Opioid and non-opioid analgesics: pharmacology and clinical
advertisement

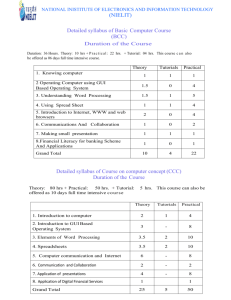
Palliative Care Dr Philip Lee Senior Staff Specialist Palliative Medicine Westmead Hospital Palliative Care Definitions To cure, occasionally To relieve, often To comfort, always Anonymous (16th Century) Death should simply become a discreet but dignified exit of a peaceful person from a helpful society … without pain or suffering and ultimately without fear. Philippe Ariès, 1977 The Hour of Our Death Palliative Care provides for all the medical and nursing needs of the patient for whom cure is not possible and for all the psychological, social and spiritual needs of the patient and the family, for the duration of the patient’s illness, including bereavement care. Roger Woodruff Palliative Medicine 2nd Edition Palliative Care Caring for a person with an active, progressive, far advanced disease with little or no prospect of cure and for whom the primary treatment goal is quality of life PALLIATIVE CARE - WHEN? ACTIVE TREATMENT PALLIATIVE CARE BEREAVEMENT ACTIVE TREATMENT BEREAVEMENT PALLIATIVE CARE PALLIATIVE CARE - WHERE? Palliative Care is a Network Services are provided by Teams Services are available in: Community, home and aged care facilities Acute hospitals Private Hospitals Specific inpatient units eg St Joseph’s, Mt Druitt, Neringah, Greenwich, Braeside Hospitals PALLIATIVE CARE - COMMUNITY GP “case manager” Generalist Community Nurse - GCN Clinical Nurse Specialist - CNS Clinical Nurse Consultant - CNC Palliative Care Medical Officer Community Palliative Care Specialist WHAT DOES PALLIATIVE CARE OFFER? Pain control Other symptom control Terminal care Family support Bereavement support Cancer pain 30-50% of cancer patients undergoing active treatment 70-90% of cancer patients with advanced disease Prospective studies indicate that as many as 90% of patients could attain adequate pain relief with simple drug therapies. The Context Symptoms of debility Non-cancer pathology Side effects of therapy Cancer Loss of social position Loss of job prestige and income SOMATIC SOURCE Friends not visiting Loss of role in family Chronic fatigue and insomnia Bureaucratic bungling DEPRESSION TOTAL PAIN ANGER Unavailable doctors Sense of helplessness ANXIETY Disfigurement Fear of hospital or nursing home Worry about family Fear of death Spiritual (existential) unrest Delays in diagnosis Fear of pain Family finances Loss of choices Uncertainty about future Irritability Therapeutic failure WHO analgesic ladder Pain Pain persists or increases Pain persists or increases 3. 2. 1. Non-opioid ± adjuvant Weak opioid ± non-opioid ± adjuvant Strong opioid ± non-opioid ± adjuvant Guidelines for opioid use Preferably oral Continuous rather than PRN Commence with immediate release Once stable convert to slow release + immediate for breakthrough pain relief If more than 2 episodes of breakthrough pain increase regular dose Laxatives Analgesic Classes Aspirin Paracetamol NSAIDS Opioids Opioids Weak opioids Codeine Dextropropoxyphene Tramadol Strong opioids Oxycodone Morphine Methadone Fentanyl Hydromorphone Opioid receptors All opioids produce analgesia and other effects by mimicking the actions of endogenous opioid compounds (endorphins) at multiple subtypes of the three major opioid receptors in the brain stem, spinal cord and peripheral tissues. Opioid actions The perception of pain is altered both by a direct effect on the spinal cord, modulating peripheral nociceptive input, and by activation of the descending inhibitory systems from the brain stem and basal ganglia. Patients’ concerns about narcotics Addiction & withdrawal Tolerance Implications of taking morphine Side effects Side effects Sedation Hallucinations Nausea & vomiting Constipation Urinary retention Myoclonus Respiratory depression Pruritus Cognitive impairment Some sedation early in use of morphine Tolerance develops Prior sleep deprivation due to poor pain control Other causes of cognitive impairment need to be excluded Opioid Dose Duration of Action Morphine (oral) 20 mg 4 hrs Morphine (parenteral) 10mg 4 hrs Codeine 130 mg 4-6 hrs Pethidine (IMI) 80 mg 2-3.5 hrs Methadone * 2-5 mg 8-12 hrs 10-20 mg 4 hrs Tramadol 200 mg 4-6 hrs Fentanyl 200 mcg 1-2 hrs 4 mg 4 hrs Oxycodone Hydromorphone Routes of administration of morphine Oral Subcutaneous IVI Epidural & intrathecal Rectal Topically Morphine metabolism Primarily metabolised in the liver Metabolites excreted in urine Morphine-3-glucuronide (M3G) Morphine-6-glucuronide (M6G) Caution in renal impairment M6G potent morphine agonist M3G no significant analgesic action Liver disease not reported to alter pharmacokinetics Morphine Pros “Gold Standard” Well understood Readily available Usually well tolerated No “ceiling” Cons Accumulates in renal failure Constipating Nausea Sedation Misconceptions Morphine Preparations Morphine mixture (Ordine) 4 hrs 1, 2, 5, 10, 20, 40 mg/ml Kapanol caps 24 hrs 10, 20, 50, 100 mg/ml MS Contin tabs 12 hrs 5, 10, 15, 30, 60, 100, 200 mgs MS Contin susp 12 hrs 30, 60, 100, 200 mgs MS Mono caps 24 hrs 30, 60, 90, 120 mgs Morphine sulphate amps 4 hrs 5, 10, 15, 30, 50 mgs/ml Morphine tartrate amps 4 hrs 120 mgs/1.5 mls, 400mgs/5mls Oxycodone Pros Various dose forms, immeadiate & slow release Neuropathic pain “New” OK in renal failure Cons Constipating Nausea Confusing names Oxycodone & Tramadol Endone Tabs 4 hrs 5 mg Oxynorm 4 hrs 5, 10, 20 mgs Oxycontin 12 hrs 5, 10, 15, 20, 30, 40, 80 mgs Tramadol caps 4-6 hrs 50 mg Tramadol SR Tabs 12 hrs 100, 150, 200 mgs Tramadol amps 4-6 hrs 100 mg/2 mls Fentanyl Pros Less constipation Less nausea Less psychotomimetic effects Convenient OK in renal failure Cons Reliant on good fat stores Inflexible dosing Difficult to titrate Expensive Breakthrough medications Hydromorphone Pros Less sedating Less constipating Less hallucinations Less nauseating OK in renal failure Cons Availability Methadone Pros Neuropathic pain Cons Stigma Difficult dosing schedule Variable half-life Fentanyl, Methadone & Hydromorphone Fentanyl Patches (Durogesic) 72 hrs 25, 50, 75, 100 mcg/hr Fentanyl sublingual liquid 1-2 hrs 100 mcg/ml Fentanyl lozenges (ACTIQ) 1-2 hrs 200, 400, 800, 1200, 1600 mcg Methadone 8-100 hrs 10 mg Hydromorphone tabs (Dilaudid) 4 hrs 2, 4, 8 mgs Hydromorphone liquid 4 hrs 1 mg/ml Hydromorphone Extended Release (Jurnista) 24 hrs 8, 16, 32, 64mgs Hydromorphone amps 4 hrs 2mg/ml, 10mg/ml, 50mg/5mls, 500mg/50mls Pethidine Repetitive dosing leads to accumulation of the toxic metabolite norpethidine Norpethidine accumulation causes CNS hyper-excitability & subtle mood changes Tremors Multifocal myoclonus Seizures Common with repeated large doses, eg 250 mg per day