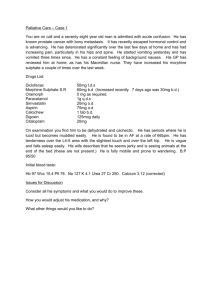
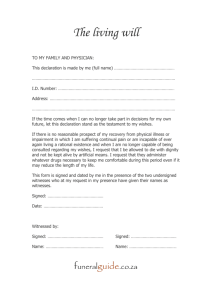
Palliative/ end of life care MOSLER Case: Patient is having confusion and drowsiness, bed bound, only few days left to live, signed DNACPR form. Partner is now here for you to talk about what happen next. Really sorry you are in this situation; it must have put both of you in stress. If it’s alright with you can we have a chat of a form call CPR. Have you heard of CPR by any chance? 1. the patient’s wishes, preferences or fears in relation to their future treatment and care 2. the feelings, beliefs or values that may be influencing the patient’s preferences and decisions 3. the family members, others close to the patient or any legal proxies that the patient would like to be involved in decisions about their care 4. interventions which may be considered or undertaken in an emergency, such as cardiopulmonary resuscitation (CPR), when it may be helpful to make decisions in advance 5. the patient’s preferred place of care (and how this may affect the treatment options available) 6. the patient’s needs for religious, spiritual or other personal support. History taking 1. Identity of the partner (LPA with consent) 2. Partner’s understanding – What do you understand about the px so far? What is your ideas concerns and expectations? What about patient’s ICE. How much do you want to know? 3. Patient’s wishes and fears - Did he clearly expressed anything in the past, his preferred place of care, is his last wishes fulfilled? 4. Patients beliefs 5. Patient’s biopsychosocial (medical needs, social care, patient wishes, spiritual/ cultural needs (chaplain), occupational therapy, mental wellbeing). 6. Does he currently have symptoms, drooling, pain (severity, nature, impact on life, mood), anything changed? 7. Discussion of DNACPR, 8. LPA (the family members, others close to the patient or any legal proxies that the patient would like to be involved in decisions about their care) ADRT etc. 9. the patient’s needs for religious, spiritual or other personal support Speech: Good morning, sir, is it ___. I am Jun, one of the doctors on the ward. I am here this morning to speak about your ___. Before I continue, it would be good for me to know just how much you know about her condition at the moment, do you mind telling me about it? That’s right, his condition has _____, cancer has spread to the brain. Her level of function has been going downhill quite a lot, how do you think she is coping with the pain the last couple of days? Do you feel the current painkiller she is on is working at all? A syrup? We think that it is not working, and we suggest that we start her on a pump. If px say no ask why not? We never do anything to bring about anyone’s death quicker. It’s not our intention. I appreciate that morphine in large doses can make people really drowsy and can potentially affects the lucid episodes she had, that is why I suggest start a low dose and perhaps moving up in small increments, see if can meet a sweet spot where she is pain-free and lucid. Has he ever spoken to you about what is important to her in her last stages of her life? SPIKES 1. Thank you for meeting me today. My name is Dr. So, we are meeting today to discuss how to best manage your ___ condition relating to his cancer. Is this place okay or would you like a side room? Would you like to bring along someone for support? Just to confirm I have the patient’s consent to discuss this with you. 2. I just wanted to start by establishing what you understand about his condition presently? 3. Some people would like to go into detail, other people would prefer to focus on specific points, before I start, I just want to establish what you wanted to discuss and how much detail you would like me to go into? 4. Unfortunately, I have some bad news for you. I am sorry to say ___. 5. Empathy – how do you feel? 6. Plan – When patients are nearing the end of life, there are specific targets for treatment that we try to address pre-emptively. 7. Before we leave her today, I wanted to just summarise what we have discussed and how we are going to manage your husband’s pain control/ other needs that may arise in the coming days or weeks…”. 8. End: I know this is a really difficult conversation, I am so sorry for your husband, thank you so much for having a talk with me. Plan of management Pain To counteract pain, we prescribe medications that sometimes contain morphine. If the patient is unable to take this by mouth, then we can give this by injection or sometimes via a pump to keep on top of pain. One of the side effects of morphine-based painkillers is constipation and so to avoid this we usually prescribe laxatives to keep the bowels regular. Agitation is also common, and we will prescribe medication that can be given in case this occurs. The secondary effect of morphine is that it slows breathing, which can have the effect of hastening death, however, that would not be our prime aim, which is always to alleviate pain. WHO pain ladder Start with non-opioids (paracetamol, NSAIDs, aspirin) If uncontrolled, then try add in opioid for mild to moderate pain such as codeine If still pain, opioids for moderate to severe pain such as morphine or diamorphine) Start low and go slow, laxatives and antiemetics can be given. Adjuvants can be added at all steps include NSAIDs, amitriptyline, pregabalin, steroids, TENS and radiotherapy. Epidural – Neuropathic pain – gabapentin or SSRIs Intestinal colic – hyoscine butylbromide Give enough explanation and reassurance Liaise with the acute pain service I understand that must be very distressing. There are definitely other options we can think about and we do work closely with our palliative care team. One of the option is a pump system, a small needle, deliver medications continuously, we can put different things on that, more consistent painrelief, medications that help with agitation, and also secretions in his mouth. Further I will liaise with the ward sister to allow you to remain by the patient 24 hours a day if wished. Discuss with the Macmillan nurse or the palliative care team to decide on the appropriate dose. The Macmillan team would be available to you who could provide further assistance and support with pain and symptom management in end-of-life care. Agitation I understand that must be really distressing, often when people are very unwell and deteriorating, it can be the way in which things happen which is fluctuating, people can be more alert one second and then drowsy the next, our goal of treatment is to make somebody as comfortable as possible. Scenario How many days? Can she wait, my relative is coming to see her in 2 days Can you not give her the IV morphine, it is making her very drowsy. Response When it comes to the end of life, it is very hard to predict. The morphine can make her drowsy but our concern is that she is in pain. When your brother come, we can try to wean her down a bit, providing that she is not in worst pain. Unfortunately when it comes to end of life, there are no certainties, we can’t predict how long, it may well be that as the disease progress, she will become less responsive, and there won’t be anything we can do about that. The most important thing is we make sure in making him comfortable as much as we can until that point, but I am sorry I can’t provide you a precise answer on that, I think we just have to watch and monitor the situations as time goes by. We never do anything to bring about anyone’s death quicker. It’s not our intention. I appreciate that morphine in large doses can make people really drowsy and can potentially affects the lucid episodes she had, that is why I suggest start a low dose and perhaps moving up in small increments, see if can meet a sweet spot where she is pain-free and lucid. We are dutybound to her to make sure she is painfree. What happen is she okay? As part of approaching the end of life, people can sometimes get agitated, have secretions, get nausea and vomiting, there is other drugs we can put in a pump to manage each of the symptoms individually as they manifest. We will be keeping a very close eye on her, to keep her as comfortable as we possibly can. Is there anything I can do for you at this point? If anything comes to mind, please do get hold of me. Relative gives information You don’t know Patient cry That’s really valuable information, thanks its good to hear your findings in a day to day basis. I will have a discussion with the ____ team to decide on. Take a moment Examiner questions Ethical principles In some cases, it is possible to follow a patient’s wishes given when lucid which considers the principle of autonomy. Other principles are beneficence and nonmaleficence in terms of symptom control. It is important to consider family wishes but our duty is to the patient. When would you discuss a DNAR? Best practice is that it should always be discussed, even if the patient lacks capacity or fails to comprehend the discussion. If the discussion causes harm to the patient, physical, psychological or otherwise, it may be more appropriate to talk to close relatives or next of kin. The final decision lies with the medical team, however, It is important and considerate to hold those discussions. When it comes to discussions at the end of life, it is important if we discussed it earlier. Will it be okay if we discuss it now? Is there anyone you would like to be with you? When we give people a tube to sustain breathing, it is not something that they want, LPA Is there anyone you would like to speak on your behalf, should you lose the capacity to make a decision, it is something called the lasting power of attorney. It can be more than one person Health and welfare – refuse not demand treatment Property and financial affairs Process: 1. choose 2. fill up form 3. register at office of the public guardian DNACPR MDT members Who are involved in the APC discussion – social care Advanced statement of wishes and preferences ADRT A legally binding document about what medical treatment you would not want in the future, if you lack capacity to say so. Limitations - patient cannot specify which treatments they want Examiner questions: Who will receive a copy of these documents? GP Care homes Hospital record Examiner script: History taking: Focus here is: patient’s ICE (last wishes, preferences) partner’s ICE (understanding of patient’s condition and treatment options) End of life symptoms that the patient may have Any previous ADRT, LPA, 4 aspects: physical, psychological, social, spiritual Candidate should: *empathetic is important: avoid saying phrases like “I understand” because you simply do not. Instead say something along the lines of “I can see this news was a huge shock, I am really sorry about that, I can’t imagine what it’s like to feel like that” *encouraging questions is an integral part of advance care planning *in this case the patient has capacity but if you are in doubt assess the patient’s capacity to understand, retain, weigh and communicate his decision to you 1. Explain about the DNAR - it is the medical teams decision - “we feel it would be kinder and more appropriate to ensure he is not in any pain or distress in the last moments of his life. If it were to get to the point where his heart was to stop, we would not try to restart it.” - “your husband will still receive all of the treatment, it is just when he reaches the natural end of his life, we would not do chest compressions and shock to restart it, because this can cause a lot of pain and distress and prolong suffering. - “even if your husband survives, he is often more disabled after and left with a quality of life he would not want” 2. Lifespan: When it comes to the end of life, it can be hard to say, but it can range from days to weeks. Our priority is to make him as comfortable as possible. 3. Management: His care should be a shared decision between his family and the healthcare professional. Pain: it may be neuropathic pain related to his diabetes, ischaemic pain related to peripheral vascular disease and bone pain from osteoporosis. WHO pain ladder for people with stage 5 CKD. Step Paracetamol 1g qds 1 Step Tramadol 50-100mg qds AVOID codeine, dihydrocodeine and 2 dextropropoxyphene Step Moderate pain and outpatient/at home: buprenorphine, oxycodone, 3 hydromorphone or fentanyl. Evidence suggests that fentanyl is the safest drug to use in stage 5 CKD Severe pain and inpatient: Fentanyl (25 mcg starting dose) subcutaneously as required, then in a continuous subcutaneous infusion if necessary. Pruritus: uraemic pruritus: correction of high calcium, parathyroid levels, use emollients liberally if xerosis or antihistamine Tiredness: anaemia due to decrease EPO production, give EPO injections Swollen: fluid overload – avoid salty food and reduce fluid intake, furosemide may be needed Nausea: give anti-emetics 4. MDT Muscle cramps: give antimuscarinic renal supportive and palliative care nurse specialist will be supporting your husband and liaise with GPs and district nurses to best manage his other comorbidities such as diabetes Referral to dietician for nutrition and supplements. His other treatment, if deemed not improving his life or act as burden, some of the medications may be stopped. Social workers or renal counsellors. Bereavement support Spiritual care such as the chaplain Geriatrician coordinate care 5. Advanced care planning - I would like to discuss with you about advance care planning - advanced statement of wishes and preferences: do you and your husband have any wishes and preferences related to his future treatment and care - 5 steps (step 1 think, step 2 talk with family and friends, step 3 write it down, step 4 discuss with GP step 5 share) - which he would not want to happen? (such as a feeding tube, antibiotics, artificial organ support, IV fluids, blood transfusions that was mentioned previously) ADRT EHCP (emergency health care plan) 6. Summarise: so today we have went through both you and your husbands thoughts and preferences to treatment, some symptoms he was having and have a discussion and come together with a plan on how best to manage his condition. Do you have any questions? In case you do have any now and then, I’ll give you our contact details with some leaflets with further information. I know this is a really difficult conversation, I am so sorry for your husband, thank you so much for having a talk with me. Should you require any spiritual and psychological support please let us know Questions for candidate: 1. Should the patient still have mental capacity and 1-2 years predicted lifespan, do you know the name of a particular legal document that lets the patient to appoint one or more people to help them make decisions on their behalf? Lasting power of attorney (LPA) 2 types: health and welfare / property and financial affairs Health and welfare o make decisions on daily routine such as washing, dressing, eating o medical care o moving into a care home o life-sustaining treatment property and financial affairs o selling home o managing bank account Register with the office of the public guardian Cost 82 pounds 2. What are the symptoms people experienced in the end of life? Divided into CNS: delirium confusion agitation drowsiness GI: nausea and vomiting, constipation Respiratory: SOB, Cheyne-stokes breathing, terminal secretions GU: incontinence Skin: mottled Pain 3. do you know any signs that are suggestive of patient entering last stages of his life Agitation Cheyne-stokes breathing Deterioration in level of consciousness Mottled skin Noisy respiratory secretions (terminal rattle) Progressive weight loss Increased fatigue and loss of apetite Social withdrawal Deteriorating mobility status 4. Can you tell me the medical management of a patient in end of life or palliative care setting? Pain Depending on the cause and follow the WHO pain ladder: 1. Cancer – morphine gold standard 2. colic pain – anticholinergic such as hyoscine butylbromide 3. muscular pain or spasm – benzodiazepines 4. neuropathic – amitriptyline Breathlessness Oxygen if hypoxic Morphine N&V Metoclopramide or haloperidol Agitation Midazolam or haloperidol Terminal Hyoscine butylbromide secretions Constipation Lactulose or senna Regular monitoring every 24 hours 5. Can this patient be allowed to die at home? Tell the partner that you will discuss the possibility of moving the patient to a nursing home or his house. It is usually feasible with community palliative care/ Macmillan nurse visiting every day to help administer his medication and make sure he is comfortable. Health care support worker and social worker can also pop in to help with the housing such as cleaning, food, grocery shopping if she requires it. 6. when would it not suitable for the patient to be allowed to die at home? Where the patient abruptly withdraw from dialysis Stage of CKD is end stage 7. what are the indications to initiate a DNAR discussion? Indications Terminal diagnosis Frailty Hospital discharge (before or after) Increase in level of care/ deterioration in condition Patient request Best practice is that it should always be discussed, even if the patient lacks capacity or fails to comprehend the discussion. If the discussion causes harm to the patient, physical, psychological or otherwise, it may be more appropriate to talk to close relatives or next of kin. The final decision lies with the medical team, however, It is important and considerate to hold those discussions. 8. let’s say this patient had a terminal cancer diagnosis, do you know any functional assessment tool to assess their performance? (one of the ACE tutorial) o Karnovsky score where a score of <50 means lower survival o Barthel index which is typically use in stroke o Nottingham Extended ADL scale focus on social participation such as driving 9. What help can a gp provide to this patient’s wife should he passaway? (bereavement tutorial) be someone to talk to help normalise what the person is going through e.g. thinking they are seeing or hearing their loved one, feeling of relief after long illness be able to help answer questions the family may have about the death encourage a healthy lifestyle e.g. eating well, avoid excess alcohol, exercise check in on the person in a few weeks to make sure they are doing okay offer suggestions for ways to help manage problems such as difficulty sleeping or feeling anxious/panicky sleeping tablets can be used in the short term (start with around 4 days and no more than 4 weeks) to help people who are struggling sleep direct people to appropriate resources e.g. NHS inform help people access bereavement counselling if this would be beneficial practical things such as providing a fit note for work to give the person time and space to grieve http://www.gmc-uk.org/End_of_life.pdf_32486688.pdf https://www.nice.org.uk/guidance/ng31 https://www.goldstandardsframework.org.uk/cdcontent/uploads/files/General%20Files/Prognostic%20Indicator%20Guidance%20October%202 011.pdf MLE tutorial