, moderately reactive, and non-reactive are contained on the control card in a dried form. Procedure for Controls A. Use Dispenstir to draw up distilled water B. Drop 1 drop on the card test circle for each patient sample. C. Invert Dipenstir and spread the water in the circle until the dried control is completely reconstituted. D. Add antigen as described for the patients E. Rotate for 8 minutes at 100 rpm Reactions for Controls The following reactions should be observed to compare against the test results: Reactive control - characteristic strong clumping. Reactive moderate control - moderate clumping. Non-reactive control - smooth, grayish appearance of unclumped particles Specimen Collection Specimen Collection *The addition of choline chloride, which inactivates complement enables the serum to be tested without prior heating. Unheated serumcentrifuge for sedimentation of cellular elements, serum may be frozen until time of testing. Heated Serum- transfer serum to clean tube and place in 56°C water bath for 30 minutes Specimen Collection Specimen Collection Unheated Plasma specimen should be collected with an anticoagulant such as EDTA or heparin, plasma must be stored at 2°C to 8°C. Plasma must be tested within in 24 hrs of collection. Procedure for Test Label rings on test card with numbers of samples to be tested Use Dispenstir to draw up serum sample. Hold Dispenstir in a perpendicular position directly over the test circle to which the specimen is to be delivered. Squeeze Dispenstir to allow 1 drop to fall on to each circle Procedure for Test Invert Dispenstir,and using the sealed end spread the specimen in the confines of the circle. Reconstitute the antigen bottle, by shaking. Holding the bottle in a straight vertical position drop one or two drops in the upper corner of each test circle, then place one “free falling” drop on each test area. Procedure for Test Rotate card for 8 minutes on a mechanical rotator at 100 rpm. The test card she also be covered with a humidifier cover. After rotating mechanically, the test card should be rotated manually by hand 3 to four rotations and then read immediately macroscopically in the “wet” state under a high intensity lamp. Results of Test The test results should be reported as reactive (even if minimally reactive) or nonreactive. All test results that are nonreactive should be quantitated. Explanation of Results A negative RPR test may indicate one of the following: 1. The patient does not have syphilis. 2. The infection is too recent for antibodies to be produced. (Repeated tests should be administered at 1 week, 1 month, and 3 month intervals to establish presence or absence of disease). 3. The syphilis is latent or inactive 4. Faulty immunodefense mechanism 5. Faulty lab techniques Explanation of Results A positive reaction is not conclusive for syphilis. Several conditions produce biologic false positive results for syphilis. (False positive means that the test revealed a positive reaction when it was actually negative). False positives may reveal the presence of other serious diseases. Non-syphilitic Conditions Giving Biologic False-Positive Results Malaria Leprosy Relapsing fever Infectious Mononucleosis Atypical pneumonia Viral pneumonia Lupus erythematosus Measles pregnancy drug abuse Resolving False Positive RPR Tests False positive RPR tests may be resolved by testing the patient’s serum with a specific treponemal antigen test. Explanation of Results Diagnosis of syphilis requires correlation of geographical area or country, patient history, physical findings, and results of syphilis antibody tests. T. pallidum is diagnosed when both the screening and confirmatory test are reactive. Explanation of Results Treponemal tests are more specific than non-treponemal tests Treponemal tests confirm syphilis when a reactive or positive non-treponemal result is obtained. Confirmatory Tests for Syphilis I. FTA-ABS flourescent treponemal antibody test II. TP-PA particle aggluntination T. pallidum test III. MHA-TP Microhemagglutination assay - T. pallidum Confirmatory Tests for Syphilis Treponemal tests are used to confirm reactive non-treponemal procedures. A positive FTA-ABS test almost always remains positive and therefore is not recommended for monitoring therapy. Theory of Antigen-Antibody Reaction It is theorized that reagin is an antibody against tissue lipids. Lipids are presumed to be liberated or free from body tissue in the normal course of activity. As a result of being free in the body, these lipids may induce antibody formation. Interfering Factors Alcohol decreases reaction intensity in tests and therefore should be avoided for a least 24 hrs before blood is drawn. Avoid drawing the blood sample immediately after the patient has eaten. Clinical Information Sexual partners of patients with syphilis should be evaluated for the disease. After treatment, patients with early stage syphilis should be tested at 3 month intervals for one year to monitor declining reactivity of the syphilis. The VDRL Procedure Background The Venereal Disease Research Laboratory (VDRL) test is one of two variations of flocculation procedures used for serological testing of syphilis, the other being the Rapid Plasma Reagin (RPR). Flocculation testing is based on antibody detection with the interaction of soluble antigen with an antibody that results in a precipitate formation of fine particles. Background The VDRL is a confirmatory serological microflocculation slide test used for the detection of syphilis antibodies. In a VDRL procedure, the patient’s serum is heat-inactivated and mixed with a buffered saline suspension of VDRL Antigen containing cardiolipin, lecithin and cholesterol that binds with Reagin, an antibody-like protein. A combination of Reagin and VDRL Antigen form microscopic clumping called flocculation. Background The VDRL can be used for qualitative and quantitative measurements and is recommended when a patient suspected of having syphilis has a negative dark field microscopy result or when atypical lesions are present. Syphilis is a venereally transmitted disease that has a serious and potentially life threatening sequelae if untreated. VDRL Serological Procedure Principles VDRL Antigen is a nontreponemal antigen composed of cardiolipin cholesterol and lecithin. The nontreponemal tests measures anti-lipid antibodies, which are formed by the host in response to lipids released from damaged host cells early in infection with T. pallidum, and lipidlike material form the treponemal cell surface. During syphilis infection, an antibody-like substance called reagin can be detected in the patient’s serum or CSF. Procedural Principles Reactive nontreponemal tests confirm the diagnosis in the presence of early or late lesion syphilis and offer a clue in latent subclinical syphilis. It is also an effective tool for detecting cases in epidemiologic investigations and are superior to the treponemal test for following the response to therapy. Procedural Principles Nontreponemal antigen tests are not entirely specific for syphilis and do not have satisfactory sensitivity in all stages of syphilis. Whenever the results of a nontreponemal antigen test disagree with the clinical impression, a treponemal antigen test such as the FTA-ABS should be performed. Quality Assurance Prepare a fresh antigen suspension each testing day. Once prepared, it should be used within 8 hours. Store prepared suspension at 23-29)C. Test antigen suspension reactivity with control sera (Reactive, Weakly reactive and Nonreactive). Test serum dilutions within 1 hour after heat inactivation. Use antigen suspension only if it produces the expected reactivity with the control sera comparable to results obtained with the reference antigen. Required Materials VDRL Antigen with buffered saline solution containing 1% sodium chloride, pH 6.0+/-0.1 with 0.05% formaldehyde preservative Reactive, weakly reactive and nonreactive serum 0.9% saline, non-disposable 1cc glass syringe and calibrated needles without bevel-18 gauge(serum) or 21-22 gauge(CSF), slide cards(serum) or concavity slides(CSF) Stirrers Rotator Specimen Collection and Preparation for Serum Collect 5-8 ml of blood by aseptic venipuncture in a red top tube. Allow blood to clot at room temperature then centrifuge to obtain serum. Heat the test sera at 560C for 30 minutes. Specimen must be at 23-290C when tested. Specimen must be clear of hemolysis and show no visible evidence of bacteria contamination. Store at room temperature for 4 hours, after which store at 2-80C, maybe refrigerated up to 5 days, then frozen at <200C. Specimen Collection and Preparation for CSF Centrifuge and decant the specimen Specimens do not require heat inactivation before testing. Spinal fluids that are visibly contaminated or that contain gross blood are unsatisfactory Antigen Suspension Preparation Pipette 0.4ml of VDRL buffered saline to the bottom of a round 30 ml glass stoppered bottle with a flat inner-bottom surface. Gently tilt bottle so that VDRL buffered saline will cover the entire inner-bottom surface of the bottle. Add 0.5 ml of VDRL Antigen directly into the saline while continuously but gently rotating the bottle on a flat surface from the lower half of a 1.0 ml pipette graduated cylinder to the tip. Add antigen drop by drop at a rate that allows about 6 sec for 0.5 ml of antigen. Keep pipette tip in the upper third of the bottle and do not splash saline unto the pipette. Antigen Suspension Preparation Expel the last drop of antigen without touching pipette to the saline and continue rotation of the bottle for 10 sec. Add 4.1 ml of buffered saline from a 5 ml pipette. Do not drop saline directly on antigen; allow it to flow down the side of the bottle. Cap the bottle and mix by gentle inversion. Allow to stand for 5 minutes but no more than 2 hours. The suspension is ready for use. Remix suspension by swirling only Antigen Suspension Mix by gentle inversion. Allow to stand at least 5 minutes but no more than 2 hours. Procedure: Step 1 Wells should be labeled R, WR, NR, and PS for reactive, weakly reactive, and nonreactive, respectively. Procedure: Step 2 Pipette .05ml of specimen into one concavity of an agglutination slide. Procedure: Step 3 Add one drop (.01 ml) of sensitized antigen suspension to each specimen with a 21 or 22 gauge needle. Procedure: Step 4 Rotate slides for 8 minutes on a mechanical rotator at 180 rpm. Note: when the tests are performed in a dry climate, the slides may be covered with a box lid to prevent evaporation. Step 5a for Positive CSF Samples Quantitative tests are run on all spinal fluids found to be reactive in the qualitative test. Prepare fluid as follows: A. Pipette 0.2 ml of 0.9% saline into each of 5 or more tubes. Step 5b for Positive CSF Samples Add 0.2ml of unheated spinal fluid to tube 1, mix well and transfer 0.2 ml to tube 2 . Step 5c for Positive CSF Samples Continue mixing and transferring 0.2 ml from one tube to the next until the last tube is reached. The respective dilutions are 1:2, 1:4, 1:8, 1:16. Etc., Step 5: for Positive CSF Samples 2. Test each spinal fluid dilution and undiluted spinal fluid as described under “VDRL slide qualitative on spinal fluid.” 3. Report results in terms of the greatest spinal fluid dilution (dils) that produces a reactive result. Reading Slide Results Results for Serum Specimen Qualitative Testing - Medium to large clumps (Reactive); Small clumps (Weakly Reactive); No clumping or very slight roughness (Nonreactive). Verify control sera results for expectation. If reactions are not as expected, the test is invalid and results can not be reported. Perform a quantitative test to endpoint on all serum samples that produce reactive, weakly reactive or “rough” nonreactive results in the qualitative slide test. Results for Serum Specimen Quantitative Testing - Report the titer as the highest dilution that produces a Reactive (not weakly reactive) results Results for CSF Specimen Qualitative Testing - No clumping or very slight roughness (Nonreactive); Definite clumps (Reactive) A quantitative test should be performed on any reactive specimen. Quantitative Testing - Report the titer in terms of the highest dilution that produces a reactive (not weakly reactive) result. Interpretation Results of the serum VDRL Test must be confirmed by a treponemal test. Diagnosis depends upon results of VDRL, treponemal confirmatory test, clinical signs and symptoms and risk factor. Reactive VDRL - may indicate past or present infection with microorganism or false positive. A false positive is determined if the confirmatory treponemal test is negative Interpretation Nonreactive VDRL - with clinical evidence may indicate early primary syphilis, a prozone reaction in secondary or late syphilis. Nonreactive VDRL - with no clinical evidence may indicate no current infection or an effectively treated infection. Quantitative VDRL - detects changes in reagin titer. Serum samples displaying a fourfold increase in titer on a repeated sample may indicate an infection, reinfection or treatment failure. A fourfold decrease during treatment indicates adequate therapy. Sources of Error False positive reactions - occur in 10% to 30% of positive serological tests for syphilis and consist of nonsyphilitic positive VDRL. reactions with cardiolipin type antigens. False negative reactions - consist of conditions and a variety of situations. Weakly reactive - caused by very early infection, lessening of the activity of the disease after treatment and improper technique or questionable reagents. False Positive Reactions Lupus erythematosus Rheumatic fever Vaccinia and virus pneumonia Pneumococcal pneumonia Infectious mononucleosis Infectious hepatitis Leprosy Malaria Rheumatoid arthritis Pregnancy Aging individuals False Negative Reactions Technical error - unsatisfactory antigen or technique. Low antibody titers Presence of inhibitors in the patient’s serum Reduced ambient temperature (below 230 to 290) Prozone reaction References Wasley G.D. (1988). Syphilis serology. Oxford press, New York. Abbot laboratories, Abbott Park, IL 60064. Center for disease control (1999). Guidelines for evaluation and acceptance of new syphilis serology tests for routine use. US department of health, education and welfare publication, Atlanta. Photos Thomas B. Wiggers, Associate Professor Clinical Laboratory Sciences, UMMC Additional photos:www.Kumc.EDU