Teratogens and Developmental Influences

Teratogens and Other
Influences on Development
Scenario
You return after class one day to find a message in your voice mail from your cousin’s husband, who is obviously upset. He has called to tell you that your cousin, Karen has just given birth more than 2 months early to a little boy who weighs slightly less than 4 pounds.
Karen’s pregnancy had been planned and completely normal and she had followed her doctor’s advice to the letter, so this outcome comes as a complete shock. The baby has been moved to the neonatal intensive care unit.
You’re very close to Karen and know that she will want to see you as soon as possible.
When you visit her in the hospital, Karen tells you that the baby is in stable condition but that she’s deeply worried about what the future holds for him and for the family. She shares her fear that he will never have a normal life.
From what you’ve learned about pre-natal development in your child development class, what can you tell Karen about her new son’s chances for normal development? If she asks for your advice, what would you tell her?
Teratogens and Other
Influences on Development
Pregnancy and Alcohol
Terminology
Teratogen: any environmental agent that causes damage to the fetus during prenatal period.
– viruses, drugs, chemicals, and radiation
– others categories?
Terminology
95% of all newborns are born without problematic developments.
Of the remaining 5%,
– 3% have mild, temporary or reversible defects.
– only 2% having continuing effects.
Effect- What happens- the developmental outcome or consequence of exposure to a teratogen
– variation in the development of the embryo, fetus, or child.
Mechanism- How it happens- the physiological or biological processes that explains the cause or how specific events occur
Terminology
Sensitive Period- That broad period of time when, if an insult occurs, there are likely to be consequences.
– insults may occur over a broad period of time or in a number of ways e.g., the neurobehavioral effects due to exposure of alcohol during last trimester
Critical Period- A specific period of time during which, if an insult occurs, a particular consequence will happen
– Malformation of ears due to thalidomide exposure on days 34-38 of PND.
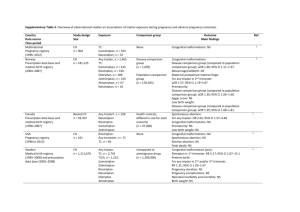
Characteristics and Effects of Teratogens
Time of exposure
– Worst effects= period when a body part or organ system is developing.
– When is this?
Susceptibility to harm varies
– Not all embryos or fetuses are affected in the same way by the same exposure.
Characteristics of the fetus influence the effects
Studies with identical twins frequently show that one twin has impairment from a teratogen while the other doesn’t.
Research on FAS shows that ½ ounce/day can cause neurobehavioral problems in some children, while some children born to alcoholic mothers don’t get FAS
Characteristics and Effects of Teratogens
Different teratogens can cause the same defect (equifinality)
– For example: ADHD may be caused by chronic stress experienced by the mother during pregnancy exposure to drugs during pregnancy exposure to alcohol during pregnancy
Characteristics and Effects of Teratogens
Single teratogen may cause more than 1 defect (multifinality)
– Rubella may cause blindness, deafness, and mental impairments
– Exposure to alcohol may cause physical malformations, growth retardation, and mental retardation.
Characteristics and Effects of Teratogens
Dose Response (more is worse than less)
– FAS- Fetal Alcohol Syndrome
Associated with heavy drinking throughout pregnancy
Results- much more severe: physical malformations, major mental retardation
– FAE- Fetal Alcohol Effects
Associated with binge drinking, or occasional drinking- Not as heavy, not as often
Results: Behavioral/emotional effects
Characteristics and Effects of Teratogens
Father’s exposure to teratogens also increases risk
WHY??????
– Because sperm take 72 hours to mature and during this period the sperm are susceptible to malformations due to environmental exposures
– Tetracycline (discolors the enamel of the infant’s teeth).
Typically associated with mom, but it is also true if dad takes it.
Characteristics and Effects of Teratogens
Long-term outcomes can be mediated by postnatal experience
– “Effect” may be a susceptibility
– Long term high quality care and enriched environment helps OVERCOME or minimize bad start
– HIV Babies with parents who were drug and alcohol users did better than non. WHY??
The Specifics
Diseases
Rubella-German Measles“Timing” is key
– 1st Trimester is likely to cause more serious impairments
Heart defects1st 8 weeks (germinal/embryonic)
Cataracts“ “
Deafness- last half of 1st trimester
– Risk of having impairments (as well as the severity of them) decreases with time-
60-85% have impairments if exposed in the first 8 weeks
50% if exposed in the 3rd month
16% if exposed in the 2nd trimester
– 2nd Trimester
Minor mental deficiencies
Motor impairments hearing impairment
Diseases
Toxoplasmosis –Beware of the household pet!!!
– 1st trimester
Severe CNS damage
Damage to the eyes and visual system
– Later trimesters increased miscarriage jaundice- problem with liver functioning- used to be major cause of MR pneumonia- inflammation of the lungs myocarditis
STDs
Syphilis (treatment matters!!!)
– 1st and 2nd trimester (<18 weeks) No effect if treatment clears infection.
– Why?
The organism cannot cross the placenta < 18 weeks
– 2nd and 3rd trimester (>18 weeks)- impairs organs after they develop
Lesions of the eyes, optic nerve atrophy
Problems with the liver functioning
Bone malformations
Heart malformations
– If present at birth, CNS impairment and gastrointestinal tract problems
STDs (read on own)
Chlamydia (timing doesn’t seem to matter)
– Infected mothers are more likely to miscarry or have stillborn infants
– If the disease is transmitted to the infant at birth, results in pneumonia and/or conjunctivitisBoth “easily” treated
STDs(read on own)
Genital Herpes (23% of all adults have HSV 2, only
1/10 know they have it)
– 700,000 new cases each year
– >350,000 new cases are women each year
– 80,500 women who are pregnant each year have new cases of HSV
– 1/15,000 births- neonatal HSV infection
– infected infants (EFFECTS):
1/3 of infants die
1/3 have permanent & moderate to severe brain damage
1/3 have mild impairments including liver probs, cns impairment, respiratory function
– C-Section is recommended if infection is known pre-birth
HIV (read in your text, p. 99)
HIV
– Can be latent for years (10-15 if you are in otherwise good shape)
– Transmitted from mother to fetus either prenatally, at birth, or through the mothers milk (postnatally)
– 30% of pregnant women with HIV have babies who become infected.
– 8% transmission when mother uses AZT treatment during pregnancy and for the infant after birth
– In twin studies where a vaginal delivery occurs, the first infant is 5X more likely to become infected-
Why?
– Cesarean section is recommended
Hormones
Oral Contraceptives
– Cardiovascular problems
– 3-6 months off BEFORE pregnancy- Longer if you’ve been on the pill for a long time
Depo Provera
– 6-18mo
– Bone loss
Medications
DES (dielthystilbestrol)- Used to prevent miscarriages and premature deliveries
If prenatal exposure:
– Increased risk of cervical cancer in daughters- can be born with no uterus or fallopian tubes
– Increased risk of fetal feminization (one testicle, recessed testes) or hypospadias
– Higher rate of reproductive problems for both sons and daughters
Medications
– Thalidomide- drug used to stop morning sickness
Not pre-tested on pregnant humans
34-38 days malformations of the ears
38-46 days- malformations of the arms
40-46 days- malformations of the legs
Direction of development?
/
\
Good ex of cephal
Environmental Teratogens
What are they?
Methyl mercury- Pollutant found in fish
(very high quantities in some areas of
Japan, Puget Sound???)
– Increased birth weight C-Sections
– Neurobehavioral effects (ADD, ADHD,
Learning disorder)
Environmental Teratogens
Lead Poisoning- found in old paint and water pipes
– Anemia- treatable
– Encephalopathy- abnormal development of the brain & MR
– Young children and infants who are lead poisoned can get MR-Method of ingestion?
Social Drugs
Alcohol- 43% of alcoholic mothers have FAS kids
(other 57% have FAE)
– Full blown FAS: early exposure (specifically days 19-23)- results in facial dysmorphology- Diagnostic criteria
– wide set eyes (small eyes)
– thin upper lip
– flat filtrum repeated exposure, throughout pregnancy (early/late)
– microencephaly
– mental retardation (mild to severe)
– growth retardation (<10% on growth charts)
Late exposure (last trimester)
–
Decreased birth weight
–
Hyperactivity
– Emotional lability (inability to control emotions/lots of emotional outbursts)
FAS
Social Drugs- Alcohol
MECHANISM- How does it work?
– Mom’s ability to metabolize alcohol is reduced during pregnancy- decreases as pregnancy advances
– breakdown of alcohol uses extra oxygen- reduces the amount that is available to the developing organism
– Alcohol can cross the placenta which impairs embryonic and fetal development
– Fetus’s ability to metabolize alcohol is 50% of mom’s (so alcohol remains longer at the end of pregnancy)
Video- FAE
Social Drugs
Smoking (nicotine)
– Effects
Decreased birthweight
Decreased heart rate increased spontaneous abortions increased perinatal mortality increased hyperactivity, ADHD, ADD
Patch??
– Mechanism reduced oxygen available to the developing fetus-different ways
Increased heart rate and blood pressure
Social Drugs
Caffeine-
– Not as much known. Studies have conflicting results.
– Increases heart rate
– Increases blood pressure
– Constricts blood vessels
– Dehydrates, so probably reduces the oxygen supply
Illegal Drugs
Marijuana- small numbers of studies-
WHY?????
– Moms who smoke during pregnancy
Attention may be impaired babies are smaller
– Moms who smoke during pregnancy: have better parent-infant relationship at 1 month of age have calmer babies
Have better social interactions with the infant
– Problem with the internal validity. Why??
Self-selected group may have more “relaxed” view of the world, so therefore have more “lax” relationship with the child
Illegal Drugs
Cocaine
– Effects:
Decreased gestational age
Increased low birth weight
Placental abruption
Increased rates of birth defects- Malformations of the heart, CNS, gastrointestinal tract
Increased hyperactivity, ADD at school age.
– Mechanism?
reduced oxygen supply
– Study with 300 exposed & 300 non-exposed, controlling for SES found that Low SES had a greater effect on the infant development than cocaine.
Low B-W and Pre-term- Premature
Low birth weight and pre-term birth
– Low birth weight= < 2500g or 5.5 lbs
– Pre-term birth = < 35 weeks (post conception)- Not necessarily bad
– Small for date
– Influences on the size of the infant
Mother’s ht, wt
Mother’s age
Mother’s weight at birth
Environmental variables (teratogens?)
Nutrition
Birth order
Gestational weight, Birth weight, and Survival
Low Birth weight & survival
Weight at birth
1
– 1 ½ lbs
1 ¾ - 2 lbs
2 ¼ - 3 lbs
3
– 3 ½ lbs
>5 ½ lbs
% survival
33%
67%
84%
91%
98%
Pre-term birth & survival to 1 year
Gestational age @ birth
<24 weeks
24-25 weeks
26-29 weeks
30-32 weeks
33-36 weeks
37-40 weeks
41+ weeks
35%
63%
86%
93%
98%
99.3%
99.4 %
Birth weight
Babies BW
14 40
Maternal Age (in years)
<14 or >40, increased risk