Evaluation & Treatment of Temporomandibular Joint Dysfunction

Evaluation & Treatment of
TMD
Presented by:
Christy Dauner, OTR
Laurie Applebee, PT
Susan Vaughn, MS, OTR
Learning Objectives
Identify TMD risk factors and related diagnoses
Differentiate joint and muscle disorders
Understand goals of Occupational Therapy for
TMD
Understand OT treatments for TMD and muscle disorders
Perform assessment and treatment approaches for TMD
Disorders of the TMJ
Myofascial Dysfunction
Internal Derangement
Capsulitis
Subluxation
Arthritis
Risk Factors for TMD
Trauma such as blow to the jaw, whiplash injuries, MVA, dental work, opening the mouth too wide or for too long, prolonged chewing
Oral parafunctional habits such as clenching and bruxism that place continued strain on the masticatory system
Malocclusion causes bite instability or functional interference during chewing that places postural strain on the masticatory system
Stressful life events can trigger parafunctional habits and muscle guarding/tension
Emotional factors such as depression or anxiety decreases the ability to cope with pain and can increase parafunctional habits.
TMJ Evaluation
History & Symptoms (referred pain)
Functional Limitations
Tests, Measures & Palpation
AROM (active/passive incisal opening, lateral excursion, and protrusion)
PROM – scissor stretch
TMJ Noise
Muscle Palpation
Differential Diagnosis
Scissor stretch test: if opens further muscular, if not - internal derangement
Clench test: bite down on tongue depressor for 10 – 15 seconds. Pain on same side – muscle, opposite side – joint
“S” vs. “C” curve with opening
Occupational Therapy
Goals for TMD
Increase ROM to >40mm
Decrease pain
Teach joint protection (decrease parafunctional habits, limited opening)
Improve function (eating, yawning, DDS visit tolerance, oral hygiene, talking, sleep, work)
HEP independence
Neutral posture (head on neck, jaw, scapular position, TUTA)
Myofascial Pain Dysfunction
Most common disorder
Referred muscle pain
Muscle pain aggravated by jaw function or parafunction
HA’s
Tenderness of muscles w/o mechanical symptoms
Loss of motion or painful motion
Myofascial Pain Dysfunction
Caused by an underlying related disorder
– malocclusion, arthritis, internal derangement, poor posture
Education is key! – posture, parafunction, stress management
Often chronic and cyclical
Often a myofascial component with all diagnoses
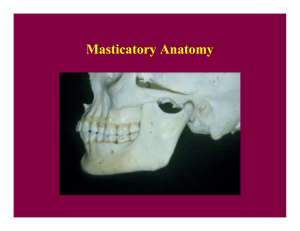
Myofascial Dysfunction
Myofascial contributors may include:
* Lateral pterygoid
* Medial pterygoid
* Temporalis
* Masseter
* Digastrics
* Muscles of the cervical spine
Lateral Pterygoid
Origin: Lateral Pterygoid Plate of Sphenoid
Insertion: Condylar Neck, Ramus of Mandible and Disc
TMJ Muscles – Lateral Pterygoid
#1 myofascial source of pain
Due to attachment to disc it can cause disc and jaw to be unable to return to normal resting position and cause clicking or popping.
Malocclusion of teeth/missing teeth
Referral pattern – zygomatic arch,
TMJ
Medial Pterygoid
Origin: Inner Surface of Lateral Pterygoid Plate
Insertion: Ramus of Mandible by the Angle
TMJ Muscles – Medial Pterygoid
Stuffiness in ear
Swallowing difficulty as restriction in protrusion of jaw
Referral pattern – posterior mandible, mouth, below and behind TMJ including internal ear – not teeth
Temporalis
Origin: Temporal Fascia, Superior to Zygomatic Arch
Insertion: Coronoid Process of Mandible
TMJ Muscles - Temporalis
Significant postural muscle (the only time it isn’t working is when you’re lying supine)
Perpetual clenching
Referral pattern – lower jaw, molar teeth and gum, maxilla, lower portion of mandible, temple eyebrow and external ear
Masseter
Origin: Zygomatic Arch
Insertion: Mandibular Angle and Ramus
TMJ Muscles - Masseter
“Sinusitis”
Referral pattern - temple, along eyebrow, behind eye or upper teeth
Digastrics
Origin: Mastoid Notch (posterior), Symphysis of Mandible
(anterior)
Insertion: Join by a Common Tendon to the Hyoid Bone
TMJ Muscles - Digastrics
Rarely in spasm due to forward head posture (stretch weakness)
Referral pattern – behind mandible toward back of ear, lower incisors
Cervical Spine Muscles
Form stable base for TMJ on which to work
Poor posture – condyle rotates backward – change of biomechanics
Referral pattern from the cervical spine-
Temporal Headaches, SCM
Assess for tension in upper traps, scalenes, and SCM
Parafunctional Behaviors
Gum/candy chewing (chewing limited to 15 – 20 minutes/day!) – including chewing on one side
Clenching/bruxing/grinding
Leaning on chin/jaw
Biting nails, pencils, cheeks
Sleep position
Caffeine use
Musical instruments
Mouth breathing
Phone cradling
Treatment – Myofascial Pain
Dysfunction
Modalities: US - 1.0 – 1.2 w/cm2, 3 MHz, x5 minutes to joint or muscle, heat, electrical stimulation
Manual Therapy – joint mobs/distraction, MFR – including upper cervical region
HEP/Lifestyle changes
Tongue positioning (TUTA)
Self-joint distraction &/or MFR
Eliminating parafunctional behaviors
Postural instruction
Conjunction with splint therapy &/or counseling (Referral to psychology for CBT as needed for stress and anxiety management)
Resting Joint Position
Capsule – anterior/posterior only
Normal Joint Motion
Internal Derangement
Disc Disorder
Internal Derangement
Disc held in place by collateral ligaments and posterior ligament, w/ movement dictated by lateral pterygoid
Click, pop, lock
Pain at joint
“S” shaped opening/closing to reposition jaw
Eye pain
History of trauma
Treatment – Internal Derangement
Modalities: Iontophoresis, electrical stimulation, cold – ice massage
Manual therapy – Joint distraction
Joint protection techniques: Limit motion to no noise, soft food diet or chewing behaviors
Home exercise instruction
Change parafunctional behaviors
Self joint distraction techniques
Tongue positioning for relaxation (TUTA)
Postural instruction and controlled opening/neuromuscular re-education
Treatment - Other
Capsulitis
Usually a result of another disorder unless post surgery
Modalities, MT and HEP
Subluxation
Excess opening (>40 mm)
Usually a component of myofascial pain dysfunction, and treated as this, with addition of stab exercises and controlled opening
Treatment - Other
Arthritis
Generalized joint pain and inflammation
Usually seen in conjunction w/ other Dx
Joint protection, rest
Stretching, therapeutic exercise
Modalities (cold vs. heat, pulsed US, phono/iontophoresis, E-stim)
Intervention: Dentist
Assess occlusion
Parafunctions of clenching/bruxing
Malocclusions
Pressure on back teeth activate temporalis an superior head of lateral pterygoid, anterior teeth activate masseters
Lab - Evaluation
AROM (Therabite)
Active Incisal Opening (Normal 40-60 mm)
Passive Incisal Opening (Normal 42-62 mm)
Lateral Excursion (Normal >7 mm)
Protrusion (Normal > 7 mm)
Lab - Evaluation
TMJ Palpation/Observation
Quality of Motion:
Smooth/Rigid/Jerky/Guarded/Fasciculation/
Thrusting
TMJ Noise: Opening Click, Closing Click,
Reproducible
Visually Assess Opening (S or C Shaped Curve)
Lab
Muscle Palpation
Medial Pterygoid (elevation, protrusion, and lateral deviation to opposite side)
Place index finer on muscle at inside of bottom teeth in mouth. Place opposite thumb under jaw line below ear.
Apply pressure to muscle as if to touch finger and thumb.
Move along gum line until reach incisors in front. Hold until relaxes 1-2X/day
Lateral Pterygoid (elevation, protrusion, and lateral deviation to opposite side)
Place index finger inside mouth, under cheek bone. Point finger up and towards opposite eye. Apply pressure to muscle until it relaxes. To check positioning of finger, actively move jaw in opposite direction and muscle will contract under finger. Hold until relaxes 1-2X/day
Lab
Manual Therapy
Trigger point release
Joint distraction
Place thumb on back, bottom molar and wrap fingers under jaw
Press down as you lift on jaw in scooping motion
Do NOT pull jaw forward
Thank You
Feel free to contact Christy at 952-908-2567 or at Christyd@pdrclinics.com
with questions.
PDR Clinic Locations: Edina, Burnsville,
Maplewood, Burnsville, Chanhassen
Specializing in the treatment of chronic neck, back and TMJ pain.