Chapter 24 - wcunurs207and217
advertisement

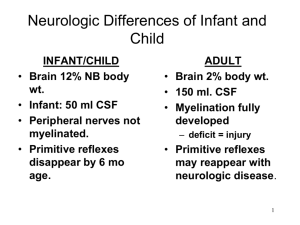
ALTERATIONS IN NEUROLOGICAL FUNCTION IN PEDIATRICS CH 29 Christine Limann Dyer, RN, MSN, CPN Pediatric Differences -Head is larger in proportion to body -Insufficient musculoskeletal support in neck -Fontenelles not closed in young child A & P Review Nervous system Central Brain nervous system and spinal cord Peripheral nervous system Sensory-somatic Autonomic Altered States of Consciousness Arousal or level of consciousness: awareness of the environment Content of thought: all cognitive functions that ensure awareness of affective states, self, and environment The Unconscious Child Unconsciousness is a state in which a child’s cerebral function is depressed and ranges from stupor to coma Caring for the Unconscious Child Evaluating neurological status The pediatric Glascow Coma Scale Eye opening, verbal response, and motor response Caring for the Unconscious Child Monitor vital signs Manage the airway Manage bladder and bowel elimination Maintain hydration & nutrition Provide proper hygiene Position and perform exercise Persistent Vegetative State A complete unawareness of the environment accompanied by sleep–wake cycles. The diagnosis is established if it is present for 1 month after acute or nontraumatic brain injury or has lasted for 1 month in children with degenerative or metabolic disorders or developmental malformations Family support is needed Increased Intracranial Pressure Intracranial pressure (ICP) is the pressure of the cerebral spinal fluid (CSF) in the subarachnoid space between the skull and the brain. A child can have increased ICP as a result of many internal or external factors. Signs and symptoms See Table 29-2 Increased Intracranial Pressure Nursing care Close monitoring (neurologic status) Maintenance of a patent airway Monitor vital signs closely (hyperthermia) Administer IV fluids Monitor fluid balance (I & O) Protect child from injury Administer antiseizure medications Provide emotional support Administer medications to decrease cerebral edema Analgesia and sedation A craniotomy is recommended when all other measures have been unsuccessful Cushing’s Triad Increased Systolic Widening Pulse Pressure Decreased Diastolic Irregular Respirations Bradycardia (Ball, Bindler, & Cowen, 2010) Seizures Most common neurologic dysfunction in kids Caused by malfunctions of brain’s electrical system Infections or high fever Chemical imbalance of the body that causes loss of metabolism Congenital conditions or trauma Genetic factors and family history Brain tumors and neurological problems Habits of the mother like smoking, alcohol consumption, drugs and certain medications (Hockenbery & Wilson, 2010) Types of Seizures Absence – (3-12 years old)5-10 sec. Lip smacking, staring, twitching, brief loss of consciousness Partial (focal) – Less than 30 sec., one extremity Generalized (tonic-clonic or grand mal) Febrile Dependent Epilepsy – Chronic disorder Febrile Seizures Usually higher than 38.9 C or 101F Usually short in duration. Instruct parents to call 911 if longer than 5 minutes Use antipyretics and cooling measures (Mayoclinic.com, 2010) Nursing actions with patients with seizures Before During Where there triggers such as change in temperature, light? Maintain airway Role to side if possible Time changes started Part of the body involved and movement Incontinence After Do they remember what happened? (Ball, Bindler, & Cowen, 2010) Treatment for Seizures Common pharmacological choices Ativan -Lorazepan Diazepam – Diastat (can be given rectally) Phenobarbital or Phenytoin Remind parents not to stop once the seizures are controlled until directed by a doctor. Other types of treatment Vagal Nerve stimulator Ketogenic Diet (Ball, Bindler, & Cowen, 2010) Seizure Disorders Signs and symptoms See Table 29-3 Nursing care Complete a detailed history Ensure airway management Maintain anticonvulsant therapy Implement seizure precautions (padded side rails, oxygen, suction equipment, IV access, and anticonvulsant medications) Provide continuous cardiac, respiratory, and oxygen monitoring Instruct caregivers instructed in CPR Keep school nurses and teachers informed about the condition Encourage medical alert identification bracelet INFLAMMATORY NEUROLOGICAL CONDITIONS Intracranial Infections -Meningitis Bacterial Meningitis More Dangerous Group B Streptococcus and gramnegative enteric bacilli most likely cause in newborns Neisseria Meningitidis 2 mo-12 yr Viral Meningitis Can also cause meningococcemia H influenzae B and Strep Pneumoniae are now less common because of vaccination Does not appear as ill as the child with bacterial meningitis Caused by enteroviruses, mumps, vericella Irritable, fever, lethargy, headache, may have stick neck or back pain Usually resolves in 3-10 days Treat with antibiotics until bacterial meningitis is ruled out -Fever, vomiting, irritable, hemorrhagic rash, headache, nuchal rigidity, seizures, Kernig and/or Brudzinski sign Treatment: Antibiotics Both Diagnosed by Lumbar Puncture-LP Encephalitis Signs and symptoms Disorientation, confusion, headache, high fever, photophobia, lethargy, aphasia, hallucinations, seizures, nuchal rigidity, and coma Nursing care Viral is treated with antiviral medication Bacterial is treated with a narrowspectrum antibiotic Other medications include antipyretics, anticonvulsants, analgesics, and antiinflammatories Provide intravenous fluids and nutrition Implement seizure precautions Monitor fluid & balance Do not suction or give percussion Brain Abscess Signs and symptoms Localized headache, fever, drowsiness, stupor, confusion, general or focal seizures, focal motor or sensory impairments, ataxia, nausea and vomiting, papilledema, and hemiparesis Nursing care Assess neurological status, assess response to treatment, administer medications, and provide supportive care Monitor serum labs Surgery required if no response to antimicrobial therapy (postoperative care) or does not meet criteria for medical therapy Reye Syndrome Associated with use of aspirin with viral illness such as chicken pox or influenza b May cause permanent tissue damage to brain and liver Signs and symptoms Lethargy, vomiting, drowsiness, liver dysfunction Nursing care Conduct neurological assessment Administer IV fluids Administer corticosteroids and/or diuretics Monitor oxygen saturation (supplemental oxygen) Insert arterial line (blood gases) Take seizure precautions Limit invasive procedures Provide emotional support Guillain-Barré Syndrome Signs and symptoms Three phases: acute, second, recovery Nursing care Plasma exchange and IV immunoglobulin therapy Give corticosteroids Monitor progression Insert indwelling urinary catheter Assess pain level Prevent contractures and loss of function (passive ROM) Provide skin care Suggest age-appropriate activities DEVELOPMENTAL NEUROLOGICAL CONDITIONS Spina Bifida Neural tube defects (NTDs) Signs and symptoms Vary depending on the level of the lesion and defect Spina bifida occulta Meningocele Myelomeningocele Types Meningocele Myelomeningocele Spina bifida occulta Spina Bifida Nursing care Place newborn in prone position (prevent injury to sack) Provide postoperative care for laminectomy & closure of defect Evaluate orthopedic function Prevent joint contractures Assess bladder and bowel function Provide skin care Assess neurological status Measure head circumference and assess fontanel Manage pain Spina Bifida Surgery to close the repair usually occurs within 24-48 hours. Some cases can be repaired in utero. May need VP shunt. Ongoing therapy Mobility-Braces, wheelchair Neurogenic bowel and bladder Hydrocephalus – Cerebrospinal fluid build up Communicating hydrocephalus – no blockage. Either a problem with over production of CSF or problem with absorption Non-communicating- obstruction Aqueduct of sylvius Hydrocephalus- clinical manifestations Newborns and infants Bulging fontanels Increased head circumference Sun set eyes Irritability High-pitched, catlike cry Visible scalp veins Children Headache Visual disturbance Nausea/vomiting Pupils sluggish Decrease in consciousness Seizures Cushing’s Triad Widening pulse pressure Bradycardia Irregular respirations (Ball, Bindler, & Cowen, 2010) Hydrocephalus Treatment Ventriculoperitoneal shunt (VP Shunt) Hydrocephalus Signs and symptoms Increased ICP Macewen sign Nursing care Understand shunt function and complications Obtain history and physical (life-threatening conditions) Discuss pharmacological measures or surgical procedure Perform nursing actions related to ICP Measure head circumference Give preoperative and postoperative antibiotics Assess neurological status Assess for shunt malfunction (eye assessment) Assess abdominal status (pain, bowel sounds, and circumference) Elevate HOB 30° Abnormal muscle tone, lack of coordination, spasticity. Symptoms very depending on age and type of CNS injury. Cerebral Palsy Nursing Role: Provide adequate Nutrition Maintain Skin Integrity Promote safety and physical mobility Prevent Constipation (Ball, Bindler, & Cowen, 2010) Cerebral Palsy Signs and symptoms Vary individually depending on the area of the brain involved and the extent of damage Four categories Spastic Ataxic Athetoid or dyskinetic Mixed Cerebral Palsy Nursing care Use splints and braces Promote self-care Administer medications (reduce muscle spasms, spasticity, anxiety, and seizure) Surgery (selective dorsal rhizotomy) Address feeding problems Provide intellectual stimulation Ensure safe environment NEUROLOGICAL INJURIES Drowning/Near-Drowning Drowning is the second leading cause of accidental death in children Death occurs from asphyxia while submerged Can occur with even small quantity of water (even as little as a pail of water) Near-drowning: survived at least 24 hours after submersion Near Drowning (Submersion) Signs and symptoms Cerebral edema, alteration in LOC, respiratory distress, cardiovascular complications, hypovolema Nursing care Assess and maintain airway Provide life support measures Suction secretions Insert NG tube Administer oxygen Assess other injures (head or spinal trauma) Head Injuries -Major cause of childhood deaths -Who is more at risk? Head Injury Traumatic Brain Injury (TBI) Signs and symptoms Obvious signs: blood on the scalp, depression of the skull, and an obvious penetrating wound Other signs and symptoms: loss of consciousness, alteration LOC, seizures and combativeness Nursing care Provide immediate care to prevent life-threatening complications Maintain airway patency and oxygen administration Insert IV and administer hypertonic fluid Assess neurological status Assess ICP Concussion Signs and Symptoms -Headache -Slowness in thinking, acting, speaking -Fatigue -Memory problems -Loss of balance (Ball, Bindler, & Cowen, 2010) Cerebral Contusion Bruising of the brain secondary to blunt trauma. Can be either coup or countercoup injuries. May involve tearing of brain tissue and may lead to areas of necrosis or infarction. (Ball, Bindler, & Cowen, 2010) Head Trauma Subdural Hematoma Between dura and cerebellum Result of head trauma such as falls, MVA, or shaken child syndrome Symptoms may appear after 24-72 hours Change in LOC, Headache, N/V, retinal hemorrhage, pupil on side of injury may be dilated Prognosis poor Epidural Hematoma Between dura and skull Almost never occurs in children less than 4 y/o. Blunt trauma such as MVA, assault, baseball injury Delayed onset followed by rapid change in mental status Headache, Fixed dialated pupils, s/s increased ICP Prognosis good Shaken Baby Countercoup injury Physical abuse Countercoup injury Subdural Hematoma Retinal Hemorrhage Seizure Check baby for fractures in the rest of their body Shaken Baby Syndrome Signs and symptoms Seizure activity, apnea, budging fontanels, coma, hemorrhage, bradycardia & cardiovascular collapse Nursing care Provide respiratory and cardiovascular support Assess for ICP Insert NG tube Maintain seizure precautions Maintain adequate fluid and nutritional intake Assess and document visible injuries Discuss short- or long-term care Assess parental concerns Spinal Cord Injury Signs and symptoms Numbness, tingling, or loss of function Nursing care Maintain airway management and respiratory function Provide cardiovascular and circulatory support Give steroid therapy Monitor fluid intake and output Maintain gastrointestinal function Provide nutritional support Provide emotional and social support Be attuned to an adolescent’s unique needs Explain lifelong care and support, circulation support, disability identification, and exposure of known and unknown physical limitations NONTRAUMATIC NEUROLOGICAL CONDITIONS Headaches Types Primary headaches Secondary headaches Tension Migraine Cluster Headaches Signs and symptoms Primary (triggers — i.e., stress) Secondary (organic disorder — i.e., trauma) Subtypes (tension, migraine, cluster) Nursing care Provide pharmacologic and nonpharmacologic care Discuss prophylactic measures Give intramuscular or intranasal medications Promote rest and stress reduction strategies SENSORY CONDITIONS Eye Disorders Hyperopia (farsightedness) Myopia (nearsightedness) Correction Concave lenses or contact lenses Laser assisted surgery Astigmatism Irregular curvature or uneven contour of the eye Correction Corrective lenses Surgery Complaints of headache, blurry vision, or dizziness; ophthalmologist referral Amblyopia –lazy eye Signs and symptoms Strabismus or anisometropia are the most common causes Correction Occlusion therapy (patching of the normal eye) is done to restore strength and function of the “lazy eye” Strabismus Nonparallelism in the different fields of gaze causing visual lines to cross even when focused on the same object Correction Ocular patching of the stronger eye, glasses, and pharmacotherapy Early identification and recognition Color Blindness X-linked recessive inheritable color vision deficiency Color blindness is detected using colored charts called the Ishihara Test plates Child can learn to compensate with support from family members, teachers, and friends Nystagmus Rapid irregular involuntary eye movement caused by a disorder of the central nervous system Correction Extraocular surgery Cataracts Signs and symptoms Excessive tearing, extraocular movements, photophobia, lens appears cloudy, or there is a white or dulled red reflex Correction Prevent loss of visual acuity Laser procedure Postoperative (monitor nausea, emesis, pain, hemorrhage and signs of infection) Postoperative eye drops Follow-up care for visual acuity Educate family Early identification and recognition Glaucoma Increase in IOP leads to retinal and optic nerve damage Signs and symptoms Bupthalmos (enlarged eye globe), epiphora (excessive tearing), and photophobia (sensitivity to light) Correction Preoperative maintain quiet environment Antiglaucoma medications Analgesia and anxiety reduction strategies Pre- and postoperative care (teach parents) Retinoblastoma Signs and symptoms Absence or abnormality of the red reflex A whitish or yellow color of the pupil called leukocoria Correction Laser, radiation, cryotherapy, or enucleation EYE INJURIES Foreign Bodies Penetration Immediate transport to ER for removal Corneal abrasion Treatment Topical antibiotic solutions or ointments, analgesics, eye patch Hyphema Hemorrhage into the anterior chamber of the eye Treatment Rest, possible evacuation Monitor increased intraocular pressure Promote decreased activity HOB 30° Patch both eyes Chemical burns Usually occur as a result of an accident Treatment Rapid eye flushing for 15 to 30 minutes followed by pH analysis of the chemical agent Eye patching HEARING LOSS Hearing Loss Causes 1/3 of all cases are due to genetic causes 1/3 of all cases are due to non-genetic influences 1/3 of all cases are due to unknown causes Hearing Loss Diagnostic testing Universal infant hearing screening before 1 month of age is recommended Treatment Based on underlying pathologic conditions, presence of organic diseases, the severity of hearing loss, the degree of frequency loss, and any CNS abnormalities Amplification aids (hearing aid) Nursing care Provide emotional, educational, and collaborative support for the child and family Language Disorders Communication A process of complex interaction involving the exchange of information, feelings, ideas, and interactions Receptive language Expressive language Nursing care Recognize speech and language developmental delays