ETHICS IN RESEARCH - University of Windsor
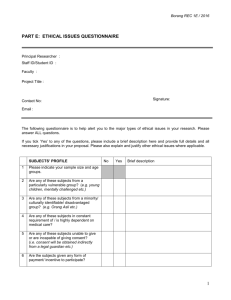
advertisement
ETHICS IN RESEARCH Professor Lisa High University of Windsor Why Ethical Guidelines? Face many ethical dilemmas in practice Vulnerable participants or patients or clients To protect people receiving health care and the interventions and treatment regimes in the system To protect the public from harm Historical Events Need to discuss “unethical studies” – led to the development of Ethical Codes and Regulations Nazi Medical Experiments Tuskegee Syphilis Study Willowbrook Study Jewish Chronic Disease Hospital Study Nazi Medical Experiments 1933 to 1945 – unethical activities implemented by the Third Reich in Europe Programs included: Sterilization Euthanasia numerous experiments to produce a pop’n of pure Germans & Aryans Tuskegee Syphilis Study 1932 – US Public Health Service initiated a study of syphilis in black men in the small rural town of Tuskegee, Alabama Cont’d for 40 years (to1962) To determine the course of syphilis in the adult black male 2 groups: n = 400 untreated syphilis (treatment group) n = 200 without syphilis (control group) Consent – participants not informed about the purpose and procedures Deliberate steps to keep subjects from receiving treatment No effort to stop the study Willowbrook Study mid 1950’s to early 1970’s – research on hepatitis at an institution for the mentally retarded Subjects – children – deliberately infected with Hepatitis virus 20 year study – closed Research cont’d – to new admits Parents were forced to give permission for their child in order to gain their child’s admission to the institution Published findings Investigators denied vs. acquired while in the institution Cont’d into the early 70’s Jewish Chronic Disease Hospital Study In 1960’s – purpose to determine the patients’ rejection responses to live cancer cells N = 22 – injected with a suspension containing live cancer cells that had been generated from human cancer tissue Rights of patients not protected, not informed, study was never presented to the research committee of the Jewish Hospital What Happened? NUMERBURG CODE DECLARATTION OF HELSINKI CODE OF ETHICS Nuremburg Code 1st internationally recognized set of ethical standards Developed post-Nazi atrocities were made public during the Nuremburg trials Declaration of Helsinki Provided: (a) Greater care should be exercised to protect subjects from harm in non-therapeutic research (b) Strong, independent justification is required for exposing a healthy volunteer to substantial risk of harm just to gain new scientific info (c) The investigator must protect the life and health of the research subject - 1964 – World Medical Assembly Code of Ethics Most disciplines have established - Canadian Nurses Association (1983) - “Ethical Guidelines for Nurses in Research Involving Human Participants” - 2002 guidelines revised - Health Canada – “Tri County Policy Statement: Ethical Conduct for Research Involving Humans” - Joint – MRC (Medical Research Canada), NSERC and SSHRC - Eight guiding principles of ethics - Research Ethic Review Board (REB) Ethical Guidelines - Principle of Respect for Human Dignity cardinal rule Right to self determination and right for full disclosure Humans are autonomous agents capable of controlling their own activities Principle of Respect For Human Dignity Right to Self-Determination and Right to Full Disclosure Is based on the principle of respect Humans capable of self-determination & controlling their own destiny Autonomy – voluntarily participate & withdrawal no coercion full disclosure no deception voluntary consent Persons with diminished autonomy: who? Principle of Respect For Human Dignity Free and Informed Consent Informed consent – participants have adequate information comprehend the research power of free choice enable voluntary participation Consent Forms – what should a consent include? Implied Consent – define? Process Consent – what does that mean? Issues Relating to the Principle of Respect Full Disclosure: 2 biases (1) Bias resulting from distorted information (2) Bias resulting from failure to recruit a good sample Techniques used: (1) Covert data collection/concealment (2) Deception (both problematic from an ethical standpoint – why?) Issues Relating to the Principle of Respect Vulnerable Populations Define: Examples: Principle of Respect for Privacy and Confidentiality Right to Privacy and the Right to Confidentiality The right an individual has to determine the time, extent, and general circumstances under which private information will be shared with or withheld from others Invasion of privacy – occurs when – private information is shared without an individuals knowledge or against his/her will Principle of Respect for Privacy and Confidentiality Anonymity – exists only if the subjects identity cannot be linked even by the researcher Based on the right to privacy, subject has the right to anonymity and the right to assume that the data collected will be kept confidential Confidentiality – is the researcher’s management of private information shared by the subject Identification numbers Principle of Respect for Justice and Inclusiveness Justice – fairness and equity Ethics review process have fair methods, standards, and procedures Distributive justice – no one within the pop’s should be unfairly burdened with the demands of the research Fair Treatment includes – see list on page 83 Principle of Balancing Harms and Benefits Based on the principle of beneficence One should do good and above all do no harm Freedom from harm, freedom from exploitation, risk-benefit ratio Risk-benefit ratio: consider how comfortable you would feel having family members participate in the study Would be comfortable Benefit to society and the nursing profession Maximizing Benefits & Minimizing Harms Principle of “Beneficence” – imposes a duty to benefit others and in research ethics a duty to maximize benefits To produce benefits to society as a whole, subjects themselves, other individuals in society, advancement of knowledge Principle of “Nonmaleficence” – the duty to avoid, prevent, or minimize harm to others Participants not subject to unecessary risks of harms – terminate, no consequences if the participant withdraws Debriefing sessions can be used Freedom from exploitation Guidelines to Critiquing the Ethical Aspect of a Study Review Box – 4-2 on page 88 (1st edition) Review Box – 5-2 on page 103 (2nd edition)